Relationship between self-efficacy and adherence to antiretroviral therapy in HIV/AIDS patients: An analytical cross-sectional study in southern Iran
Abstract
Background and Aims
The human immunodeficiency virus (HIV) infection, also known as acquired immunodeficiency syndrome (AIDS), is spreading rapidly in the world, especially in developing countries, and is considered a serious health threat. This study aimed to assess the relationship of adherence antiretroviral therapy (ART) and self-efficacy among people living with HIV.
Methods
This cross-sectional study was conducted in March–July 2022 at the Center for Behavioral Diseases in Bandar Abbas. A total number of 208 HIV patients treated with ART entered the study after voluntarily signing an informed letter of consent. The data collection instrument was the adherence to ART questionnaire with the six subscales and the General Self-Efficacy Scale-17 (GSE-17) general self-efficacy questionnaire. Multivariate regression analysis was used to test the relationship among the variables.
Results
The participants' mean age was 41.7 ± 8.2 years. Self-efficacy was positively correlated with adherence ART. With every one score of increased self-efficacy, MA increased for 0.85 score (p < 0.001) and medical challenges have the strongest correlation (r = 0.27) with self-efficacy. The multivariable regression analysis showed that moderate and high socioeconomic status (SES) each improved MA for 18 and 22 units, respectively, compared to poor SES. Alcohol consumption reduced MA for 11 units.
Conclusion
This study proved the positive relationship of self-efficacy in adherence to ART in HIV patients. The insights offered by this research can help develop a systematic and effective intervention to promote MA in HIV patients. SES and alcohol consumption significantly affect MA.
1 INTRODUCTION
Human immunodeficiency virus (HIV) remains to be a major global health threat, and as reported by the World Health Organization (WHO), 40.4 million people have died due to this disease so far. In 2022, 630,000 people died from HIV-related causes and 1.3 million people were infected with HIV.1 HIV infection is spreading rapidly in the world, especially in developing countries,2 which is considered a health threat, especially in these countries.3 As reported by Iran National HIV Registration System, the total population infected with HIV by the end of 2018 was 38,966, the majority of whom were male (83%). Their age group was 16–40 years (67.6%). The infected population by the end of 2018 was 15,845 cases infected with HIV having died for some reason.4
Acquired immunodeficiency syndrome (AIDS) is not only one of the most devastating diseases of the present time but also a social phenomenon that has affected various aspects of life.5 Although AIDS is in its third decade of prevalence, compared to other medical and social issues, it is considered a complex and unique concern. From the medical point of view, this disease is a long and fatal disease destroying the body's immune system and leading to death. It brings about a slow death2 and is stigmatized in society. It, in fact, lowers the social dignity,6 which significantly affects the therapeutic procedure for those infected.
Medication adherence (MA) is key to the achievement of the desired therapeutic outcomes in HIV. To improve the quality of life of HIV patients and reduce the resultant mortality, the desired adherence should be at least 95%.7 Despite the availability of effective antiretroviral therapy (ART), poor MA is the main cause of treatment failure.8
MA is defined by WHO as the extent to which the patient follows medical instructions.9 It involves the initiation of treatment, implementation, and continuation with the recommended dose.10 ART is crucial for a successful HIV treatment, as it has dramatically reduced viral transmission, disease progression, and mortality among HIV patients.11, 12
However, in Iran, it was estimated that only 20% of HIV patients were adherent to ART.4 Studies have shown that poor adherence to medication in low- and middle-income countries is influenced by a lack of knowledge, negative attitudes, and negative beliefs.13, 14
Studies showed that one factor affecting MA of HIV patients is one's self-efficacy (SE) in MA. In other words, self-efficacy can act as a mediator to improve HIV patients' MA.15, 16 According to the socio-cognitive theory, individuals with higher self-efficacy to perform health-promoting behaviors are more likely to show this behavior.17, 18
The effect of self-efficacy is highlighted due to the continuous process of adherence to ART, which begins when the patient begins taking medicine and continues all throughout his/her life. Despite the fact that most patients are aware of the importance of medical therapy in improving their quality of life and increasing their life expectancy, the MA in these patients is not at an optimal level, and as mentioned in Iran, the level of MA is far from optimal.4, 19 Bandar Abbas, the largest commercial port in Iran, located in Hormoz Strait adjacent to the Persian Gulf countries, accepts many immigrants from different parts of Iran and other countries for various commercial and industrial jobs.20 In this region, there is a high rate of risky behaviors.21 Also, the number of HIV/AIDS patients is high compared to other provinces.22 This study aimed to explore the adherence to HIV/AIDS medication (and the subscales including personal barriers, medication challenges, service delivery quality, financial problems, perceived support, and disease disclosure). Then the relationship between MA and self-efficacy and demographic variables was explored in southern Iran.
1.1 Methodology
The present cross-sectional study was conducted in March–July 2022 at the Behavioral Diseases Center of Bandar Abbas city, in central Hormozgan province. The participants were supposed to have a history of ART for at least a year. Those with incomplete questionnaires or unwilling to continue with the study were excluded.
1.2 Sampling
The research population was HIV patients visiting the Center for Behavioral Diseases in Bandar Abbas. All patients visiting the Center for Behavioral Diseases were invited to participate in the study, and finally, 208 patients signed the informed consent form and entered the study voluntarily. The response rate was 83.87.
1.3 Data collection
Having gained the required permissions, the present researchers visited the Center for Behavioral Diseases. Due to the sensitive nature of the disease and to preserve the confidentiality of data, two staff members of the Center for Behavioral Diseases were invited to cooperate with the researchers. Having provided an informed letter of consent to participate in the research, the data collection began. The participants could choose between a hard-copy or soft-copy questionnaire to complete. All the questionnaires were completed in the presence of the researcher. If the participant was illiterate, the researcher read the questions aloud and jotted down the exact answer for the respondent.
1.4 Adherence to ART questionnaire
The adherence to ART questionnaire included two parts: demographic information and MA information.23
The first part enquired about age, gender, marital status, educational level, occupation, socioeconomic status (SES), cigarette smoking, hookah smoking, drug addiction, alcohol consumption, Imprisonment, duration of treatment, and place of residence.
The second part was related to MA and consisted of six subscales: personal barriers, medication challenges, service delivery quality, financial problems, perceived support, and disease disclosure. The questionnaire was rated on a 5-point Likert-type scale ranging from very high to no effect. The sections of personal barriers, medication challenges, quality of service delivery, financial problems, perceived support, and disease disclosure included, respectively, eight items (range of 8–40), six items (range of 6–30), six items (range of 6–30), two items (range of 2–10), four items (range of 4–20), and four items (range of 4–20). Validity and reliability of the questionnaire were previously substantiated.
The qualitative and quantitative content validation was done by a panel of 10 experts (professors in health education and promotion, infection specialists, and instructors of nursing and instrumentation). To this aim, CVI (Content Validity Index) and CVR (Content Validity Ratio) were estimated. The results showed that all items received a score above 0.79.
Cronbach's α was estimated at 0.91 for the overall questionnaire and ranged between 0.7 and 0.88 for the subscales. The test–retest method was used to check the reliability of the overall questionnaire, which was estimated at 0.80. For the subscales, it ranged between 0.57 and 0.75, which supports the consistency of scores obtained from the questionnaire.23
1.5 General Self-Efficacy Scale-17 (GSE-17)
GSE-17 was developed by Sherer and Adams,24 and its reliability and validity were substantiated in Iran.25 This scale measured general self-efficacy with 17 items. The reliability of this instrument was tested using Cronbach's α and was found to be 0.86.26 This questionnaire was rated on a 5-point Likert-type scale ranging from strongly disagree to strongly agree. Items 1, 3, 8, 9, 13, and 15 were reverse-scored.
1.6 Ethical considerations
This research was approved by the committee of ethics at Hormozgan University of Medical Sciences (#IR.HUMS.REC.1400.090). All participants signed an informed letter of consent. The content included all details of the study. The participants were asked to take part in the study voluntarily. The questionnaire completion was anonymous, and all participants were assured of the confidentiality of information they provided.
1.7 Statistical analysis
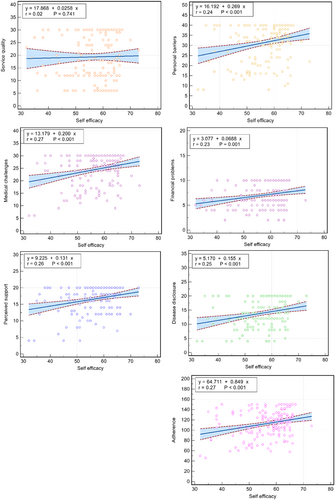
To describe the demographic variables (age, sex, marital status, educational level, occupation, SES, cigarette smoking, hookah smoking, drug addiction, alcohol consumption, imprisonment, duration of treatment, and place of residence) as categorical categories, frequency, and percentage were used. Mean and standard deviation were used to describe noncategorical variables (i.e., self-efficacy and MA). T test was used to check the difference in the score of the two noncategorical dependent variables of self-efficacy and MA at different levels of two-level demographic variables. One-way analysis of variance was used for three-level (or more) demographic variables. To describe self-efficacy and MA and the subscales, mean, maximum, and minimum scores were used. The percentage of the obtained score was also calculated by dividing the average score by the total score that could be obtained. Univariable and multivariable linear regression analyses were used to investigate the demographic factors affecting MA. To test the relationship between self-efficacy and sub-scales of MA, a scatter plot was drawn using the correlation coefficient. To draw the graph, MedCalc 18 was used and the data were analyzed in STATA 14.2 at a significance level of <0.05.
2 RESULTS
A total number of 208 participants with an average age of 41.65 ± 8.166 took part in this study. They were mostly (59.6%) within the age range of 41–61 years. Moreover, 57.2% of the participants were female. About half of them (51%) were married and 51.9% were unemployed. The most common way of transmitting HIV was through sex affair with the spouse (43.3). Other detailed demographic variables are summarized in Table 1.
| Variable | Quantity (%) | Self-efficacy | MA | ||
|---|---|---|---|---|---|
| Mean SE | SE p value | Mean MA | MA p value | ||
| Age | |||||
| 20–40 | 84 (40.4) | 56.70 ± 8.67 | 0.777 | 111.53 ± 26.20 | 0.592 |
| 41–61 | 124 (59.6) | 56.37 ± 7.96 | 113.49 ± 25.52 | ||
| Gender | |||||
| Male | 89 (42.8) | 57.00 ± 6.97 | 0.455 | 111.86 ± 25.59 | 0.686 |
| Female | 119 (57.2) | 56.13 ± 9.08 | 113.33 ± 25.97 | ||
| Marital status | |||||
| Single | 102 (49) | 55.07 ± 8.78 | 0.013 | 109.65 ± 26.65 | 0.093 |
| Married | 106 (51.0) | 57.89 ± 7.46 | 115.64 ± 24.63 | ||
| Educational level | |||||
| Primary school | 109 (52.4) | 54.73 ± 8.89 | 0.007 | 109.93 ± 29.81 | 0.189 |
| Secondary school | 50 (24.0) | 57.60 ± 6.96 | 112.64 ± 21.82 | ||
| Diploma | 37 (17.8) | 58.95 ± 7.37 | 117.22 ± 18.08 | ||
| University | 12 (5.8) | 60.50 ± 5.82 | 124.17 ± 16.68 | ||
| Occupation | |||||
| Employee | 12 (5.8) | 61.00 ± 2.95 | 0.048 | 124.25 ± 10.89 | 0.048 |
| Freelancer | 70 (33.7) | 57.81 ± 7.22 | 113.80 ± 22.20 | ||
| Unemployed | 108 (51.9) | 55.31 ± 8.97 | 108.95 ± 28.03 | ||
| Other | 18 (8.7) | 55.56 ± 8.42 | 123.22 ± 27.34 | ||
| SES | |||||
| Low | 119 (57.2) | 54.24 ± 8.84 | <0.001 | 105.42 ± 27.14 | <0.001 |
| Medium | 76 (36.5) | 59.25 ± 6.49 | 122.93 ± 19.67 | ||
| High | 13 (6.3) | 61.23 ± 3.85 | 119.54 ± 23.21 | ||
| Cigarette smoking | |||||
| No | 153 (73.6) | 57.16 ± 7.86 | 0.054 | 115.84 ± 24.54 | 0.003 |
| Yes | 55 (26.4) | 54.67 ± 9.02 | 103.96 ± 27.25 | ||
| Hookah smoking | |||||
| No | 148 (71.2) | 57.34 ± 7.73 | 0.022 | 115.47 ± 24.41 | 0.015 |
| Yes | 60 (28.8) | 54.45 ± 9.11 | 105.88 ± 27.85 | ||
| Drug addiction | |||||
| No | 183 (88.0) | 56.84 ± 7.87 | 0.117 | 114.11 ± 24.60 | 0.033 |
| Yes | 25 (12.0) | 54.08 ± 10.44 | 102.40 ± 31.74 | ||
| Alcohol consumption | |||||
| No | 172 (82.7) | 56.96 ± 8.30 | 0.082 | 115.59 ± 24.36 | <0.001 |
| Yes | 36 (17.3) | 54.33 ± 7.68 | 98.92 ± 28.07 | ||
| Imprisonment | |||||
| No | 143 (68.8) | 57.41 ± 8.20 | 0.018 | 116.07 ± 24.58 | 0.005 |
| Yes | 65 (31.3) | 54.51 ± 8.03 | 105.29 ± 26.91 | ||
| Duration of treatment | |||||
| 1–5 | 102 (49.0) | 56.35 ± 8.01 | 0.352 | 112.82 ± 27.33 | 0.169 |
| 6–10 | 77 (37.0) | 57.35 ± 8.26 | 115.48 ± 21.80 | ||
| 11–20 | 29 (13.9) | 54.79 ± 8.92 | 104.90 ± 28.88 | ||
| Place of residence | |||||
| Urban | 164 (78.8) | 56.15 ± 8.42 | 0.226 | 112.15 ± 26.28 | 0.549 |
| Rural | 44 (21.2) | 57.84 ± 7.43 | 114.77 ± 23.85 | ||
- Abbreviations: MA, medication adherence; SE, standard error; SES, socioeconomic status.
The T test results of the relationship of variables with self-efficacy and MA showed that self-efficacy was correlated with marriage, level of education, occupation, SES, hookah consumption, and history of imprisonment. MA was also correlated with drug abuse. Drug addicts showed less MA, and this relationship is also significant with cigarette smoking, hookah smoking, alcohol consumption, occupation, history of imprisonment, and SES.
The division of the mean score of self-efficacy and adherence dimensions showed the participants' highest score was that of perceived support (83%) and the lowest was that of service quality (64%). Also, on average, the participants obtained 66.47% of the attainable score of self-efficacy (Table 2).
| Mean | Standard deviation | Percentage mean of score | Maximum | Minimum | |
|---|---|---|---|---|---|
| SE | 56.5 | 8.24 | 66.47 | 73 | 32 |
| Personal barriers | 31.40 | 9.17 | 78.50 | 40 | 8 |
| Medical challenges | 24.47 | 6.09 | 81.57 | 30 | 6 |
| Service quality | 19.33 | 9.24 | 64.43 | 30 | 6 |
| Financial problems | 6.97 | 2.41 | 69.70 | 10 | 2 |
| Perceived support | 16.60 | 4.10 | 83.00 | 20 | 4 |
| Disease disclosure | 13.94 | 5.19 | 69.70 | 20 | 4 |
| Total MA | 112.70 | 25.75 | 75.13 | 150 | 46 |
- Abbreviations: MA, medication adherence; SE, standard error.
Univariate regression analysis showed that SES, cigarette smoking, hookah smoking, drug addiction, alcohol consumption, and history of imprisonment are related to MA. The results of multivariable regression analysis showed that moderate and high economic status improved MA for 18 and 22 units, respectively, compared to poor SES. Also, alcohol consumption reduced MA for 11 units (Table 3).
| Variable | Univariable | Multivariable | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| aB | 95% CI | bβ | p Value | aB | 95% CI | bβ | p Value | |||
| Age | ||||||||||
| 41–61 | 1.96 | −5.23 | 9.14 | 0.04 | 0.592 | −0.1 | −8.18 | 7.98 | −0.04 | 0.981 |
| Gender | ||||||||||
| Female | 1.46 | −5.67 | 8.59 | 0.03 | 0.686 | −11.46 | −24.22 | 1.30 | 0.08 | 0.078 |
| Marital status | ||||||||||
| Married | 5.99 | 1.02 | −13.01 | −0.12 | 0.093 | −0.63 | −8.31 | 7.06 | −0.17 | 0.872 |
| Educational level | ||||||||||
| Secondary school | 2.7 | −5.93 | 11.34 | 0.04 | 0.538 | −0.76 | −9.14 | 7.63 | −0.08 | 0.859 |
| Diploma | 7.28 | −2.34 | 16.9 | 0.11 | 0.137 | −2.17 | −12.09 | 7.75 | 0.01 | 0.667 |
| University | 14.23 | −1.15 | 29.61 | 0.13 | 0.07 | −5.5 | −24.36 | 13.36 | −0.1 | 0.566 |
| Occupation | ||||||||||
| Freelancer | −10.45 | −26.13 | 5.23 | −0.19 | 0.190 | −0.52 | −18.65 | 17.61 | −0.06 | 0.955 |
| Unemployed | −15.30 | −30.56 | −0.03 | −0.30 | 0.050 | −3.60 | −21.97 | 14.76 | −0.002 | 0.699 |
| Other | −1.03 | −19.73 | 17.67 | −0.01 | 0.914 | 14.23 | −7.24 | 35.69 | −0.22 | 0.193 |
| SES | ||||||||||
| Medium | 17.51 | 10.44 | 24.59 | −0.33 | <0.001 | 18.13 | 10.01 | 26.24 | −0.01 | <0.001 |
| High | 14.12 | 0.04 | 28.19 | −0.13 | 0.049 | 22.09 | 4.90 | 39.27 | −0.01 | 0.012 |
| Cigarette smoking | ||||||||||
| Yes | −11.88 | −19.71 | −4.04 | −0.2 | 0.003 | −2.76 | −13.77 | 8.25 | −0.07 | 0.621 |
| Hookah smoking | ||||||||||
| Yes | −9.58 | −17.26 | −1.90 | −0.17 | 0.015 | −2.20 | −10.54 | 6.15 | 0.16 | 0.604 |
| Drug addiction | ||||||||||
| Yes | −11.71 | −22.44 | 0.98− | −0.15 | 0.033 | 6.79 | −6.72 | 20.31 | 0.34 | 0.323 |
| Alcohol consumption | ||||||||||
| Yes | −16.67 | −25.71 | −7.63 | −0.24 | <0.001 | −11.56 | −22.85 | −0.27 | 0.21 | 0.045 |
| Imprisonment | ||||||||||
| Yes | −10.78 | −18.25 | −3.31 | −0.19 | 0.005 | −4.45 | −17.04 | 8.14 | −0.33 | 0.486 |
| Duration of treatment | ||||||||||
| June 10 | 2.66 | −4.98 | 10.29 | −0.05 | 0. 494 | 0.74 | −7.15 | 8.63 | −0.17 | 0.853 |
| November 20 | −7.93 | −18.57 | 2.72 | 0.11 | 0.144 | −7.31 | −18.53 | 3.91 | −0.17 | 0.201 |
| Place of residence | ||||||||||
| Rural | 2.63 | −6.01 | 11.26 | 0.04 | 0.549 | −3.66 | −12.96 | 5.63 | −0.05 | 0.438 |
- Abbreviations: CI, confidence interval; SES, socioeconomic status.
- a Unstandardized regression coefficient.
- b Standardized regression coefficient.
Concerning the relationship between self-efficacy and MA, Figure 1 shows any one score of increase in self-efficacy was followed by an increase in the score of MA for 0.85 score (p < 0.001). The strongest positive correlation (r = 0.27) was observed in the medical challenges subscale.
3 DISCUSSION
This study aimed to explore the state of adherence to ART and its relationship with self-efficacy and demographic variables. As the results of the study showed, self-efficacy had a significant positive correlation with MA. Also, there was a significant relationship between SES and alcohol consumption with MA.
The present findings showed that higher self-efficacy leads to greater MA. Bandura described self-efficacy as an individual's belief in his/her ability to show a certain behavior.27 In this study, patients who had higher self-efficacy showed better MA and were able to overcome barriers to adherence. Likewise, a body of research also confirmed that self-efficacy affects MA in HIV patients.15, 28, 29 In their study, Mi et al. contended that disclosing information to family members mediated by social support and self-efficacy significantly and indirectly affects medication adherence.15 Arguably, those enjoying adequate self-efficacy have reached a stable condition. As they have accepted their disease, they can get along with it better and enjoy a better mental health. Therefore, it is less likely that they stop taking medication to solve their problem. Navarra et al. contended that those who had hope for positive outcomes or believed in the potential positive outcome, which is strongly a matter of self-efficacy, were more likely to be completely adherent to medication and more likely to attend all doctor's visits.30
As the findings showed, higher SES was related to greater adherence, in other words, patients with higher SES could have better adherence to medication. Other studies also addressed the relationship between SES and medication adherence.31, 32 Fernandez et al., in some research on homeless women, found that accommodation (housing), stability, and relationships affect women's adherence to medication and involvement in care. Difficulty adhering to medication, routine disruption, interrupted access to medication and health care disruptions, privacy issues with cohabitants, and competing physical and mental health concerns among women in unstable housing conditions were reported as significant barriers to medication adherence.31 It can be argued that for MA, a main principle for patients is to reach an economic stability, and after being sure of this stable condition, the patient is prepared for the treatment stage. Another study suggested that greater life instability among HIV patients could lead to poor health outcomes (in case of HIV disease) over and above the effects of depression, anxiety, and drug abuse.33 Therefore, efforts to provide shelter for patients and reduce therapeutic costs, including health subsidies, as well as to shorten the waiting time to use the services provided by social welfare institutions can be effective in removing financial barriers to MA.
The present findings showed MA decreases with alcohol consumption. The results of another study by Duko et al. showed the prevalence of alcohol consumption among HIV patients is higher than the general population, and recommended screening and appropriate management of alcohol consumption.34 The results of a meta-analysis among HIV patients in sub-Saharan Africa showed that alcohol consumption was associated with reduced adherence to ART, potentially impeding the achievement of HIV therapeutic goals.35 In chronic diseases such as HIV/AIDS, patients may use alcohol as a way to deal with depression and mental problems caused by the severity of disease and the side effects of antiretroviral medication.
The main limitation of this study was the low participation rate because of the existing sociocultural sensitivities of the disease. It was harder to attract these patients' attention and persuade them to participate in the study. Therefore, our results may not be generalizable to the wider population of people living with HIV/AIDS in Iran. To remove this limitation, experts at the Center for Behavioral Diseases gained patients' trust by visiting the center with a wide range of barriers.
In addition, the sample size was moderate, which limits the power to detect minute differences. For this reason, the sampling was a census. All HIV/AIDS patients receiving healthcare services visiting the behavioral diseases center of Bandar Abbas city were included in the study. Although self-reported adherence is a widely accepted approach in assessing adherence to ART, the low concordance of self-reported adherence with adherence to the number of pills suggests a bias toward higher reported MA due to the social desirability of responses.36 The patients trusted the experts at the center. Thus, they answered the questions honestly, and objective measures, such as pill counts, are routinely taken in the Center for Behavioral Diseases as MA monitoring. Also, all participants were assured of the confidentiality of the information they provided. Also, this study only included participants attending outpatient clinics, who were less likely to have a severe disease compared to inpatients, and this may have biased the results toward higher MA. For this reason, a longer period of data collection was followed. If a patient is in hospital, after discharge, s/he can enter the study by visiting the behavioral disease center. The design of study was cross-sectional and correlational. Therefore, no causal inferences can be made about the relationships between these variables.
4 CONCLUSION
This study proved the positive relationship of self-efficacy in adherence to ART in HIV/AIDS patients. The knowledge provided by this research can help develop a systematic and effective intervention to facilitate MA of HIV patients. In addition, a focus on demographic variables such as SES and alcohol consumption can be effective in dealing with barriers to MA.
AUTHOR CONTRIBUTIONS
Zahra Hosseini: Data curation; methodology. Roghayeh Ezati Rad: Data curation; writing—review and editing. Nahid Shahabi: Conceptualization; methodology; writing—original draft. Shokrollah Mohseni: Formal analysis; validation; writing—review and editing. Mehdi Hassani Azad: Writing—review and editing. Teamur Aghamolaei: Writing—review and editing. Abdoulhossain Madani: Writing—review and editing.
ACKNOWLEDGMENTS
The authors thank the Hormozgan University of Medical Sciences as funder and participants taking part in the study. This work was supported by the Hormozgan University of Medical Sciences under Grant HUMS: 4000016. The funding body (HUMS) did not have any role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS STATEMENT
All methods were performed in accordance with the Declaration of Helsinki. This study was approved by the ethics committee of Hormozgan University of Medical Sciences (Code: IR.HUMS.REC.1400.090). All participants provided written consent to participation.
TRANSPARENCY STATEMENT
The lead author Nahid Shahabi affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




