Investigating salivary concentration of calcium ion in hypothyroidism
Abstract
Background and Aims
Hypothyroidism is the most common disease of the thyroid gland. Thyroid hormone plays a crucial role in regulating tissue growth and metabolism. Additionally, patients with thyroid dysfunction have a higher incidence of caries and periodontal problems. The presence of calcium and phosphate ions seems to be effective in remineralizing teeth and reducing caries. The aim of this study was to evaluate the salivary level of calcium in patients with hypothyroidism.
Results
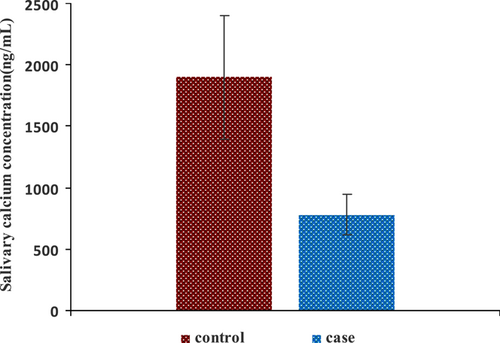
The results of this study showed that saliva calcium concentration in patients with hypothyroidism is significantly lower than healthy subjects. Also, no significant association was found between salivary calcium levels and TSH and T4 hormones level of blood.
Conclusion
The increased prevalence of dental caries in patients with hypothyroidism may be related to a decrease in their calcium levels.
1 INTRODUCTION
Hypothyroidism is the most common thyroid disease that is more common in females than males and results in decreased production of thyroxine (T4), triiodothyronine (T3), and calcitonin. This disorder can be caused by autoimmune disorders, radiotherapy, or thyroid resection, and so forth.1-5 Thyroid dysfunction affects various systems of human body. Thyroid hormone effectively regulates tissue growth and metabolism, and hypothyroidism reduces bone metabolism and maturation and has a negative effect on the bone homeostasis.2, 3, 6 Caries and periodontal disease are more common in patients with thyroid dysfunction and can be a result of disease itself or surgical treatment (thyroidectomy), or medications.1
Tooth decay is the most common oral disease that affects people of all ages.2, 7-9 Tooth decay is an infectious disease caused by caries-causing bacteria. These bacteria, or the fermentation of carbohydrates, destroy the mineral tissue of the tooth and cause decay.2, 7, 9, 10 The spread of caries can be stopped by a process called remineralization. The presence of calcium and phosphate ions and high pH is essential for the remineralization of demineralized dentin.7, 11 Mineral metabolism is altered in thyroid dysfunction.12 Thyroid hormones appear to be effective in the metabolism of calcium, magnesium, and zinc.6 Yoshihara et al. showed that dental plaque in children without caries contained more calcium and phosphate than dental plaque in children with caries.8 Free ionized calcium plays an important role in the body, including blood coagulation, normal heart irritability, and muscle and nerve irritation.6 Combined saliva contains 99% water, electrolytes, antibacterial compounds, and various enzymes. Dental remineralization depends on the high saturation and ionic strength of saliva or dentin.7, 13 There is a positive association between high salivary calcium levels and high periodontal disease, as well as fewer carious teeth.14, 15 Due to the fact that studies on the evaluation of salivary calcium levels in patients with hypothyroidism are very few and according to studies the rate of dental caries and periodontal disease in these patients is high, this study aimed to evaluate the salivary level of calcium in patients with hypothyroidism.1
2 MATERIALS AND METHODS
this study was a large single center study. In this study, 85 patients with clinical hypothyroidism with blood concentrations of TSH > 10 mlu/L and T4 < 4 mlu/L and clinical signs of auxiliary thyroid diseases such as fatigue, dry skin, cold sensation, and hair loss or had low subclinical hypothyroidism with blood concentrations of 4 mlu/L < TSH < 10 mlu/L and T4 in normal doses and without clinical signs of hypothyroidism or very mild symptoms or patients with controlled or uncontrolled hypothyroidism treated with levothyroxine16, 17 who referred to Shahid Beheshti hospital in Hamadan, as study group and 85 people without a history of autoimmune disease and without a history of supplementation who did not have hypothyroidism and hyperthyroidism as control group. They were tested for TSH and matched with the study group in the terms of age and sex. This study started among the patients of Shahid Beheshti Hospital in Hamedan for 9 months from 2020. This research was approved by the ethics committee of Hamadan University of Medical Sciences (IR.UMSHA.1399.380). The selection of subjects in both groups was based on the following inclusion and exclusion criteria conditions (Table 1).
| Inclusion criteria | Exclusion criteria |
|---|---|
| Confirmation of diagnosis of hypothyroidism in the study group | Existence of symptoms of hypothyroidism in the control group |
| No hypothyroidism or hyperthyroidism | Consumption of calcium-containing drugs |
| No hyperthyroidism in the study group | Smoking |
| History of other thyroid diseases and thyroid cancers | |
| Taking medications containing iodine, antidepressants, heart disease and hypertension, corticosteroids | |
| In the control group, a history of type 1 and 2 diabetes, vitiligo, rheumatoid arthritis | |
| evidence of hypothyroidism or hyperthyroidism |
- 1.
In study group: Confirmation of diagnosis of hypothyroidism in the study group (with clinical hypothyroidism with blood concentrations of TSH > 10 mlU/L and T4 < 4 mlU/L and clinical signs of hypothyroidism such as fatigue, dry skin, cold, and hair loss or with subclinical hypothyroidism with blood concentrations of 4 mlU/L < TSH < 10 mlU/L and T4 in normal amounts and without clinical signs of adjuvant thyroid disease or very mild symptoms or a patient with controlled or uncontrolled hypothyroidism who are treated with levothyroxine).
- 2.
In control group: No hypothyroidism or hyperthyroidism (blood TSH level <0.4 mlU/L and does not have symptoms such as hyperactivity, heat intolerance, sweating, and palpitations).16, 17
- 3.
No hyperthyroidism in the study group.
- 1.
Existence of symptoms of hypothyroidism in the control group.
- 2.
Consumption of calcium-containing drugs (in both cases).
- 3.
Smoking (in both cases).
- 4.
History of other thyroid diseases and thyroid cancers (in both cases).
- 5.
Taking drugs containing iodine, antidepressants, heart disease and hypertension, corticosteroids (in both cases).
- 6.
In control group, history of type 1 and 2 diabetes, vitiligo, rheumatoid arthritis.
- 7.
There was evidence of hypothyroidism or hyperthyroidism (in control group).
2.1 Sample collection and analysis
Participant volunteers were asked to refrain from eating, drinking, or brushing their teeth for about 90 min before sample collection. After obtaining consent and completing the consent form, saliva samples were prepared using the Navazesh method.18 The Un-stimulating saliva sampling method was that the subjects poured 2−5 mL of saliva into the sample container for 5 min while sitting and with the head slightly bent forward. Saliva samples were then quickly stored on the ice box at 4°C and sent to the laboratory within 20 min, where they were stored at −30°C.18 After collecting saliva samples, to analysis the calcium concentration in samples, the samples were centrifuged for 20 min at speed of 4000 rpm. Two hundred microliters of the supernatant was placed in two separate containers and kept at −30°C until the analysis. Before injecting the samples into the device, 0.05 mL of nitric acid (70%) was added to 1 mL of each sample. Inductively coupled plasma-optical emission spectrometry (ICP-OES) (710-ES Varian) was used to analysis of calcium level in salivary samples.19, 20
2.2 Statistical analysis
Descriptive statistics (central indices [average] and dispersion [standard deviation]) at 95% confidence level were used to determine the average salivary calcium level. Also, to compare the average salivary calcium level in the studied groups, an independent t-test was used. A significance level of 0.05 was used for the two-sided test to test the research hypothesis.
In this study, we used Pearson's correlation coefficient test with a significance level of 0.05 to investigate the correlation between quantitative variables (calcium and thyroid hormone). All analyses were conducted using Stata 14 software.
2.3 Sample size calculation
The sample size calculation was made based on the mean difference test at the 95% confidence level as 85.21
3 RESULTS
In the present study, saliva samples were prepared from 85 patients as the case group and 85 healthy subjects as the control group, and calcium ions concentration in these samples were determined. Both groups were matched in terms of age and sex. As shown in Figure 1, there was a significant difference between the average of salivary calcium in healthy subjects and those with hypothyroidism. Also, salivary calcium levels in healthy subjects were significantly higher than salivary calcium levels in hypothyroidism patients (p < 0.001). Also, in comparison between salivary calcium concentration and blood levels of thyroid hormones, there is no significant relationship between salivary calcium concentration and TSH and T4 hormones in patients with hypothyroidism (Table 2).
| Ca | ||
|---|---|---|
| TSH | The correlation coefficient | −0.02 |
| p Value | 0.819 | |
| T4 | The correlation coefficient | −0.06 |
| p Value | 0.534 |
4 DISCUSSION
At this time, limited studies have been performed to assess the salivary calcium levels in patients with hypothyroidism. Most studies have been assessed other elements such as selenium, zinc, copper, magnesium, and manganese, and blood samples. In this study, the salivary calcium levels in patients with hypothyroidism and healthy subjects were compared. Our results are in agreement with the results of Anuradha et al. which the salivary calcium levels in patients with hypothyroidism were significantly lower than the control group.22
Hakim et al. showed that the serum calcium level of patients with hypothyroidism is significantly lower than healthy people.23 In the study of Simak et al., magnesium, calcium, and zinc were evaluated in the serum of mice with hypothyroidism. They showed that magnesium and zinc levels in patients were significantly different in comparison with healthy subjects, while no significant difference was observed in serum calcium levels.6 The reason for the difference between the results of Simak et al. and the present study can be related to the difference in the study population that in the above study the rat was used and our study was related to humans, as well as the type of sample as serum in that study and saliva in our study. Abdullah et al. showed that there is no significant difference between blood calcium concentration and blood thyroid hormone concentration which is in agreement with our results.24 In the Cornejo study, caries in the molar teeth increased as salivary levels of calcium and phosphorus decreased.25 Sewón et al. showed that people with more salivary calcium had more caries-free teeth and less DMFT.26, 27 According to the present study, salivary calcium levels were lower in patients with hypothyroidism compared to the control group. Also, a decrease in salivary calcium levels showed in our study may be associated with an increase in caries. Therefore, in our opinion, one of the reasons for the increase in tooth decay in patients with hypothyroidism may be the decrease in calcium in saliva, which reduces tooth remineralization.1, 7
5 CONCLUSION
In conclusion, the results of this study show that salivary calcium levels in patients with hypothyroidism is lower than the control group. There is an association between salivary calcium levels in patients with hypothyroidism. It seems that a decrease in salivary calcium levels may be associated with increased caries in these people. It is also possible to help patients with hypothyroidism by consuming calcium-rich foods or calcium supplements to prevent the effects of calcium deficiency as well as dental caries.
AUTHOR CONTRIBUTIONS
Shiva Borzuei: Investigation; methodology; validation. Samaneh Vaziri Amjad: Funding acquisition; methodology; project administration; supervision; validation, writing—review and editing. Mohammadreza Badiei: Data curation; methodology; writing—original draft. Abbas Farmany: Methodology; writing—original draft; writing—review and editing. Zahra Cheraghi: Formal analysis; software; validation.
ACKNOWLEDGMENTS
This research was funded by Hamadan University of Medical Sciences.
CONFLICT OF INTEREST STATEMENT
The authors declare conflict of interest.
ETHICS STATEMENT
Ethical approval for this study was obtained from ethics committee of Hamadan University of Medical Sciences (HUMS), (Approval ID: IR.UMSHA.1399.380).
TRANSPARENCY STATEMENT
The lead author Samaneh Vaziri Amjad, Abbas Farmany affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
DATA AVAILABILITY STATEMENT
Data supporting this study are included within the article.




