Anemia prevalence and its predictors among children under-five years in Ghana. A multilevel analysis of the cross-sectional 2019 Ghana Malaria Indicator Survey
Abstract
Background and Aims
Despite the implementation of anemia control interventions in Ghana, anemia prevalence is still high in children under-fives. Reducing the prevalence of anemia requires identifying and targeting associated critical risk factors. This study seeks to identify predictors of anemia among children under-fives in Ghana.
Methods
Nationally representative data from the 2019 Ghana Malaria Indicator Survey was used in this study. Both fixed and random effects (multilevel) logistic regression models were applied to 2434 children to identify critical factors associated with anemia.
Results
In this study, 54% (95% confidence interval [CI] 52.0–57.0) of children under-5 years were anemic. Infants were more likely to be anemic (66.7%) compared with other children below 5 years. In the multivariable multilevel model, the risk of anemia was found to be higher in younger children especially 6–11 months old (adjusted odds ratio [aOR] = 3.59, CI: 2.54–5.08) and 12–23 months old (aOR = 2.97, CI: 2.08–4.23), children who had malaria (aOR = 1.53, CI: 1.13–2.06), children whose mothers were not registered but not covered with health insurance (aOR = 1.45, CI: 1.21–1.74) or were not even registered for insurance (aOR = 1.49, CI: 1.15–1.93), children born to adolescent mothers (aOR = 2.21, CI: 1.36–3.57), children born to non-Christian mothers (Islam [aOR = 1.53, CI: 1.17–2.00]), children born to families of poorer households (poorest [aOR = 3.01, CI: 1.64–5.51]; poorer [aOR = 2.56, CI: 1.65–3.98]); middle (aOR = 2.03, CI: 1.32–3.11) and richer (aOR = 1.78, CI: 1.19–2.64), and children who lived in either Upper East (aOR = 2.03, CI: 1.26–3.26) or Central (aOR = 2.52, CI: 1.42–4.47) regions. Significant unobserved community-level differences in anemia prevalence were observed.
Conclusion
The probability of anemia in children under-fives differs substantially from one community to another, and the prevalence remains high. The identified critical risk factors should be addressed. Multifaceted and targeted approaches are needed to help reduce the anemia prevalence in this setting to achieve the multiple United Nation's Sustainable Development Goals, which are related to risk and prevalence of anemia by 2030.
1 BACKGROUND
Anemia in children under-5 years although preventable, is a severe public health problem which is closely related to achieving multiple United Nation's Sustainable Development Goals (SDGs).1-3 Despite the numerous interventions and control plans such as intermittent iron supplication and food fortification that has been implemented, anemia prevalence (42.6%) and deaths of (45% of children deaths) children under-5 years globally remains high.4-10 However, in the WHO African region, the prevalence of anemia is estimated to be 68% among children under-5 years.11, 12 In sub-regions where malaria is endemic, the prevalence of anemia is higher (49%–76%) compared to nonendemic malaria regions.13-15
Reducing the incidence of anemia is essential for improving the health and well-being of populations around the world, especially in Asia and Africa, where it is most prevalent.3, 16, 17 Anemia may be caused by vitamin deficiency, iron deficiency, sickle cell anemia, hemolytic anemia, aplastic anemia, or anemia of chronic disease.18, 19 Anemia during pregnancy has both maternal and fetal consequences of which a newly born may suffer from reduced iron store problem from birth up to infancy and the demand for iron during the period of rapid growth.2, 9, 20, 21 Also, during pregnancy and lactation there is an increasing need for iron, vitamins, and minerals by these groups of women, the lack of it makes them and children under-5 years the most vulnerable to anemia.21-23
Although most mothers have been sensitized on the consequences of iron deficiency during antenatal and postnatal clinics, poverty, poor socioeconomic challenges, household food insecurity, and monotonous diet hinder them from eating healthy meals resulting to anemia.7 Also, mothers who do not visit antenatal/postnatal clinic, mothers' level of education, diarrhea, malaria, fever, parasitic infestations, poor sanitation, and maternal anemia are other circumstances that leads to anemia.1, 24-26
Studies have proven that the factors associated with anemia are multifactorial and context-dependent.21 The contribution of these determinants to childhood anemia are complex and vary from country, dietary practice, and environmental factors.27, 28 For international bodies, governments, and other stakeholders to be guided and know the appropriate interventions to implement in Ghana, country specific predictors of anemia in children under-fives must be ascertained.29 However, to the best of our knowledge, we are yet to come across any study in Ghana using a multilevel model to assess country specific potential predictors of anemia, and to quantify possible unobserved community level differences in anemia prevalence. Also, anemia is a continuous phenomenon and requires continuous assessments of its predictors to inform timely and targeted interventions. Therefore, the focus of this study is to quantify unobserved community-level differences in anemia and to simultaneously determine critical predictors of anemia prevalence in children under-fives utilizing multilevel modeling framework to inform timely and targeted intervention strategies as part of a broad efforts to achieving the SDGs related to health by 2030.
2 METHODS
2.1 Study design and participants
Secondary data from the 2019 Ghana Indicator Malaria Survey (GMIS) which was collected as part of the most recent phase of Ghana Demographic and Health Survey (GDHS) was used for this study.30 Demographic and Health Survey (DHS) which is nationally representative uses a two-stage stratified sampling design method by using enumeration areas from the most current Ghana census data. A total of 200 clusters (103: rural and 97 urban) were used.31 The survey provided information on all 10 regions in Ghana at the time, although the regions have now been sub-divided to be 16. Because the administrative boundaries of the additional 6 newly created regions were not available at the time of conducting 2019 GMIS, the 10 regions were used.30
2.2 Study area
The study used data from 2019 Ghana Malaria Indicator Survey. The children recode data file which was part of the 2019 GMIS was used for the analysis of this study.
2.3 Sample size
Total observations (3004) realized for the 2019 GMIS children recode data file was used. However, since the study focused on assessing predictors of anemia in children under-fives, only data on these children with available anemia status were included in the study resulting in a final sample of 2434, representing 81.0% of the original sample.30
2.4 Study variables
2.4.1 Outcome variable
Anemia among children under-five defined as children with hemoglobin below 11.0 g/dL was the study outcome. Hemoglobin level was dichotomized to 1 if child had hemoglobin level below 11.0 g/dL otherwise, 0.
2.4.2 Independent variables
The independent variables can be put into three main groups namely, child characteristics, mother or caregiver characteristics and the household characteristics. The child characteristics included sex of child (male or female), age in years (0–4), type of birth (single or multiple) birth order (1st, 2nd, or 3rd+ child), preceding birth interval in months (<18months, 18+ months, or 1st born), experience of fever in the past 2 weeks (no fever, fever with negative malaria test and fever with positive malaria test, fever with unknown malaria test). Mother or caregiver characteristics included age group in years (15–19, 20–29, 30–39, and 40–49 years), parity (1 child, 2–3 children, 4–5 children, and 6+ children), highest education (no education, primary, secondary, and higher), literacy level of mother (cannot read at all, able to read only parts of sentence, or able to read whole sentence), religion (catholic/Christians, Islam, or Others [traditional, none, etc.]), ethnicity (Akan, Ewe, Mole-Dagbani, and Others ethnicity), number of births for last 5 years (1, 2, or 3+ births), and access to health insurance (no access, registered but not covered, or registered and covered). Household characteristics included region of residence, place of residence (rural or urban), age group of household head in years ( < 30, 30–39, 40–49, 50–59, or 60+), sex of household head (male or female), type of cooking fuel (nonsolid fuel or solid fuel), floor material (improved or unimproved material), wall material (improved or unimproved material), roof material (improved or unimproved material), source of drinking water (improved or unimproved source), toilet facility (improved or unimproved facility), and household wealth quintile (poorest, poor, middle, rich, or richest). These variables have been shown to be significant factors associated with anemia in literature.7, 12, 27, 32 Re-categorization of some selected variables from the original survey variables are presented in Table 1.
| Variable name & category | Original categories |
|---|---|
| Religion | |
| Catholic/Christians | Catholic, Anglican, Methodist, Presbyterian, Pentecostal/Charismatic, Other Christians. |
| Islam | Islam |
| Others (Trad./None etc) | Traditional/Spiritualist, No Religion, Other |
| Ethnicity | |
| Akan | Akan |
| Ewe | Ewe |
| Mole-Dagbani | Mole-Dagbani |
| Others | Ga/Dangme, Guan, Grusi, Gurma, Mande, Other |
| Cooking fuel | |
| Nonsolid | Electricity, LPG, natural gas, biogas |
| Solid | Charcoal, wood, straw/shrubs/grass, agricultural crop |
| Household floor material | |
| Unimproved material | Earth/sand, dung, wood planks |
| Improved material | Parquet or polished wood, vinyl or asphalt strips, ceramic/marble/porcelain tiles/terrazzo, cement, woolen carpet/synthetic carpet, linoleum/rubber carpet |
| Household wall material | |
| Unimproved material | No walls, cane/palm/trunks, mud/landcrete, bamboo with mud, stone with mud, plywood, cardboard, reused wood |
| Improved material | Cement, stone with lime/cement, bricks, cement blocks, wood planks/shingle |
| Household roof material | |
| Unimproved material | No roof, thatch/palm leaf, sod, rustic mat, palm/bamboo, wood planks |
| Improved material | Zinc/aluminum, ceramic/brick tiles, cement, roofing shingles, asbestos/slate roofing sheets |
| Source of drinking water | |
| Unimproved source | Unprotected well, unprotected spring, river/dam/lake/ponds/stream/canal/irrigation channel, rainwater, tanker truck, cart with small tank |
| Improved source | Piped into dwelling, piped to yard/plot, piped to neighbor, public tap/standpipe, tube well or borehole, protected well, protected spring, bottled water, sachet water |
| Type of toilet facility | |
| Unimproved facility | Flush to somewhere else, flush, don't know where, pit latrine with slab, pit latrine without slab/open pit, no facility/bush/field, hanging toilet/latrine, other |
| Improved facility | Flush to piped sewer system, flush to septic tank, flush to pit latrine, flush, bio-digester (biofil), ventilated improved pit latrine (VIP), composting toilet |
2.5 Statistical analysis
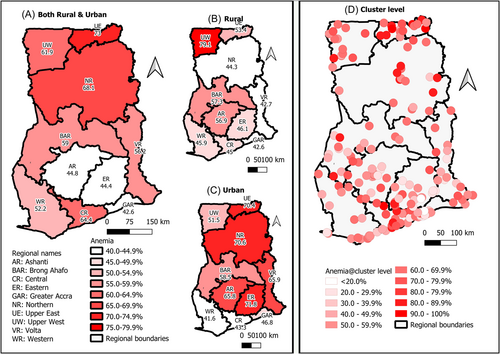
Stata SE version 17 (Stata Corp) was used to perform the statistical analysis. Descriptive analysis was performed using the frequency and both unweighted and weighted percentages for categorical variables. All analysis thereafter were weighted and accounted for clustering, stratification and design effect using the survey mode in Stata (“svy”) due to the complex survey design of the MIS data. The prevalence of anemia was estimated with the corresponding 95% confidence interval (CI) estimates across the categories of all the independent variables considered in the study. The simple Poisson regression model was used to assess the difference in prevalence ratios of anemia across the categories of the exposure variables. Estimates of anemia prevalence across regions and by rural and urban residence as well as study clusters was presented in the form of choropleth maps generated using the Quantum Geographic Information System (QGIS) version 3.28.2.
The binary logistic regression model was used to assess the factors associated with anemia prevalence among the children under-5 years. First the crude odds ratio (OR) was estimated with the corresponding 95% CI and p-values from the simple logistic regression model. Next the single level fixed effect multivariable logistic regression model was fitted for variables considered in the simple logistic regression analysis. Finally, we extend the single level multivariable logistic regression model to random intercept and random slope multilevel logistic regression model and estimated the ORs and their corresponding 95% CI and p-values. The individual child served as Level 1 and community as Level 2. We hypothesized that the effect of the rural–urban variable will vary from one community to another, hence the random slope model. Multicollinearity was assessed for all variables considered in the study using variance inflation factor (VIF) and VIF < 10 was considered acceptable. The Hosmer–Lemeshow goodness of fit test was applied to examine how well the model fits the data. The area under the operating characteristics curve (AUROCC) was determined and plotted for both the single level multivariable logistic regression and the multilevel logistic regression models. All statistical analysis were considered significant at p-value < 0.05 for a two-sided test.
2.6 Ethical approval
This study was based on publicly available data set from the MEASURE DHS program. No ethical approval was needed since it did not directly involve contacts between the authors and the individuals interviewed. However, the protocol for the 2019 Ghana Malaria Indicator Survey was approved by the Ghana Health Service Ethical Review Committee and ICF's Institutional Review Board. The risk and benefits of participation in the survey were explained to respondents, including informed consent for the interview or blood collection, and informed consent was sought from all respondents. Also, the data used for this study has no contact details of the interviewed participants and households, and permission was sought from and given by the MEASURE DHS program for this study via the online portal http://www.dhsprogram.com.
3 RESULTS
3.1 Characteristics of study population
From the data set using the weighed percentages, children under-5 years whose anemia status was available were 2434 with 1236 (50.9%) being males. Multiple birth was 76 (2.6%) and two-third (67.8%) were the first child. Majority of the children (88.8%) had no fever in the 2-weeks before survey interview, while 218 (7.5%) had a fever with malaria positive test. Young mothers (20–29) were more (44.6%) than mothers in other age groups with about 27.5% of the women having between four and five children. However only 108 (5.2%) of the mothers had attained higher educational status and 1428 (54.2%) cannot read at all. Children aged 2 years were more than children of other ages, they represented 23.8% of the study population. However, most (58.9%) of them lived in rural areas. Although majority of study participants (23.4%) lived in poorest household with household heads mostly being males (70.2%), about 87.8% had improved water source and 1563 (57.7%) had unimproved toilet facilities in their homes/community (Table 2).
| Unweighted | Weighted | Prevalence of anemia | ||
|---|---|---|---|---|
| Characteristics | n (%) | % | % [95% CI] | p-Value |
| Overall | 2434 (100.0) | 100 | 54.5 [52.0–57.0] | |
| Child characteristics | ||||
| Sex of child | 0.194 | |||
| Male | 1236 (50.8) | 50.9 | 56.4 [52.9–59.8] | |
| Female | 1198 (49.2) | 49.1 | 52.6 [48.6–56.6] | |
| Age group of children | <0.001 | |||
| 6–11 months | 305 (12.5) | 11.9 | 66.7 [59.9–72.9] | |
| 12–23 months | 565 (23.2) | 23.5 | 62.9 [57.8–67.8] | |
| 24–35 months | 554 (22.8) | 23.8 | 59.2 [54.2–64.0] | |
| 36–47 months | 521 (21.4) | 21.2 | 50.1 [45.2–55.0] | |
| 48–59 months | 489 (20.1) | 19.7 | 36.3 [31.6–41.3] | |
| Type of birth | 0.584 | |||
| Single birth | 2358 (96.9) | 97.4 | 54.4 [51.9–56.9] | |
| Multiple birth | 76 (3.1) | 2.6 | 58.3 [43.8–71.4] | |
| Birth order | <0.001 | |||
| 1st child | 1675 (68.8) | 67.8 | 49.5 [46.6–52.4] | |
| 2nd child | 690 (28.3) | 29.2 | 65.2 [61.1–69.1] | |
| 3rd+ child | 69 (2.8) | 3.0 | 65.9 [52.3–77.2] | |
| Preceding birth interval (months) | <0.001 | |||
| <18 months | 52 (2.1) | 2.3 | 57.0 [40.8–71.7] | |
| 18+ months | 707 (29.0) | 29.9 | 65.9 [61.5–70.0] | |
| 1st born | 1675 (68.8) | 67.8 | 49.5 [46.6–52.4] | |
| Fever with malaria in the past 2 weeks | <0.001 | |||
| No fever | 2105 (86.5) | 88.8 | 53.2 [50.4–55.9] | |
| Yes, negative malaria | 69 (2.8) | 2.4 | 56.7 [42.5–69.9] | |
| Yes, positive malaria | 218 (9.0) | 7.5 | 67.4 [58.8–75.0] | |
| Yes, unknown results | 42 (1.7) | 1.3 | 70.9 [53.8–83.6] | |
| Mother/caregiver characteristics | ||||
| Age group of mothers | 0.001 | |||
| 15–19 | 90 (3.7) | 3.3 | 71.1 [60.3–79.9] | |
| 20–29 | 1092 (44.9) | 44.6 | 55.2 [51.8–58.5] | |
| 30–39 | 976 (40.1) | 41.4 | 53.8 [50.1–57.6] | |
| 40–49 | 276 (11.3) | 10.7 | 49.4 [42.0–56.8] | |
| Parity of mother | 0.001 | |||
| One child | 391 (16.1) | 16.2 | 53.1 [47.5–58.6] | |
| 2–3 children | 987 (40.6) | 42.0 | 50.8 [47.0–54.7] | |
| 4–5 children | 674 (27.7) | 27.5 | 56.5 [51.6–61.3] | |
| 6+ children | 382 (15.7) | 14.3 | 63.3 [57.7–68.5] | |
| Highest education | <0.001 | |||
| No education | 698 (28.7) | 22.9 | 63.4 [58.7–67.9] | |
| Primary | 531 (21.8) | 21.9 | 61.5 [55.2–67.5] | |
| Secondary | 1097 (45.1) | 50.0 | 48.9 [45.4–52.4] | |
| Higher | 108 (4.4) | 5.2 | 40.3 [31.5–49.7] | |
| Literacy level of mother | <0.001 | |||
| Cannot read at all | 1428 (58.7) | 54.2 | 60.0 [56.5–63.4] | |
| Able to read only parts of sentence | 179 (7.4) | 7.7 | 53.7 [45.4–61.9] | |
| Able to read whole sentence | 827 (34.0) | 38.2 | 47.0 [43.1–50.9] | |
| Religion of mother | <0.001 | |||
| Catholic/Christians | 1724 (70.8) | 74.3 | 50.4 [47.6–53.2] | |
| Islam | 591 (24.3) | 21.8 | 66.0 [60.7–70.9] | |
| Others (Trad./None etc) | 119 (4.9) | 3.9 | 69.4 [59.9–77.6] | |
| Ethnicity of mother | <0.001 | |||
| Akan | 822 (33.8) | 40.4 | 47.9 [43.8–52.1] | |
| Ewe | 307 (12.6) | 15.1 | 53.7 [46.8–60.6] | |
| Mole-Dagbani | 807 (33.2) | 22.4 | 67.2 [62.1–72.0] | |
| Others | 498 (20.5) | 22.1 | 54.3 [49.7–58.8] | |
| Births in the last 5 years | 0.132 | |||
| 1 | 1373 (56.4) | 56.2 | 53.1 [50.0–56.2] | |
| 2 | 948 (38.9) | 38.2 | 57.4 [53.4–61.2] | |
| 3+ | 113 (4.6) | 5.6 | 49.6 [39.6–59.6] | |
| Access to health insurance | 0.002 | |||
| Not registered | 255 (10.5) | 10.8 | 60.0 [53.1–66.4] | |
| Registered, not covered | 922 (37.9) | 37.9 | 58.6 [54.9–62.1] | |
| Registered, covered | 1257 (51.6) | 51.3 | 50.4 [46.8–54.1] | |
| Household characteristics | ||||
| Household size | <0.001 | |||
| 2–3 members | 314 (12.9) | 14.5 | 46.3 [40.8–51.9] | |
| 4–6 members | 1183 (48.6) | 50.4 | 51.9 [48.8–55.1] | |
| 7–9 members | 618 (25.4) | 23.4 | 60.0 [55.4–64.6] | |
| 10+ members | 319 (13.1) | 11.6 | 65.1 [57.5–72.0] | |
| Number children under-five in household | 0.005 | |||
| 1 child | 986 (40.5) | 41.4 | 50.9 [47.6–54.2] | |
| 2 children | 955 (39.2) | 38.4 | 55.3 [50.8–59.7] | |
| 3 children | 319 (13.1) | 13.4 | 58.2 [49.7–66.3] | |
| 4 children | 174 (7.1) | 6.8 | 65.0 [56.4–72.8] | |
| Age of household head | 0.623 | |||
| <30 | 378 (15.5) | 16.2 | 54.3 [49.2–59.2] | |
| 30–39 | 806 (33.1) | 35.8 | 52.4 [48.4–56.4] | |
| 40–49 | 599 (24.6) | 23.6 | 55.3 [49.4–61.1] | |
| 50–59 | 295 (12.1) | 11.3 | 57.2 [50.7–63.4] | |
| 60+ years | 356 (14.6) | 13.0 | 57.1 [50.5–63.5] | |
| Sex of household head | 0.558 | |||
| Male | 1779 (73.1) | 70.2 | 55.0 [52.0–58.0] | |
| Female | 655 (26.9) | 29.8 | 53.4 [49.0–57.8] | |
| Type of cooking fuel | <0.001 | |||
| Non-solid fuel | 316 (13.0) | 17.4 | 39.8 [34.0–45.8] | |
| Solid fuel | 2118 (87.0) | 82.6 | 57.7 [54.7–60.6] | |
| Household floor material | 0.037 | |||
| Unimproved material | 256 (10.5) | 8.8 | 61.9 [54.1–69.1] | |
| Improved material | 2178 (89.5) | 91.2 | 53.8 [51.2–56.4] | |
| Household wall material | <0.001 | |||
| Unimproved material | 662 (27.2) | 21.1 | 64.5 [59.8–68.9] | |
| Improved material | 1772 (72.8) | 78.9 | 51.9 [49.2–54.6] | |
| Household roof material | <0.001 | |||
| Unimproved material | 136 (5.6) | 4.3 | 66.7 [59.8–72.8] | |
| Improved material | 2298 (94.4) | 95.7 | 54.0 [51.4–56.5] | |
| Source of drinking water | 0.002 | |||
| Unimproved source | 357 (14.7) | 12.2 | 65.3 [57.6–72.2] | |
| Improved source | 2077 (85.3) | 87.8 | 53.1 [50.3–55.8] | |
| Type of toilet facility | <0.001 | |||
| Unimproved facility | 1563 (64.2) | 57.7 | 60.1 [56.8–63.4] | |
| Improved facility | 871 (35.8) | 42.3 | 46.9 [43.4–50.4] | |
| Household wealth quintile | <0.001 | |||
| Poorest | 810 (33.3) | 23.4 | 68.5 [64.7–72.1] | |
| Poorer | 511 (21.0) | 21.6 | 59.2 [53.8–64.4] | |
| Middle | 479 (19.7) | 21.1 | 54.6 [48.4–60.7] | |
| Richer | 347 (14.3) | 18.0 | 48.2 [41.9–54.7] | |
| Richest | 287 (11.8) | 15.8 | 34.6 [28.9–40.9] | |
| Community level characteristics | ||||
| Region of residence | <0.001 | |||
| Western | 243 (10.0) | 10.7 | 52.2 [46.6–57.7] | |
| Central | 216 (8.9) | 7.2 | 64.4 [53.6–73.9] | |
| Greater Accra | 174 (7.1) | 12.6 | 42.6 [35.7–49.7] | |
| Volta | 212 (8.7) | 11.2 | 56.2 [51.1–61.2] | |
| Eastern | 189 (7.8) | 9.9 | 44.4 [35.4–53.8] | |
| Ashanti | 251 (10.3) | 16.6 | 44.8 [39.1–50.6] | |
| Brong Ahafo | 236 (9.7) | 9.1 | 59.0 [51.6–66.0] | |
| Northern | 407 (16.7) | 15.1 | 68.1 [62.3–73.3] | |
| Upper east | 236 (9.7) | 4.3 | 73.0 [65.0–79.7] | |
| Upper west | 270 (11.1) | 3.3 | 61.9 [56.0–67.4] | |
| Place of residence | <0.001 | |||
| Urban | 912 (37.5) | 41.1 | 48.0 [44.4–51.6] | |
| Rural | 1522 (62.5) | 58.9 | 59.1 [55.8–62.3] | |
3.2 Prevalence of anemia
The anemia prevalence of children under-5 years in Ghana was 54.5% (95% CI 52.0–57.0) with 59.1% in rural areas and 41.1% in Urban areas (Table 2). The Upper East region recorded the highest (73.0%), followed by Northern region (68.1%) prevalence of anemia in children under-5 years in Ghana whilst Greater Accra region recorded the least prevalence (42.6%) of anemia in the study population. In terms of the stratification to rural and urban areas within regions, the anemia was highest in the rural areas of the Upper West region (79.1%) followed by the Brong Ahafo (57.3%), the Ashanti (56.9%), and the Upper East (53.4%) regions whilst anemia highest the urban areas of the Eastern (71.8%), Upper East (70.4%) and the Northern (70.6%) regions. Figure 1D shows the spot map of the prevalence of anemia at the cluster level (Figure 1).
Infants were more likely to be anemic (66.7%) compared with other children below 5 years. Children who tested positive to malaria were more likely to be anemic compared with children who had no fever, or no malaria 2 weeks before the survey (67.4%; at 95% CI 58.8–75.0; p < 0.01). Teenage mothers (20–29 years) recorded a higher prevalence of anemia in their children compared with children of younger and older mothers (71.1%; at 95% CI 60.3–79.9; p < 0.01). Anemia was higher (63.3%) in children under-5 years of mothers who had more than six children. Mothers who had never been educated had a higher prevalence (63.4%) of their children having anemia than mothers who had attained higher education (40.3%). Children who were neither registered nor covered on any health insurance scheme attained a higher prevalence of anemia (60.0%) than children who were registered and covered (50.4%). Also, children for very poor households, unimproved toilet facilities and unimproved water facilities were more likely to be anemic, 68.5%, 60.1%, and 65.3%, respectively, than children from richer (34.6%), improved toilets (46.9%) and improved water facilities (53.1%) (Table 2).
3.3 Factors associated with anemia in children under-five from the multilevel model
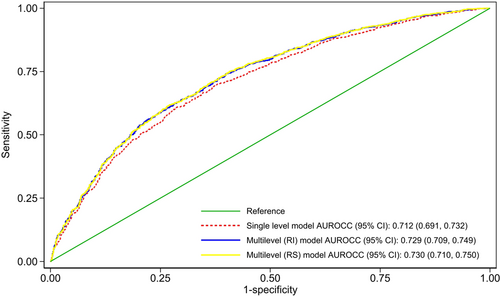
The results from the single multivariable logistic regression and the multilevel regression analyses were presented in Table 3. All the model comparison statistics, such as the Akaike information criteria (AIC), Bayesian information criteria (BIC), and AUROC values favored the multilevel logistic regression models over the single-level multivariable logistic regression model. Among the multilevel models, the random intercept model was preferred to the random slope model because it has the lowest AIC and BIC and negligible differences in the AUROC value under the principle of parsimony (Table 3 and Figure 2). Thus, the results showed that the random intercept multilevel logistic regression model was superior to the random slope multilevel multivariable logistic regression model. As a result, the interpretations and conclusions were based on the results from the random intercept multilevel logistic regression model.
| Adjusted models | ||||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted model | Fixed effect model | Random intercept multilevel model | Random slope multilevel model | |||||
| Characteristics | cOR [95% CI] | p-Value | aOR [95% CI] | p-Value | aOR [95% CI] | p-Value | aOR [95% CI] | p-Value |
| Sex of child | ||||||||
| Male | 1.16 [0.93–1.46] | 0.192 | 1.20 [1.07–1.35] | 0.002 | 1.20 [1.07–1.36] | 0.003 | 1.20 [1.07–1.36] | 0.002 |
| Female | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | ||||
| Age group of children | ||||||||
| 6–11 months | 3.51 [2.37–5.20] | <0.001 | 3.47 [2.47–4.86] | <0.001 | 3.59 [2.54–5.08] | <0.001 | 3.60 [2.54–5.09] | <0.001 |
| 12–23 months | 2.98 [2.24–3.96] | <0.001 | 2.86 [1.97–4.13] | <0.001 | 2.97 [2.08–4.23] | <0.001 | 2.97 [2.07–4.27] | <0.001 |
| 24–35 months | 2.55 [1.88–3.46] | <0.001 | 2.60 [1.85–3.66] | <0.001 | 2.61 [1.82–3.74] | <0.001 | 2.61 [1.83–3.74] | <0.001 |
| 36–47 months | 1.76 [1.32–2.35] | <0.001 | 1.77 [1.29–2.43] | <0.001 | 1.80 [1.32–2.46] | <0.001 | 1.79 [1.30–2.47] | <0.001 |
| 48–59 months | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | ||||
| Type of birth | ||||||||
| Single birth | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | ||||
| Multiple birth | 1.17 [0.65–2.10] | 0.600 | 1.14 [0.57–2.30] | 0.710 | 1.18 [0.59–2.36] | 0.647 | 1.18 [0.58–2.39] | 0.642 |
| Birth order | ||||||||
| 1st child | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | ||||
| 2nd child | 1.91 [1.58–2.32] | <0.001 | 1.41 [1.13–1.75] | 0.003 | 1.40 [1.12–1.75] | 0.003 | 1.40 [1.12–1.75] | 0.003 |
| 3rd+ child | 1.97 [1.09–3.55] | 0.024 | 1.36 [0.70–2.64] | 0.371 | 1.32 [0.65–2.71] | 0.441 | 1.33 [0.65–2.71] | 0.438 |
| Fever with malaria in the past 2 weeks | ||||||||
| No fever | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | ||||
| Yes, negative malaria | 1.15 [0.64–2.07] | 0.631 | 1.15 [0.56–2.38] | 0.700 | 1.16 [0.55–2.43] | 0.691 | 1.16 [0.55–2.44] | 0.701 |
| Yes, positive malaria | 1.82 [1.24–2.69] | 0.003 | 1.48 [1.12–1.96] | 0.006 | 1.53 [1.13–2.06] | 0.006 | 1.52 [1.13–2.05] | 0.006 |
| Yes, unknown results | 2.15 [1.03–4.49] | 0.042 | 1.73 [0.91–3.32] | 0.096 | 1.74 [0.91–3.34] | 0.096 | 1.75 [0.90–3.40] | 0.097 |
| Age group of mothers | ||||||||
| 15–19 | 2.52 [1.43–4.45] | 0.002 | 2.31 [1.42–3.75] | 0.001 | 2.21 [1.36–3.57] | 0.001 | 2.21 [1.36–3.58] | 0.001 |
| 20–29 | 1.26 [0.93–1.71] | 0.129 | 1.50 [0.99–2.26] | 0.053 | 1.47 [0.96–2.25] | 0.074 | 1.48 [0.97–2.26] | 0.067 |
| 30-39 | 1.20 [0.86–1.66] | 0.280 | 1.38 [0.96–1.99] | 0.082 | 1.37 [0.95–1.98] | 0.095 | 1.37 [0.96–1.97] | 0.083 |
| 40-49 | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | ||||
| Parity of mother | ||||||||
| One child | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | ||||
| 2–3 children | 0.91 [0.69–1.21] | 0.525 | 0.90 [0.63–1.29] | 0.576 | 0.90 [0.63–1.28] | 0.558 | 0.90 [0.63–1.28] | 0.556 |
| 4–5 children | 1.15 [0.86–1.54] | 0.353 | 1.07 [0.68–1.66] | 0.778 | 1.03 [0.66–1.62] | 0.889 | 1.03 [0.66–1.60] | 0.899 |
| 6+ children | 1.52 [1.09–2.13] | 0.014 | 1.33 [0.91–1.95] | 0.142 | 1.31 [0.90–1.91] | 0.162 | 1.30 [0.89–1.89] | 0.171 |
| Highest education | ||||||||
| No education | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | ||||
| Primary | 0.92 [0.65–1.32] | 0.652 | 1.27 [0.92–1.76] | 0.150 | 1.30 [0.92–1.82] | 0.131 | 1.29 [0.92–1.81] | 0.137 |
| Secondary | 0.55 [0.43–0.70] | <0.001 | 0.95 [0.63–1.44] | 0.803 | 0.97 [0.63–1.50] | 0.892 | 0.96 [0.62–1.48] | 0.859 |
| Higher | 0.39 [0.26–0.58] | <0.001 | 1.15 [0.63–2.10] | 0.651 | 1.20 [0.62–2.32] | 0.589 | 1.20 [0.61–2.35] | 0.596 |
| Literacy level of mother | ||||||||
| Cannot read at all | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | ||||
| Able to read only parts of sentence | 0.77 [0.55–1.09] | 0.137 | 1.06 [0.74–1.54] | 0.742 | 1.06 [0.72–1.56] | 0.756 | 1.07 [0.72–1.58] | 0.732 |
| Able to read whole sentence | 0.59 [0.47–0.74] | <0.001 | 1.04 [0.68–1.58] | 0.860 | 1.03 [0.67–1.59] | 0.896 | 1.03 [0.67–1.60] | 0.892 |
| Religion of mother | ||||||||
| Catholic/Christians | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | ||||
| Islam | 1.91 [1.47–2.48] | <0.001 | 1.53 [1.17–1.99] | 0.002 | 1.53 [1.17–2.00] | 0.002 | 1.53 [1.18–1.98] | 0.001 |
| Others (Trad./None etc) | 2.23 [1.44–3.47] | <0.001 | 1.64 [1.09–2.47] | 0.017 | 1.61 [1.06–2.45] | 0.027 | 1.61 [1.06–2.45] | 0.027 |
| Ethnicity of mother | ||||||||
| Akan | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | ||||
| Ewe | 1.26 [0.90–1.77] | 0.180 | 1.14 [0.86–1.51] | 0.377 | 1.20 [0.88–1.63] | 0.253 | 1.20 [0.87–1.65] | 0.260 |
| Mole-Dagbani | 2.23 [1.68–2.96] | <0.001 | 1.39 [0.89–2.17] | 0.149 | 1.45 [0.91–2.31] | 0.117 | 1.47 [0.89–2.43] | 0.129 |
| Others | 1.29 [1.01–1.65] | 0.041 | 0.88 [0.64–1.21] | 0.417 | 0.88 [0.63–1.22] | 0.445 | 0.88 [0.64–1.22] | 0.452 |
| Births in the last five years | ||||||||
| 1 | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | ||||
| 2 | 1.19 [0.98–1.43] | 0.071 | 1.15 [0.84–1.57] | 0.399 | 1.17 [0.85–1.62] | 0.341 | 1.17 [0.85–1.62] | 0.340 |
| 3+ | 0.87 [0.57–1.33] | 0.514 | 0.79 [0.43–1.44] | 0.439 | 0.79 [0.42–1.48] | 0.462 | 0.79 [0.42–1.49] | 0.469 |
| Access to health insurance | ||||||||
| Not registered | 1.47 [1.09–1.98] | 0.012 | 1.47 [1.14–1.88] | 0.002 | 1.49 [1.15–1.93] | 0.002 | 1.49 [1.15–1.93] | 0.002 |
| Registered, not covered | 1.39 [1.13–1.71] | 0.002 | 1.45 [1.21–1.74] | <0.001 | 1.45 [1.21–1.74] | <0.001 | 1.46 [1.23–1.74] | <0.001 |
| Registered, covered | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | ||||
| Region of residence | ||||||||
| Western | 0.67 [0.48–0.94] | 0.019 | 1.35 [0.88–2.08] | 0.172 | 1.41 [0.90–2.20] | 0.133 | 1.40 [0.90–2.19] | 0.136 |
| Central | 1.11 [0.67–1.86] | 0.675 | 2.37 [1.36–4.12] | 0.002 | 2.47 [1.42–4.29] | 0.001 | 2.52 [1.42–4.47] | 0.002 |
| Greater Accra | 0.46 [0.31–0.67] | <0.001 | 1.26 [0.75–2.12] | 0.379 | 1.32 [0.78–2.25] | 0.300 | 1.32 [0.78–2.25] | 0.304 |
| Volta | 0.79 [0.57–1.09] | 0.151 | 1.28 [0.87–1.87] | 0.210 | 1.23 [0.84–1.79] | 0.281 | 1.25 [0.84–1.85] | 0.278 |
| Eastern | 0.49 [0.31–0.77] | 0.002 | 1.10 [0.67–1.80] | 0.713 | 1.14 [0.70–1.86] | 0.594 | 1.13 [0.70–1.81] | 0.626 |
| Ashanti | 0.50 [0.36–0.70] | <0.001 | 1.01 [0.65–1.57] | 0.976 | 1.05 [0.66–1.67] | 0.853 | 1.04 [0.65–1.65] | 0.867 |
| Brong Ahafo | 0.89 [0.60–1.31] | 0.542 | 1.45 [0.87–2.43] | 0.155 | 1.48 [0.87–2.51] | 0.145 | 1.50 [0.87–2.59] | 0.140 |
| Northern | 1.31 [0.92–1.87] | 0.128 | 1.33 [0.87–2.03] | 0.190 | 1.34 [0.87–2.05] | 0.184 | 1.37 [0.87–2.14] | 0.170 |
| Upper East | 1.66 [1.06–2.60] | 0.026 | 2.06 [1.27–3.34] | 0.003 | 2.07 [1.29–3.32] | 0.003 | 2.03 [1.26–3.26] | 0.004 |
| Upper West | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | ||||
| Place of residence | ||||||||
| Urban | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | ||||
| Rural | 1.57 [1.29–1.91] | <0.001 | 1.02 [0.84–1.23] | 0.868 | 1.00 [0.83–1.19] | 0.964 | 0.99 [0.83–1.18] | 0.927 |
| Household size | ||||||||
| 2–3 members | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | ||||
| 4–6 members | 1.25 [0.97–1.63] | 0.086 | 1.40 [0.96–2.04] | 0.077 | 1.40 [0.96–2.06] | 0.083 | 1.41 [0.96–2.07] | 0.076 |
| 7–9 members | 1.74 [1.34–2.28] | <0.001 | 1.54 [1.05–2.26] | 0.027 | 1.59 [1.08–2.33] | 0.018 | 1.60 [1.09–2.35] | 0.017 |
| 10+ members | 2.17 [1.49–3.14] | <0.001 | 1.81 [1.18–2.78] | 0.007 | 1.92 [1.25–2.95] | 0.003 | 1.92 [1.25–2.95] | 0.003 |
| Number children under-five in household | ||||||||
| 1 child | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | ||||
| 2 children | 1.19 [0.96–1.48] | 0.111 | 0.79 [0.60–1.03] | 0.076 | 0.78 [0.60–1.02] | 0.066 | 0.78 [0.60–1.03] | 0.076 |
| 3 children | 1.34 [0.92–1.96] | 0.122 | 0.87 [0.55–1.35] | 0.526 | 0.85 [0.54–1.35] | 0.490 | 0.85 [0.53–1.35] | 0.485 |
| 4 children | 1.79 [1.23–2.60] | 0.002 | 0.76 [0.43–1.35] | 0.352 | 0.74 [0.41–1.33] | 0.310 | 0.74 [0.41–1.35] | 0.323 |
| Age of household head | ||||||||
| <30 | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | ||||
| 30–39 | 0.93 [0.72–1.20] | 0.568 | 1.03 [0.78–1.35] | 0.838 | 1.05 [0.80–1.38] | 0.741 | 1.04 [0.79–1.37] | 0.771 |
| 40–49 | 1.04 [0.76–1.43] | 0.794 | 1.01 [0.74–1.37] | 0.947 | 1.03 [0.76–1.39] | 0.853 | 1.02 [0.76–1.38] | 0.879 |
| 50–59 | 1.13 [0.82–1.55] | 0.466 | 0.92 [0.77–1.11] | 0.403 | 0.92 [0.77–1.10] | 0.359 | 0.92 [0.77–1.10] | 0.349 |
| 60+ years | 1.12 [0.82–1.54] | 0.471 | 0.82 [0.64–1.05] | 0.117 | 0.83 [0.65–1.05] | 0.112 | 0.82 [0.65–1.05] | 0.113 |
| Sex of household head | ||||||||
| Male | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | ||||
| Female | 0.94 [0.76–1.16] | 0.555 | 1.16 [0.85–1.58] | 0.362 | 1.16 [0.84–1.59] | 0.370 | 1.15 [0.84–1.58] | 0.378 |
| Household wall material | ||||||||
| Unimproved material | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | ||||
| Improved material | 0.59 [0.48–0.74] | <0.001 | 1.07 [0.74–1.54] | 0.724 | 1.05 [0.73–1.52] | 0.787 | 1.05 [0.72–1.53] | 0.815 |
| Source of drinking water | ||||||||
| Unimproved source | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | ||||
| Improved source | 0.60 [0.42–0.86] | 0.005 | 0.95 [0.73–1.25] | 0.741 | 0.93 [0.71–1.20] | 0.559 | 0.94 [0.72–1.22] | 0.627 |
| Type of toilet facility | ||||||||
| Unimproved facility | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | ||||
| Improved facility | 0.59 [0.48–0.72] | <0.001 | 1.04 [0.76–1.42] | 0.830 | 1.03 [0.75–1.43] | 0.836 | 1.05 [0.76–1.46] | 0.776 |
| Household wealth quintile | ||||||||
| Poorest | 4.11 [2.98–5.67] | <0.001 | 2.80 [1.56–5.05] | 0.001 | 2.97 [1.63–5.42] | <0.001 | 3.01 [1.64–5.51] | <0.001 |
| Poorer | 2.74 [2.00–3.74] | <0.001 | 2.36 [1.58–3.51] | <0.001 | 2.52 [1.64–3.87] | <0.001 | 2.56 [1.65–3.98] | <0.001 |
| Middle | 2.27 [1.54–3.34] | <0.001 | 1.87 [1.31–2.68] | 0.001 | 1.98 [1.34–2.93] | 0.001 | 2.03 [1.32–3.11] | 0.001 |
| Richer | 1.76 [1.14–2.72] | 0.011 | 1.68 [1.17–2.41] | 0.005 | 1.74 [1.19–2.54] | 0.004 | 1.78 [1.19–2.64] | 0.005 |
| Richest | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | ||||
| Model summary | ||||||||
| AIC | 2871.988 | 2867.826 | 2869.425 | |||||
| BIC | 2982.136 | 2977.974 | 2985.37 | |||||
| AUROC (95% CI) | 0.712 [0.691–0.732] | 0.729 [0.709–0.749] | 0.730 [0.710–0.750] | |||||
| Random effect analysis | ||||||||
| Child level variance | π2/3 ≈ 3.29 | π2/3 ≈ 3.29 | π2/3 ≈ 3.29 | |||||
| Community level variance (intercept) | - | 0.08 (SE = 0.04) | 0.13(SE = 0.10) | |||||
| Community level variance (slope: rural–urban) | - | - | 0.03(SE = 0.12) | |||||
- Abbreviations: AIC, Akaike information criteria; AOR, adjusted odds ratio; AUROCC, area under the operating receiver characteristics curve; BIC, Bayesian information criteria; CI, confidence interval; COR, crude odds ratio; SE, standard error.
The study found that children in Central (aOR: 2.47 at 95% CI 1.42–4.29; p = 0.001) and Upper East (aOR: 2.07 at 95% CI 1.29–3.32; p = 0.003) regions were 2.47 and 2.07 times more likely to be anemic compared to children who were in Upper West region respectively. Also, male children under-5 years were 20% more likely to be anemic compared to female children under-5 years (aOR: 1.20 at 95% CI 1.07–1.36; p = 0.003). Infants between 6 and 12 months old were 3.6 times more likely to be anemic compared to children who were 4 years old (aOR: 3.59 at 95% CI 2.54–5.08; p < 0.001). Second-born children were 40% more likely to be anemic compared with first-born children (aOR: 1.40, 95% CI: 1.12–1.75, p = 0.003). Children born to adolescent mothers had over two times high odds of anemia compared with children born to mothers in the age range 40-49 years (aOR: 2.21, 95% CI: 1.36–3.57, p = 0.001).
Additionally, children who tested positive for malaria in the last 2 weeks before the survey were 53% more likely to be anemic compared with children who had no malaria (aOR: 1.53 at 95% CI 1.13–2.06; p = 0.006). The odds of anemia among children were 45% and 49% higher for mothers who were registered, but not covered with insurance (aOR: 1.45, 95% CI: 1.21–1.74, p < 0.001) and those who were not registered at all (aOR: 1.49, 95% CI: 1.15–1.93, p = 0.002). Also, children born to the poorest households were about three times more likely to be anemic than children in richer households (aOR: 2.97 at 95% CI 1.63–5.42; p < 0.001) (Table 3).
Figure 2 shows the predictive ability of the fitted models to correctly predict under-five anemia prevalence among children under-five in Ghana. The predictive ability of the single-level model was 71% (69, 73%), 73% (0.71, 0.74%) for the random intercept multilevel model, and 73% (0.71, 0.75%) for the random slope multilevel model. Thus, both the random intercept and the random slope multilevel models provided similar predictive ability. However, based on the principle of parsimony, the random intercept multilevel model was preffered.
4 DISCUSSION
4.1 Principal findings
This study employed both random intercept and random slope multilevel logistic regression models to quantify unobserved community-level differences in anemia and to simultaneously determine critical predictors of anemia among 2434 children under five and found substantial unobserved community-level differences in the probability of anemia among this group of children. Thus, the probability of developing anemia differs from one community to another in the country, suggesting the need for targeted community-level public health interventions aimed at reducing anemia within communities rather than universal interventions. We did not find the effect of rural/urban residence covariate on anemia to significantly differ from one community to another in Ghana. The risk of anemia was found to be higher in children below 2 years, male children, children born to adolescent mothers, children born to non-Christian homes, children whose mothers were not covered with health insurance, leaving in either upper west or central region and children born to families of poorer households.
4.2 Interpretation
The findings revealed that anemia was prevalent among 54% of children under five, an estimate lower than 76.6% in Sub-Sahara Africa,33 but reasonably higher in other sub-Sahara Africa countries13, 34 and global estimates of 40.0% in 2019.16, 35 Although the World Health Organization considers anemia prevalence greater than 40% as a severe public health problem, findings from this study and another study showed that Ghana's anemia prevalence in children under-5 years has reduced from 78% in 2008 to 66% in 2014 and further to 54% in 2019 which implies anemia intervention control programs implemented are gradually influencing the population.36 This shows that although Ghana's anemia prevalence is lower than most developing countries,37 it is still a severe public health concern, which needs specific geographic, behavioral, community, and individual interventions to reduce it drastically.
Also, older children ( > 2 years) were at a lesser risk of anemia compared with infants, as shown in this study. This is in line with several studies that reported on high prevalence among infants and children under 2 years compared to older children.35, 38 The higher prevalence of anemia is likely to be the effect of monotonous diets, poor feeding habits during weaning periods worsen the problem of anemia as breast milk is replaced with meals that lack iron, vitamins, and other essential nutrients. Also, during infancy, these children are more vulnerable to diseases because they have less developed immune systems, and this makes them more likely to be susceptible to anemia which is largely caused by low levels of iron. Although babies are born with iron stored in their bodies, because of their rapid growth, they need to absorb a lot of iron each day. Iron deficiency anemia most commonly affects babies 9–24 months old.
Furthermore, our results showed that the risk of anemia when a child has malaria is higher, which is consistent with these studies.28, 32, 33, 36 The main approach to preventing anemia in children under five is through malaria prevention, diagnoses, and treatment.36 Several studies have confirmed the presence of malaria in children causes severe anemia, which may lead cognitive issues and even death.34 In some parts of Ghana, sanitation issues, vegetation, rainfall, and precipitation contribute to the formation of natural habitats for mosquitoes, thereby increasing children's risk of malaria in such regions.35
A study conducted across multiple countries in sub-Sahara Africa confirms our findings that females were at lower risk of anemia compared to the male child, although significant variations were not observed between the two genders in a study analysis of three national demographic health survey data from Ghana.7, 33, 39 The prevalence of anemia was higher in males than females this is similar in these studies,33, 34, 37-39 where male children less than 60 months older exhibited a higher fold of being diagnosed with anemia than females. The reasons being male children have a higher pre-natal and post-natal growth.40 Conversely at puberty anemia is more prevalent in females than males due to menstruation, but that difference couldn't be established in a study elsewhere.39
Further, our findings of a higher risk of anemia among children in poorer households is also supported by multiple literature.33, 41-43 Children from poorer households may be fed monotonous, competition for food, insufficient meals per day, and undernutritious diets that wouldn't contain the essential nutrients to prevent anemia, hence they are at higher risk of anemia compared with children from richer homes who because of the availability of resources may be fed with right proportions of healthy meals.7
In addition, an increase in household size was found to be associated with an increased risk of anemia among children. This is supported by findings from elsewhere in Ethiopia41 and a systematic review in Africa.13 Reducing household crowding, and improving toilet and water facilities helped in reducing the risk of anemia in children under-5 years.34
Although the univariate analysis showed that anemia was more prevalent in the rural areas compared to the urban areas, both the fixed and multilevel multivariable analysis did not show differentials in anemia prevalence between the rural and urban areas. This finding was also observed in other literature where residence was no longer significant after adjusting for other factors.7 This suggests that implementing interventions in just rural areas is not the best approach but instead, it is imperative we go further to identify what demographic of children is associated with anemia within these rural areas. This, however, may not be the same for other settings.41 In a study by Gebreweld et al.,35 children under five urban dwellers were 1.8 times more likely to be anemic than children under five rural dwellers.35
4.3 Strengths of the study
The key strength of this study is the utilization of the random intercept and the random slope multilevel models, which permit drawing conclusions about significant differences in the probability of anemia in children across communities and the impact of a covariate on anemia across communities, respectively, and allow for correct estimation of model parameters and correct statistical inference and policy decisions. The study simultaneously examined over 20 critical predictors of anemia in this group of children under the multilevel modeling framework and highlighted significant predictors. Our modeling approach is an improvement on previous studies that examined factors associated with anemia among children under-fives in Ghana and ignored the hierarchical structure of the datasets used in their study. For example, Klu et al.,44, 45 used data from the 2019 Ghana Malaria Indicator Survey where children are nested within communities (cluster) but did not consider the clustering of observations on these children from the same community, which could lead to spurious statistical significance and its associated incorrect statistical inference and misleading policy decisions.46 The population-level nature of the data allows making inferences to cover all children under-fives in Ghana and in other similar settings.
4.4 Limitation of the data
The study used a cross-sectional study design hence interpretation of results should be done in the context of association and not causality. Also, given that the measurement was among only children alive at the time of the survey, the results are likely to be biased, especially for the exclusion of children who died due to anemia-related causes. The data is also limited in terms of the availability of other variables that are likely to impact the hemoglobin level such as uptake of iron supplementation, diarrhea among children, and others.
5 CONCLUSION
Prevalence of anemia among children remains high in Ghana, especially among poorer households, infants, and children of younger mothers. As Ghana is assiduously working hard towards achieving the majority of the SDGs by 2030, the identified factors in this study could be considered as part of an overall strategy aimed at addressing the anemia problem in the country. Also, the type of intervention and intervention allocation strategies should be reorganized and targeted at communities to attain a reduced prevalence of anemia in children under-5 years in the country. Our finding that children from one community were more likely to be anemic compared to children from another community suggests the need to search for other factors not considered in this study that might help to further understand why children from certain communities have had higher chances of being anemic than their counterparts from other communities in this population.
AUTHOR CONTRIBUTIONS
Justice M. K. Aheto: Conceptualization; data curation; formal analysis; investigation; methodology; project administration; resources; software; supervision; validation; visualization; writing—original draft; writing—review & editing. Yakubu Alhassan: Formal analysis; investigation; software; validation; visualization; writing—original draft; writing—review & editing. Adikwor E. Puplampu: Investigation; writing—original draft; writing—review & editing. Julius K. Boglo: Investigation; writing—original draft; writing—review & editing. Kojo M. Sedzro: Investigation; writing—original draft; writing—review & editing.
ACKNOWLEDGMENTS
We thank the participants for taking part in the study and making it a success. The authors declare that this study received no outside funding.
CONFLICT OF INTEREST STATEMENT
Justice Moses K. Aheto is an Editorial Board member of Health Science Reports and coauthor of this article. He was excluded from editorial decision-making related to the acceptance of this article for publication in the journal. All other authors declare that they have no conflict of interest.
TRANSPARENCY STATEMENT
The lead author Justice Moses K. Aheto affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
DATA AVAILABILITY STATEMENT
The datasets generated and/or analyzed during the current study are available from the MEASURE DHS Program website http://dhsprogram.com/data/available-datasets.cfm.




