A clinician's guide to gallstones and common bile duct (CBD): A study protocol for a systematic review and evidence-based recommendations
Abstract
Background and Aims
Gallstones are one of the most common and costly diseases of the gastrointestinal tract and occur when a combination of deposits consisting of fat or minerals accumulate in the gallbladder or common bile duct (CBD). This paper provides a comprehensive review of gallstone epidemiology, diagnosis, and management, focusing on current clinical guidelines and evidence-based approaches.
Methods
A systematic literature review gathered information from various sources, including PubMed, Trip, Google Scholar, Clinical Key, and reputable medical association websites. Keywords related to gallstones, CBD stones, cholelithiasis, choledocholithiasis, and guidelines were used to extract relevant recommendations. Expert consultations and consensus meetings localized the recommendations based on the target population and available resources.
Results
The paper discusses demographic factors, dietary habits, and lifestyle influences contributing to gallstone formation. Gallstones are categorized into cholesterol and pigment types, with varying prevalences across regions. Many individuals with gallstones remain asymptomatic, but complications can lead to serious and potentially life-threatening conditions. Diagnosis relies on history, physical examination, laboratory tests, and transabdominal ultrasound. Specific predictive factors help categorize patients into high, moderate, or low probability groups for CBD stones.
Conclusion
Evidence-based recommendations for gallstone diagnosis and management are presented, emphasizing individualized treatment plans. Surgical interventions, nonsurgical treatments like oral litholysis with UDCA, and stenting are discussed. The management of gallstones in pregnant women is also addressed, considering the potential risks and appropriate treatment options during pregnancy.
Key points
-
Gallstones are a prevalent and costly gastrointestinal disease caused by fat or mineral deposits in the gallbladder or common bile duct (CBD).
-
This paper reviews gallstone epidemiology, diagnosis, and management based on clinical guidelines and evidence.
-
Predictive factors help categorize patients into high, moderate, or low risk for CBD stones.
1 INTRODUCTION
Cholelithiasis or gallstones is characterized by the accumulation of sediments consisting of fatty or mineral deposits in the gallbladder or common bile duct (CBD). Demographic conditions, diet, lifestyle, and other metabolic conditions are among the factors and risk factors for gallstones (Table 1).1-3 Gallstones are divided into two categories in terms of constituent elements: cholesterol (yellow) and pigment gallstones (Black and brown). Various other elements such as iron, phosphorus, carbonate, protein, carbohydrates, mucus, and cell debris form the composition of gallstones.4 Cholesterol and black pigment gallstones are commonly formed in the gallbladder, while brown pigment gallstones are mainly in the bile duct.3 Cholesterol gallstones account for 80%–90% of all gallstones in European and American countries, whereas pigment gallstones are mainly reported in Asian countries.5
| Risk factors |
|---|
| Population cognitive |
| Family history, female gender, aging, certain races |
| Diet |
| High-calorie and carbohydrates refined diet, unsaturated-fat and fiber diet, complete intravenous (i.v.) nutrition and TPN |
| Life style |
| Low physical activity, fast food consumption, obesity, pregnancy, long fasting, rapid weight loss |
| Other conditions |
| Alcoholic cirrhosis, diabetes mellitus, dyslipidemia, estrogen therapy or oral contraceptives, hyperinsulinemia, metabolic syndrome |
Gallstone-related disease refers to cases that are due to the presence of asymptomatic and symptomatic stones in the gallbladder or CBD presented with similar symptoms and/or complications.6 Most people with gallstones are asymptomatic and diagnosed accidentally while examining other problems. Only in a small number of people with gallstones, existing stones irritate the gallbladder or block part of the biliary system, and this can be accompanied by symptoms such as pain, infection, and inflammation. If left untreated, gallstones can cause more serious complications and in some cases be life-threatening.2
Choledocholithiasis, also known as CBD stones, are primary or secondary according to stone origin. Primary stones are formed in the bile duct and these stones are mainly composed of bilirubin and are probably associated with biliary stasis and infection. Secondary stones form in the gallbladder that moves into the CBD. In such cases, the biochemical composition of the CBD stones is quite similar to that of gallstones, which are mainly composed of cholesterol.7, 8 CBD stones may be asymptomatic or symptomatic and may be associated with symptoms such as colic pain, obstructive jaundice, cholangitis, and gallstone-induced pancreatitis.9, 10
1.1 Epidemiology of the disease
More than 98% of all bile duct disorders result from gallstones. Cholelithiasis is one of the most high-risk gastrointestinal disorders which has high health care costs (~6.5 billion dollars/year). About 10%–15% of gallstone patients have both gallbladder and CBD stones.8
Geography and ethnicity have a significant effect on the prevalence of gallstones and stone-type formation.11 Gallstones are highly prevalent in developed countries, affecting 10%–15% of the population of America and developed countries12 and 10% of the population in Asian countries and 4%–12% in the Middle East have gallstones. The prevalence of asymptomatic gallstones is reported as 0.8% in North of Iran, 4.7% in southern Iran, and 4.4% in eastern Iran.13
The history of asymptomatic gallstones suggests that a large number of affected individuals will remain asymptomatic throughout life, and 10%–25% will develop symptoms such as colic. The annual risk of pain is 2%–3% and for severe complications is 1%–2%.12 Although 0.6% of deaths are caused by the gallbladder, the high burden of the disease indicates alarming mortality. It was estimated that 1092 deaths due to gallstones occurred in the United States in 2004. Nowadays, cholecystostomy is the most common elective abdominal surgery, and more than 750,000 surgeries are performed annually in the United States.11 Although the mortality rate of this disease is low, its high rate of complications imposes a financial burden. According to the results of studies, 21%–34% of CBD stones move spontaneously, and these stones increase the risk of pancreatitis or cholangitis if the distal duct is blocked. Given that biliary pancreatitis and cholangitis may be life-threatening conditions, it is generally recommended to remove the CBD stones.14, 15
Screening and identifying people who need to be treated or followed up clinically is achieved by physicians and general practitioners. Surgical procedures and consultation for treatment are performed and coordinated with internal medicine specialists and gastroenterologists. Clinical guidelines with strong expertise can be used to help standardize health care in this field. The clinical guide seeks to determine general and important policies for this disease and to modify its screening, diagnostic, and managerial approaches.
To date, no systemized guidelines are found for gallstones with severe complications, for its diagnosis, treatment, and management. Commonly invasive procedures like endoscopy or exploratory laparotomy, in some cases, are performed for diagnosis and surgery for the treatment, however, guidelines regarding the timing of these procedures remain questioned.
2 METHOD
The search engines of PubMed, Trip, Google Scholar, Clinical Key, and the websites of scientific and reputable associations such as AASLD, ESAL, ESGE, ASGE, ACG, AGA, and UEG were examined with the following keywords. Guidelines were compiled and published in English and in full. Simultaneously, medical literature was examined to find the best evidence (Table 2).
| No. | Guide reference | Internet address |
|---|---|---|
| 1 | PubMed | https://www.ncbi.nlm.nih.gov/pubmed/ |
| 2 | NICE guidelines | https://www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/nice-guidelines |
| 3 | Trip database | https://www.tripdatabase.com/ |
| 4 | Google scholar | https://scholar.google.com/ |
| 5 | Clinical Key | https://www.clinicalkey.com/#!/browse/guidelines |
| 6 | American Association for the Study of Liver disease guideline (AASLD) | https://www.aasld.org/publications/practice-guidelines |
| 7 | European Association for the Study of the Liver (EASL) | https://easl.eu/publications/clinical-practice-guidelines/ |
| 8 | European Society of Gastrointestinal Endoscopy (ESGE) | https://www.esge.com/publications/guidelines/ |
| 9 | American Society for Gastrointestinal Endoscopy (ASGE) | https://www.asge.org/home/guidelines |
| 10 | American College of Gastroenterology (ACG) | https://gi.org/guidelines/ |
| 11 | United European Gastroenterology (UEG) | https://www.ueg.eu/publications/ |
| 12 | American Gastroenterological Association (AGA) | https://www.gastro.org/guidelines |
| 13 | American Academy of Family Physician (AAFP) | https://www.aafp.org/journals/afp.html |
2.1 Keywords under study
Gallstone, CBD stone, CBD stones, Cholelithiasis, Choledocholithiasis, Guideline Extraction of recommendations and clinical solutions were done based on different guidelines and each was localized according to the specific situation and conditions of the target population and the conditions in which the solution should be operational and executive conditions such as health, cultural and economic conditions. Then, all the recommendations and solutions in the field of diagnostic and treatment methods were presented based on consultation sessions with experts and finally the consensus of experts consisting of members of the Isfahan Association of Gastroenterology & Liver.
After the final approval of the clinical guide, it was necessary to hold a meeting with the partner team every 2 years to research and review the resources. The duty of the partner team in this meeting was to provide the latest evidence and scientific information and make changes if approved by the other members. After the work was completed, the clinical guide was reviewed by three experienced liver gastroenterologists from other universities (Table 3a–f).
| a. Level of evidence | |
|---|---|
| 1 | Evidence from the meta-analysis of controlled randomized studies (a) or at least from a randomized controlled study (b). |
| 2 | Evidence from at least one nonrandomized controlled study (a). |
| 3 | Evidence from well-designed nonempirical studies such as comparative studies, a relational studies and rare items. |
| 4 | Evidence from the committee of experts or the opinions and experiences of experts. |
| b. Rating recommendations | |
|---|---|
| a | Recommendations based on randomized controlled studies and quality and coherent studies. |
| b | Recommendations based on coherent and good design but nonrandom. |
| c | Recommendations based cases which despite the lack of studies has a coherent and hiugh quality design. |
| c. Guideline recommendations | ||
|---|---|---|
| Level of evidence/grading of recommendations | Recommendations | No |
| 1/a | The term gallstone disease refer to diseases caused by symptomatic or asymptomat stones in the gallbladder or common bile duct, symptoms or complications caused by it. | 1 |
| 1/a | The initial evaluation of patients with suspected gallstone and common bile duct stones based on history, physical examination, laboratory tests and ultrasound. | 2 |
| 1/a | In case of no diagnosis with the said items, but still had doubts about gallstones and common bile duct stones, MRCP, EUS, And ERCP be used. | 3 |
| 2/b | Pain in the epigastrium or RUQ is reported in the history of patients with suspected biliary pain based on ROME Ⅳ. The duration of pain equal to or greater than 30 min, the pain is intermittent, but is not daily and is ascending to a constant level and is severe enough to require hospitalization, the pain do not respond to excretion and antacids. | 4 |
| 2/c | Pain due to gallstones (nonbiliary colic) lasts more than 6 h. | 5 |
| 1/c | Biliary colic is a noncolic pain whivh in the epigastric or RUQ may radiated to the back or right shoulder and may be accompanied by sweating, nausea and vomiting. Pain duration is often less than 30 min and the pain lasts more than 6 h. | 6 |
| 1/a | In biliary colic, CBC, Aminotransferases, Bill, ALP, Amylase and lipase tests are normal. | 7 |
| 1/a | Acute Choledocholithiasis is a syndrome with epigastric pain or RUQ, Fever and leukocytosis due to inflammation of the gallbladder and is usually caused by stones in the gallbladder. | 8 |
| 1/a | CBD stone pain mostly is reported in the epigastrium or RUQ and accompanied by nausea, vomiting and jaundice, pain duration is usually over 6 h and fever is also found in the presence of cholangitis. | 9 |
| 1/a | Laboratory tests, including CBC, Aminotransferases, liver function test, amylase, and lipase are checked for all patients with gallstones. | 10 |
| 2/c | Very strong predictive factors refer to the presence of common bile duct stones on transabdominal ultrasound or ascending cholangitis or bilirubin <4 mg/dL. | 11 |
| 2/c | In strong predictive factors, enlarged common bile duct (more than 6 mm in the transabdominal ultrasound) or bilirubin between 1.8 and 4 mg/dL. | 12 |
| d. Level of evidence | ||
|---|---|---|
| Level of evidence/grading of recommendations | Recommendations | No. |
| 2/c | Moderate predictive factors refers to abnormal liver biochemical tests other than bilirubin or age over 55 years or pancreatitis caused by gallstones. | 13 |
| 2/c | ERCP must be used for patients who have common bile duct stones with a probability >50% and have a very strong predictive factor or two strong predictive factor. | 14 |
| 2/c | MRCP or EUS is recommended for patients with probability of between 10% and 50% have common bile duct stones and have a strong predictive factor or at least a moderate predictive factor. | 15 |
| 1/a | MRCP (If there is no contraindication) or EUS (If available and not possible MRCP) is recommended in case of strong clinical suspicion of the presence of stones and normal transabdominal ultrasound, the presence enlarged CBD on ultrasound or abnormal liver test results. | 16 |
| 1/c | ERCP is used as diagnostic and therapeutic methods for CBD stones, but because of complications such as pancreatitis, bleeding, infection and perforation is less used as a diagnostic modality. | 17 |
| 2/a | Hydration during ERCP and Rectal NSAID are used to prevent post ERCP pancreatitis. | 18 |
| 1/a | In cases where there is the possibility of not removing the obstruction after ERCP, anti prophylactic antibiotics is given before ERCP. These cases include the cases of suspected malignancy of the liver which leads to helium obstruction, PSC and the other cases don't perform with a high probability of not removing the obstruction prophylaxis with antibiotics, ciprofloxacin 400 mg g every 8 h and amoxicillin/Clavulanic acid as an alternative, ampicillin, penicillin or ampicillin penicillin plus gentamicin can be used. | 19 |
| 1/a | During an acute biliary colic attack, the focus is on prescribing analgesics, first NSAIDs and in case of no effect or contraindication, opioids should be prescribed. | 20 |
| 2/a | The patient should be hospitalized in cases where his pain continued for more than 4 h with the possibility of other diagnosis or complications. | 21 |
| 2/a | After administration of analgesics and hydration if you suspect to acute Cholecystitis, severity of illness is estimated and the treatment to be done based on it. | 22 |
| 2/a | Mild acute Choledocholithiasis is defined as acute Choledocholithiasis in a patient with no organ dysfunction and Cholecystectomy is performed in the same bed of the patient. In this group of patients, cholecystectomy has few complications | 23 |
| 1/a | Moderate acute Choledocholithiasis is associated with no organ dysfunction but there is extensive disease in the gallbladder, disease duration of more than 72 h; and the painful mass is felt on RUQ on examination. In these cases, antibiotics may be needed and cholecystectomy should be performed immediately. Surgical complications are more common in this group of patients than mild cases. | 24 |
| e. Level of evidence | ||
|---|---|---|
| Level of evidence/grading of recommendations | Recommendations | No. |
| 1/a | There is organ damage in severe acute cholecystitis and requires supportive cares along with receiving antibiotics and emergency treatment and hospitalization in the ICU. | 25 |
| 1/a | Complicated acute cholecystitis include perforated gallbladder, gangrene, necrosis, and emphysematous cases that increase mortality in patients and are difficult to diagnose. | 26 |
| 1/a | Treatment of complicated cholecystitis is emergency cholecystectomy (if the patient is a candidate for surgery). | 27 |
| 2/b | The patient should have a cholecystectomy in cases where the patient develops analgesics-resistant abdominal pain or becomes detrroriate during hospitalization and treatment of acute cholecystitis. | 28 |
| 1/a | Cholecystectomy is not indifated in cases where the gallstone is asymptomatic, unless the stone is larger than 3 cm, there is a possibility or increased risk of cancer (associated with polyps, gallbladder anomaly and gallbladder adenoma) and porcelain gallbladder. | 29 |
| 2/a | Laparoscopic cholecystectomy is the standard treatment for gallstones. | 30 |
| 1/a | Symptomatic and asymptomatic common bile duct stones should be treated. | 31 |
| 1/a | Acute cholangitis and pancreatitis are complications of common bile duct stones that increased morbidity and mortality. | 32 |
| 1/a | The time of stone discovery (before or after cholecystectomy) is effective on the treatment of the common bile duct stone. It is preferred over endoscopic treatment (ERCP) and if surgery is not possible or unsuccessful. | 33 |
| 2/a | ERCP should be performed within 24 h of the onset of the problem in complicated common bile duct stones in the form of severe cholangitis with organ failure. Also perform emergency ERCP (within 24 h) if the severity of cholangitis is mild but does not respond to supportive care. ERCP should be performed within 24–48 h in cases where cholangitis is not severe and has responded to supportive treatment. | 34 |
| 1/a | ERCP should be performed within the first 24 h of admission in cases where gallstone pancreatitis is associated with cholangitis. | 35 |
| 2/a | Liver tests should be rechecked at 24–48 h or MRCP or EUS performed in cases where bile duct obstruction is suspected in acute pancreatitis (in the absence of cholangitis). | 36 |
| 2/a | Delayed ERCP should be performed after relieving the symptoms of pancreatitis. In case of acute pancreatitis due to gallstones and obstruction of the bile duct without cholangitis. | 37 |
| f. Level of evidence | ||
|---|---|---|
| Level of evidence/grading of recommendations | Recommendations | No. |
| 1/a | Common bile duct stones after cholecystectomy may be caused by residual stones or newly formed duct stones. Diagnosis is by patient’ history, physical examination, lab data, ultrasound, and finally MRCP or EUS. ERCP is preferred modality for treatment. | 38 |
| 1/b | biliary stents are used in cases where we suspected that the bile ducts are not clear after ERCP or have strnosis. | 39 |
| 2/b | In cases where repeated cannulation of the PD duct has been performed, in addition to hydration and rectal NSAID, a PD stent can also be used to prevent ERCP-induced pancreatitis. | 40 |
- Abbreviations: CBD, common bile duct; EUS, endoscopic ultrasound; ICU, intensive care unit; MRCP, magnetic resonance cholangiopancreatography; RUQ, right upper quadrant.
2.2 Diagnosis
Initial assessment of a patient with suspected gallstones and CBD stones is performed based on history, physical examination, laboratory test, and ultrasound. These tests and ultrasounds are available cheaply and widely. Also, these tests are recommended for patients with abdominal and gastrointestinal symptoms who have not responded to treatment, as these patients are suspected of stones.
2.3 History and physical examination (H&P)
- ❖
Pain located in the epigastric or right upper quadrant (RUQ)
- ❖
Pain duration equal to or greater than 30 min
- ❖
Recurrent symptoms occur at different intervals rather than daily
- ❖
Constant-to-increasing pain
- ❖
The severity of pain leads to hindrance in everyday activity and causes emergency visits
- ❖
There is a weak correlation between pain and bowel movements (less than 20%)
- ❖
Pain does not improve significantly with the use of antacids or by changing the position of the body (less than 20%).
- ❖
Pain with nausea and vomiting
- ❖
Pain radiating to the back or right infrascapular region
- ❖
The pain awakens the patient from sleep.16
Most patients suffer from CBD stone pain in the epigastrium or RUQ accompanied by nausea and vomiting. The pain is often longer than typical biliary colic (biliary colic pain usually resolves within 6 h) and resolves when the stone either passes spontaneously or is removed. Patients may have icterus and Courvoisier's sign on examination (palpably enlarged gallbladder, followed by gallbladder obstruction due to obstruction, which is more common in malignancies).3, 17
Also, anorexia, nausea or vomiting, fever, jaundice, and positive reaction to analgesics should be considered in reviewing patient H&P. Symptoms of ascending cholangitis include fever, jaundice, and abdominal pain (Charcot's cholangitis triad) caused by biliary and bacterial infections of the bile duct and should be cleared up immediately with intravenous antibiotics and endoscopic retrograde cholangiopancreatography (ERCP). Acute Choledocholithiasis is an inflammation of the gallbladder caused by gallbladder obstruction. The disease should be suspected in patients with fever, RUQ pain, or Murphy signs. In a morphological examination to confirm acute choledocholithiasis, the examiner touches the patient's right rib deeply with the right hand and asks the patient to take a deep breath. The sudden cessation of inspiration due to pain characterizes a positive “Murphy sign.” Patients with gallstone pancreatitis due to obstruction at the level of the edema sphincter are usually associated with epigastric pain.3, 18
2.4 Laboratory test
All patients with suspected gallstones should be evaluated based on laboratory tests, including complete blood count, liver test, aminotransferases, amylase, and lipase. In choledocholithiasis, aseptic bile duct obstruction usually occurs with biliary pain, elevated liver enzymes, normal amylase and lipase, and normal white blood cell counts. Cholangitis, as an infectious complication, is associated with obstruction of the biliary tract and is usually associated with a left-shift leukocytosis, elevated liver tests with cholestatic pattern (increased ALP and GGT), elevated levels of bilirubin (more than 2 times), and increased aminotransferase levels up to 2000 and natural amylase and lipase.
Pancreatitis, inflammation of the pancreas, can cause amylase and lipase levels to increase up to 3 times normal. Elevated values of serum alanine aminotransferase level (ALT) indicate that the origin of pancreatitis may be gallstones. The amount of bilirubin and white blood cells can be normal or abnormal, depending on the location and severity of the blockage and the amount of infection. Leukocytosis is also common in acute choledocholithiasis where total bilirubin is usually normal or slightly elevated, unless in co-choledocholithiasis.18
2.5 Transabdominal ultrasound
Ultrasound of RUQ and epigastrium should be performed in patients who are suspected of stones. The accuracy of transabdominal ultrasound in the detection of gallstones is more than 95%. Elderly patients with unusual abdominal pain, immune-compromised patients with unknown sites of infection, or patients suspected of sepsis due to abdominal problems may also be evaluated by transabdominal ultrasound, due to the possible presence of gallstones. The stones appear as echogenic focus with a posterior shadowing without a signal on transabdominal ultrasound. Also, polyps and bile sludge in ultrasound are seen as echogenic foci without shadowing. The only difference is that biliary sludge moves but the polyp is fixed. For this reason, the patient's ultrasound is performed in different positions such as lying on his back, turning to the left, or standing.3 No gallstones are seen in imaging, in up to 20% of the patients with symptoms typical of biliary colic, possibly because of the small size or composition of the stone.1
2.6 Useful predictive factors of CBD stones
There are three predictive factors of CBD stones categorized as very strong, strong, and moderate predictive factors (Table 4). Very strong predictive factors include CBD stone seen on transabdominal ultrasound/ascending cholangitis, bilirubin >4 mg/dL. Strong predictive factors are enlarged CBD stones in transabdominal ultrasound (more than 6 mm on trans-abdominal ultrasound) or bilirubin between 1.8 and 4 mg/dL and moderate predictive factors are abnormal liver test (AST, ALP, and ALT) excluding bilirubin or age over 55 or pancreatitis caused by gallstones.10, 19, 20
| Predicting the common bile duct stones | |
| The presence of common bile duct stones inside the common bile duct (CBD) | Very strong |
| Ascending cholangitis | |
| Bilirubin more than 4 mg per deciliter | |
| Enlarged common bile duct on ultrasound (more than 6 mm on transabdominal ultrasound) | Strong |
| Bilirubin 1.8–4 mg per deciliter | |
| Abnormal liver test except for bilirubin | Moderate |
| Age over 55 years | |
| Pancreatitis caused by gallstones | |
| Possibility of common bile duct stone based on clinical predictions | |
| The presence of at least one very strong predictor or two strong predictors | High |
| The presence of a strong predictor or any moderate predictor | Intermediate |
| No clinical predictor | Low |
The results of tests and ultrasound classify patients into three categories: high, moderate, and low probability of having common gallstones (Table 4). Patients with a high probability (i.e., more than 50% likely to have common gallstones) have a very strong predictive factor or two strong predictive factors that direct ERCP must be performed on these patients. Patients with a moderate probability (i.e., a 10%–50% chance of having a CBD stone) have a strong predictive factor or at least a moderate predictive factor in which magnetic resonance cholangiopancreatography (MRCP) or endoscopic ultrasound (EUS) should be performed for better diagnosis. Patients with a low probability (i.e., less than a 10% chance of having a CBD stone) refer to those for whom there is no predictive factor and should undergo cholecystectomy without further evaluation18, 21 (Table 5).
| Laboratory test | Physical examination | Complications |
|---|---|---|
| High levels of liver enzymes | Biliary colic | Choledocholithiasis |
| Normal amylase and lipase | ||
| Count of white blood | ||
| Leukocytosis is common | Fever, RUQ sign, pain in Murphy | Acute Cholecystitis |
| Total bilirubin is usually normal or slightly elevated | ||
| Left shift leukocytosis | Fever, jaundice and pain (Charcot's cholangitis triad) | Cholangitis |
| Elevated enzymes of the liver. | ||
| Elevated bilirubin greater than 2 | ||
| Normal amylase and lipase | ||
| Amylase and lipase 3 times higher than normal | Epigastric pain | Pancreatitis |
| Elevated alanine aminotransferase (ALT) more than 150 | ||
| Bilirubin and blood cells, white blood depending on the site and severity of obstruction, and the infection can be normal or abnormal |
2.7 MRCP and EUS
It is necessary to perform EUS or MRCP in case of strong clinical suspicion of gallstones and normal abdominal ultrasound.3 In the second stage of diagnosis, MRCP or EUS is also performed where the presence of the enlarged CBD in ultrasound or the liver test results are abnormal. The diagnostic accuracy of EUS and MRCP for CBDs has been high in studies (sensitivity and specificity above 90%). Different considerations should be considered to choose one of these two methods. Some of the most important advantages of MRCP include being Noninvasive, no need for sedation, and showing biliary tree anatomy.
One of the most important advantages of EUS over MRCP is that if a person has a CBD stone, ERCP can be performed in the same session after EUS. Other advantages of EUS include the ability to perform for patients with intracranial aneurysm clips, pacemakers, mechanical heart valves, and obese patients with claustrophobia. However, it is more aggressive than MRCP and requires sedation, and a skilled specialist to perform it.2, 6, 22
According to the guideline, MRCP is safer and more acceptable than EUS in most cases. Also, EUS, like MRCP, is not available everywhere.22 Patients with CBD stones with positive EUS or MRCP should undergo ERCP or surgery for the removal of CBD stones, and there is no need for invasive tests for people with negative EUS or MRCP. However, cost, the prevalence of CBD stones, center resources, and specialist skills must be considered.21
2.8 ERCP
ERCP is an endoscopic technique in which an upper endoscope with a side view is inserted through the mouth and then guided into the duodenum that allows instruments to be transferred to the bile duct and pancreas. ERCP is considered a gold standard for the diagnosis and is more aggressive than MRCP and requires sedation. The benefits of ERCP over surgical treatment are well documented; however, there are significant risks of short-term complications such as pancreatitis, bleeding following sphincterotomy, infection, and perforation. Due to the associated complications and costs, ERCP should be performed in patients with a high probability (Table 6) of CBD stones.15, 21
| MRCP |
| Advantages |
| nonaggressive |
| Intravenous contrast is usually given, but not necessary |
| No need for sedatives |
| It is available widely |
| Showing all biliary anatomy |
| Suitable for altered anatomy |
| Disadvantages |
| Low sensitively for small stones (smaller than 5) |
| Unsuitable for patients with intracranial aneurysm clips, pacemaker, mechanical heart valves, and claustrophobia |
| EUS |
| Advantages |
| Higher accuracy |
| Diagnosis of biliary sludge is possible |
| High resolution images compared to MRCP |
| Possibility to perform ERCP For the patient in the same session |
| It can be used patients with intracranial aneurysm clips, pacemaker, mechanical heart valves and claustrophobia |
| Disadvantages |
| More aggressive than MRCP |
| There is need for sedation |
| Complications associated with sedation and endoscopy |
| Restrictions on access to equipment and trained endosonographers |
| Impossible or abundant limitation in cases of altered anatomy |
- Abbreviations: EUS, endoscopic ultrasound; MRCP, magnetic resonance cholangiopancreatography.
ERCP is often associated with bacteremia, which is typically transient. Antibiotic prophylaxis can reduce bacteremia. It is considered unnecessary to prescribe antibiotic prophylaxis to all patients undergoing ERCP, unless there is cholangitis, pancreatic cysts, patient is immunodeficient, or incomplete biliary drainage is predicted. All patients undergoing ERCP should receive prophylactic drugs such as indomethacin or rectal diclofenac after ERCP due to the risk of pancreatitis.10, 12
2.9 Treatment of gallstones and CBD stones
Pain relief is targeted during an acute biliary colic attack. NSAIDs are used to start treatment, and opioids can be used if significant pain relief is not achieved or there is a contraindication. The pain usually subsides within 10–30 min and the patient can be discharged with oral analgesia, and if it recurs, cholecystectomy is performed for the patient. The patient is hospitalized if the pain does not subside within 4 h, as the patient is more likely to have complications.23 There is no need for treatment for the majority of asymptomatic patients and the expected treatment is used. Unless there are the following cases, which increase the risk of fatal complications: (1) Cases in which the risk of cancer increases, such as gallbladder anomalies, gallbladder adenomas, and porcelain gallbladder; (2) Gallstones larger than 3 cm.24
2.9.1 Pain control
For the treatment of acute biliary colic, pain control is primarily used with Nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids. NSAIDs (such as diclofenac, ketoprofen, and indomethacin) are preferred by most patients due to their fewer side effects. Contraindications should be considered which include a history of hypersensitivity/severe allergic reactions to NSAIDs as well as renal impairment and gastrointestinal complications. Opioids (such as pethidine) may be used for severe pain. However, according to the results of comparative studies, NSAIDs are faster and more effective in pain relief. Also, according to Recent RCTs, the risk of acute choledocholithiasis during biliary colic can be reduced by NSAIDs.1, 3
2.9.2 Antibiotics
- 1.
Grade I (mild acute Choledocholithiasis) is defined as acute choledocholithiasis in a patient with no organ dysfunction and limited disease in the gallbladder, making cholecystectomy a low-risk procedure.
- 2.
Grade II (moderate acute choledocholithiasis) is associated with no organ dysfunction but there is an extensive disease in the gallbladder, resulting in difficulty in safely performing cholecystectomy. Grade II disease is usually characterized by an elevated white blood cell count, palpable and tender mass in the right upper abdominal quadrant, disease duration of more than 72 h, and imaging studies indicating significant inflammatory changes in the gallbladder.
- 3.
Grade III (severe acute choledocholithiasis) is defined as acute choledocholithiasis with organ dysfunction. Acute choledocholithiasis is associated with dysfunction of any one of the following organs/systems: cardiovascular (hypotension requiring treatment with dopamine >5 mg/kg/min (body weight) or any dose of norepinephrine), Neurological (decreased level of consciousness), respiratory (PaO2/FiO2 <300), Renal (oliguria, creatinine >2.0 mg/dL), hepatic (PT-INR >1.5), and hematologic (platelet count <100,000/mL).
The community-acquired antibiotic regimen for low-risk acute choledocholithiasis includes piperacillin-tazobactam, cefazolin or ceftriaxone, safertaxime, or ciprofloxacin, or levofloxacin, and metronidazole. The community-acquired antibiotic regimen for high-risk acute choledocholithiasis is imipenem, meropenem, and piperacillin—tazobactam, cefepime, ceftazidime, and metronidazole. The hospital-acquired antibiotic regimen is similar to a community-acquired regimen with ampicillin or vancomycin.25
2.9.3 Surgery
- A.
Cholecystectomy: Laparoscopic cholecystectomy is recommended currently as standard procedure for all patients with CBD stones and symptomatic gallbladder, except for those who are not candidates for surgery (such as gallbladder cancer, anesthesia, and coagulation-related problems).22 In industrialized countries, cholecystectomy is considered the most common abdominal surgery, so about 900,000 surgeries are performed in Europe and the United States per year.1, 9 According to the results of comparison of open cholecystectomy and laparoscopy, laparoscopy is generally expected to reduce pain in incision sites, length of hospital stay, shorten recovery period, and improve the quality of life.26
- B.
It is recommended to perform cholecystectomy for cases where surgery is possible. It should be performed in the same hospital or if the patient is discharged within 2 weeks thereafter, immediately after elimination of acute pancreatitis caused by gallstones.22, 27 The time of surgery is expressed as early cholecystectomy (EC) or delayed cholecystectomy (DC) in patients with acute choledocholithiasis. EC should be performed within 24, 48, or 72 h or 1 week of the onset of symptoms, and DC should be performed within 6 weeks of the onset of symptoms.2, 18, 26 Also, choledocholithiasis is performed in patients with co-occurrence of gallstones and CBD stones. Primary laparoscopic cholecystectomy should be performed within 72 h after ERCP.3 Surgical risk should be calculated in patients with acute cholecystitis-containing stones. Emergency surgery is required in a small number of patients. These include:
- 1.
Complicated cholecystitis: This includes perforated gallbladder, gangrenous gallbladder with necrosis, and emphysema. The patient may die if emergency surgery is not performed in these cases. It is difficult to diagnose necrosis and gangrene by imaging the gallbladder.27 Gangrene and necrosis should be suspected in these cases: old age, male gender, coronary heart disease, diabetes mellitus, presence of abdominal tachycardia on examination, leukocytosis, increased CRP, increased bilirubin, urea, and creatinine, increase the thickness of the gallbladder and the accumulation of fluid around the gallbladder in Imaging.
- 2.
In cases where the disease progresses and the person becomes ill during supportive treatment, including severe pain that does not respond to analgesic therapy, fever, and unstable hemodynamics.28
- C.
Diagnosis of stones after cholecystectomy: CBD stones after cholecystectomy can be caused by the movement of the stone from the gallbladder, an undiagnosed stone during surgery, or usually a stone that has just formed in the CBD. The diagnosis of choledocholithiasis is slightly different in patients with previous cholecystectomy. Patients with choledocholithiasis are very unlikely to have normal aminotransferases and ultrasound. The incidence of choledocholithiasis after initial evaluation is from 33% to 43%. For the diagnosis of choledocholithiasis in this group of patients, MRCP and EUS are preferred over ERCP due to their low side effects.3, 10
- 3.
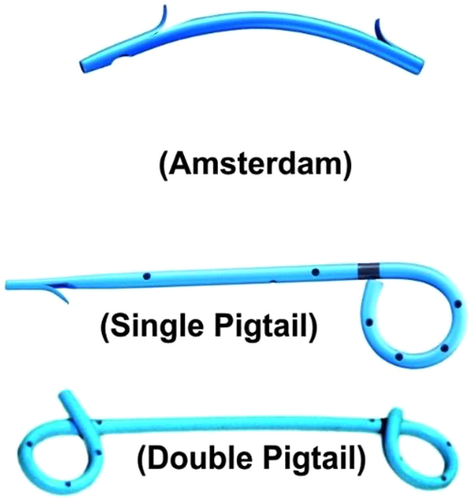
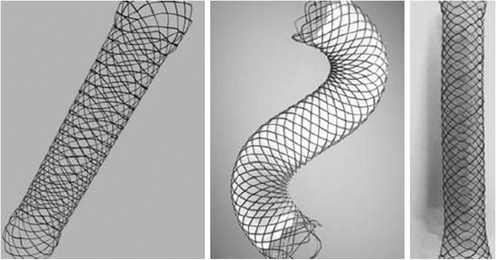
Stenting: Biliary and pancreatic stents are plastic tubular devices, composed of polyethylene, polyurethane, or Teflon. Stent French diameter and length range from 5 to 12 Fr and 1 to 18 cm, respectively. Pancreatic plastic stents are made of polyethylene and have a French diameter of 3–11.5 and a length of 2–25 cm. There are side holes in most plastic stents to help maintain bile or pancreatic flow if the end of the stent is blocked by bile or food, however, side holes along the stent axis can cause sludge formation. Plastic stents are found in three forms of Amsterdam, single pigtail or double pigtail (Figure 1). Metal stents were developed to increase the diameter of the stent, leading to a shorter stent opening time and more frequent stent occlusion. Metal stents are used for patients with biliary or pancreatic cancer who cannot have surgery. Metal stent diameter and length vary from 6 to 10 mm and 4 to 12 cm, respectively (Figure 2). These stents are composed of stainless steel or a variety of metal alloys, such as nitinol. These stents can be used in benign and malignant biliary diseases, bile leakage, pancreatic leakage or fistula, pancreatic stenosis, chronic pancreatitis, bile duct stones, and pancreatitis after ERCP29, 30 (Figure 2).
A biliary stent, also known as a bile duct stent, is used for biliary drainage as a temporary treatment or procedure until endoscopy or surgery if bile duct cleansing has not been performed by ERCP.2, 6 A common finding in patients with CBD stones is bacterial infection of the gallbladder, and incomplete bile duct clearance that may put patients at risk for cholangitis, therefore, the use of short-term stents in this group of patients is of utmost importance. The use of pancreatic stents is recommended in addition to rectal NSAID administration in patients at high risk for pancreatitis after ERCP due to frequent cannulation of the pancreatic duct. Long-term biliary stents as the only treatment for CBD stones should be used only for a group of patients with low life expectancy or high surgical risk.22, 31
2.9.4 Nonsurgical treatment of gallstones
- A.
UDCA: Noninvasive nonsurgical treatment for cholesterol gallstones is still performed by oral litholysis with biliary acids. UDCA is a biliary salt that reduces cholesterol secretion in the bile and increases cholesterol solubility and may improve gallbladder drainage. According to the results of different studies, treatment with UDCA leads to the dissolution of cholesterol gallstones. It has been concluded that bile acid therapy may inhibit gallstone symptoms and complications even in patients with incomplete gallstone dissolution.32, 33 To know the effectiveness of UDCA, before using UDCA, it is better to examine the gallstones by computerized tomography (CT) imaging, oral cholecystography, or cholecystography to determine the solubility. A stone with a lower density in CT and floating probably has more cholesterol and is suitable for UDCA treatment (density less than 75 Hounsfield).34 UDCA can be used to treat the following: stone size less than 1 cm, minimal calcification, mild symptoms, open septic duct, and a suitable concentration of gallbladder. The recommended dose of UDCA for gallstones is 8–10 mg/kg per day in two or three doses. Ultrasound every 6–12 months is recommended for these patients to monitor the treatment, and after the stone disappears the duration of drug administration is up to 6 months.35
Only a small number of patients (<10% of total) can be treated with systemic dissolution therapy using UDCA, though gallstones are composed mainly of cholesterol. It is reported that the dissolution rate is 30%–60% (about a 1 mm decrease in stone diameter per month), although the initial diameter of the gallstone is considered the most effective factor on the dissolution rate. Biliary sludge has been considered another therapeutic target of UDCA. Formation of sludge in the biliary system can be accelerated for example by rapid weight loss, pregnancy, total parenteral nutrition, and solid organ transplantation. A clinical study has reported the beneficial effect of UDCA to prevent gallstones or biliary sludge-related acute idiopathic pancreatitis. In the study, UDCA administration for 3–6 months prevented gallstone recurrence and more pancreatitis at 44-month follow-up.36
- B.
Cholecystostomy: Cutaneous cholecystostomy and stone removal are performed for high-risk surgery patients and the stones can be removed 2–3 weeks after tube insertion.37
2.9.5 Treatment of CBD stones
Endoscopic or surgical procedures are the basis of treatment and removal of stones from the biliary duct. Also, it is of utmost importance to diagnose and treat the complications of choledocholithiasis (including acute cholangitis or pancreatitis). Determination of the type of treatment depends on when the stone is discovered. ERCP is used for treatment before or after cholecystectomy. If CBD is detected during cholecystectomy surgery, ERCP during surgery or exploration during surgery is used for the biliary duct drainage.38
2.9.6 Gallstones and CBD stones in pregnant women
Gallstones are more common during pregnancy due to decreased gallbladder motility and increased biliary cholesterol saturation. Biliary diseases are associated with the risk of premature labor and mortality in both mother and baby. Supportive care often relieves symptoms in pregnant women. However, the symptoms may recur, and some mothers may need aggressive measures, such as recurrent biliary colic, acute cholecystitis, choledocholithiasis, cholangitis, and acute pancreatitis.39 Fluid therapy, nutritional support (if needed), and correction of electrolyte imbalance in pregnant women. It isn't recommended to use NSAIDs in pregnancy to relieve pain, especially after 32 weeks of pregnancy and acetaminophen can be prescribed. Prescribing drugs such as fentanyl and meperidine are allowed during pregnancy. Ampiculbactam, piperacillin-tazobactam, ceftriaxone, and metronidazole can be recommended, and clindamycin when diagnosing drug allergy. Biliary colic treatment should be supportive and cholecystectomy surgery should be performed in the second trimester if it is repeated too much. Surgery with or without ERCP should be performed with caution by specialists in complicated cases.40
AUTHOR CONTRIBUTIONS
Vahid Sebghatollahi: Conceptualization; Data curation; Formal analysis; Resources; Software; Supervision. Mohammadreza Parsa: Methodology; Project administration; Resources; Writing—original draft; Writing—review & editing. Mohammad Minakari: Formal analysis; Funding acquisition; Investigation; Supervision; Validation; Visualization. Saleh Azadbakht: Formal analysis; Funding acquisition; Investigation; Supervision; Validation; Visualization.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
TRANSPARENCY STATEMENT
The lead author Saleh Azadbakht affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
DATA AVAILABILITY STATEMENT
Data available on request from the authors.




