The psychometric properties of the Persian version of the Multiple Sclerosis Self-Management Scale-Revised: A cross-sectional methodological study
Abstract
Backgrounds and Aims
Patients with multiple sclerosis (pwMS) need self-management (SM) skills to manage their symptoms and problems. An essential step to SM improvement is accurate SM assessment using valid and reliable instruments. The aim of this study was to evaluate the psychometric properties of the Persian version of the Multiple Sclerosis Self-Management Scale-Revised (MSSMS-R).
Methods
This cross-sectional methodological study was conducted from December 2021 to June 2022. The face, content, and construct validity of MSSMS-R were evaluated. Construct validity was evaluated through confirmatory factor analysis (CFA) and evaluating convergent and discriminant validity using the data obtained from 210 randomly selected MS patients. The reliability of the scale was also evaluated through the test–retest stability and the internal consistency evaluation methods.
Results
The face validity was confirmed and the content validity ratio and index values of all items were more than 0.62 and 0.79, respectively. CFA revealed the acceptable construct validity of the scale after omitting items 21 and 22. In convergent and discriminant validity evaluation, the total score of MSSMS-R had significant positive correlation with the total mean scores of the Multiple Sclerosis Self-Efficacy Scale (r = 0.36; p < 0.001) and the physical health composite (r = 0.31; p < 0.001) and the mental health composite (r = 0.39; p < 0.001) dimensions of the 54-item Multiple Sclerosis Quality of Life scale and significant inverse correlation with the total mean score of the Beck Depression Inventory (r = –0.28; p < 0.001). The Cronbach's alpha values of the scale and its subscales were 0.86 and 0.65–0.90 and their test–retest intraclass correlation coefficients were 0.97 and 0.95–0.99, respectively.
Conclusion
The Persian MSSMS-R is a valid and reliable scale and can be used in future studies for SM assessment among pwMS.
Key points
The aim of this study was to evaluate the psychometric properties of the Persian version of the Multiple Sclerosis Self-Management Scale-Revised (MSSMS-R). In Iran, there is no standard and reliable tool to check the self-management (SM) of patients with multiple sclerosis (MS). Therefore, due to the increase of MS disease in the country and the lack of a reliable tool to check the SM of these patients, we decided to check the psychometric properties of the Persian version of the MSSMS-R. We hope that we have taken a positive step in this direction
1 INTRODUCTION
Multiple sclerosis (MS) is a prevalent inflammatory demyelinating disease of the central nervous system.1 It affects more than 2.5 million people worldwide2 and its prevalence has increased in the last five decades.3 The number of MS-afflicted patients increased by 10% from 1990 to 2016 and reached 2,221,188.4 Recent studies reported that the global prevalence of MS in 2020 was 4395 per 100,000 people.5 The highest prevalence of MS is in North America, West Europe, and Australia, while its lowest prevalence is in Sub-Saharan Africa, countries in Central Africa, and Oceania.4 With a prevalence of five cases per 100,000 people, Iran is a low-risk country respecting MS prevalence.3 Iran is a Muslim country in Western Asia with a population of more than 85 million people. People from different ethnic groups live in Iran and the dominant language in the country is Persian.6 The total number of patients with MS (pwMS) in Iran in 2017 was 62,000 and the age-standardized prevalence of MS was 69.5 per 100,000 people.5 MS prevalence among women is three times more than among men. Although its onset age is usually 20–40 years, it may happen at any age.3
MS is associated with different physical, mental, and social symptoms and problems.7, 8 Currently, there is no effective treatment for MS. Given the early onset age and chronicity of the disease, self-management (SM) is one of the most important strategies for MS management,9 symptom alleviation,10 and patient empowerment.7 The concept of SM is broadly defined as learning and performing the necessary skills for active and emotionally satisfactory life during the course of a chronic disease.9, 11, 12 SM in a chronic disease is an approach through which patients can be empowered to manage their health status.7 SM strategies such as better disease understanding, enhancement of disease-related knowledge, adherence to dietary regimen and healthy eating, and improvement of disease management skills can improve patient health and reduce disease consequences.13 The pwMS can play significant role in the management of their disease far from expectations.2 Nonetheless, studies show that these patients have limited SM-related knowledge.9, 13 With the peak of the COVID-19 pandemic in Wuhan, China, since early December 2019, patients with autoimmune diseases, including MS, have been particularly vulnerable to severe outcomes from viral pandemics. These patients had on average more than double the rate of both severe outcomes (hospitalization and use of ventilator) and mortality. The inability of these patients to SM during the COVID-19 pandemic worsened the condition and increased the need for hospitalization and, as a result, the exacerbation of the infection14 and hence, SM skills improvement is greatly important for them.15
An essential step to SM improvement is its accurate assessment using valid and reliable instruments. However, most previous studies into SM among pwMS employed self-efficacy and quality of life assessment instruments for SM assessment.15 Examples of these instruments are the Multiple Sclerosis Self-Efficacy Scale (MSSS) and the Multiple Sclerosis Quality of Life-54 (MSQOL-54) scale. The 4-dimension MSSS measures patients' ability to manage their conditions and overcome their challenges16 and the 12-dimension MSQOL-54 measures patients' physical and mental health.17 These instruments are not SM-specific and do not cover all aspects of SM. General SM assessment instruments also cannot specifically assess SM among pwMS. Therefore, comprehensive MS-specific instruments are needed for careful SM assessment among pwMS. Bishop and Frain developed the Multiple Sclerosis Self-Management Scale for SM assessment in 2007 and revised it in 2011.9 The Multiple Sclerosis Self-Management Scale-Revised (MSSMS-R) includes items on both general SM among patients with chronic diseases and specific SM among pwMS.12
Instruments developed in a specific context may not directly be suitable for other contexts. Rather, they should be translated and culturally adapted to the intended context. Recently, Saadat et al. translated MSSMS-R into Persian and reported its acceptable psychometric properties.18 Another study in Iran also reported that this scale had acceptable reliability19, while a study showed that this scale had no acceptable face validity.15
Given the paucity of information about the validity and reliability of the Persian MSSMS-R and the contradictory results of previous studies, further studies are necessary to provide firmer evidence in this area. The present study was conducted to evaluate the psychometric properties of the Persian MSSMS-R.
2 METHODS
2.1 Design
This cross-sectional methodological study was conducted from December 2021 to June 2022 to evaluate the face, content, and construct validity (confirmatory factor analysis [CFA], convergent, and discriminant validity) as well as the reliability of the Persian MSSMS-R.
2.2 Sample size
Sample size was determined based on the rule of thumb which states that at least five participants per item are necessary for factor analysis.20 Kline also states that samples larger than 200 participants are appropriate for most factor analysis models.21 Accordingly, 210 pwMS were selected through simple random sampling.
2.3 Participants
Participants were 210 pwMS who were randomly selected from the special disease clinic of Tabriz University of Medical Sciences, Tabriz, Iran, and the neurology ward of Shahid Beheshti Hospital, Kashan, Iran. These two cities were selected due to our easy access to eligible patients. Eligibility criteria were consent for participation, definite diagnosis of MS, age of 18–60 years, and ability to communicate in Persian. Participants were provided with information about the study, their verbal and written consents for participation were secured, and the Expanded Disability Status Scale (EDSS) was completed for them based on their medical records. Participants were asked to complete MSSMS-R, MSQOL-54, MSSS, and Beck Depression Inventory (BDI), and a demographic questionnaire with items on age, gender, educational level, marital status, family support, health insurance support, place of residence, and occupation.
2.4 Instruments
2.4.1 Multiple Sclerosis Self-Management Scale-Revised
MSSMS-R has 24 items in five subscales, namely six items on healthcare provider relationship/communication (HPRC) (items 9, 12, 14, 16, 18, and 20), seven items on treatment adherence/barriers (TA/B) (items 11, 15, 17, 21, 22, 23, and 24), three items on social/family support (S/FS) (items 6, 10, and 13), four items on MS knowledge and information (MSKI) (items 1–4), and four items on health maintenance behavior (HMB) (items 5, 7, 8, and 19). The 24 items of this scale are scored on a 5-point Likert scale as follows: 1: “Completely disagree”; 2: “Disagree”; 3: “Neither agree, nor disagree”; 4: “Agree”; and 5: “Completely agree”. Items 21, 23, and 24 are reversely scored and the possible total score of the scale is 24–120, with higher scores showing greater SM.9 Exploratory factor analysis revealed that these five factors explained 57.7% of the total variance. Moreover, the total score of this scale had significant positive correlation with the Delighted-Terrible Scale (quality of life) as well as the function and the control subscales of MSSS and significant inverse correlation with the physical and the psychological impact subscales of the Multiple Sclerosis Impact Scale. These findings confirmed the acceptable construct, convergent, and discriminant validity of the scale. Moreover, the Cronbach's alpha of the scale and its subscales were 0.85 and 0.59–0.85, respectively.9, 15 A recent study into the psychometric properties of the Persian MSSMS-R reported the acceptable face and content validity and reliability of the scale with Cronbach's alpha of 0.85 for the whole instrument and 0.70–0.89 for its subscales and test–retest intraclass correlation coefficient (ICC) of 0.77.18
2.4.2 Multiple Sclerosis Self-Efficacy Scale
MSSS is a valid and reliable scale developed by Rigby et al. in England to measure self-efficacy among patients with MS. It has 104 items in the four main subscales of independence and activity (five items), concerns and interests (four items), personal control (three items), and social confidence (two items). Items are scored on a 6-point scale from 1 (Completely disagree) to 6 (Completely agree) and the possible total score of the scale is 14–84, with higher scores showing greater self-efficacy. Rigby et al. confirmed the acceptable construct, convergent, and discriminant validity of this scale as well as its acceptable reliability with a Cronbach's alpha of 0.81 and a test–retest ICC of 0.81.22 Recently, Reshvanloo et al. translated MSSS into Persian and reported its acceptable psychometric properties (α = 0.90). As a result of psychometrics, the social confidence factor was removed, and the scale was modified to 11 items. The possible total score of the scale is 11–66.23 Another study also showed that the Persian version of this scale had acceptable validity and reliability (α = 0.92).24
2.4.3 MSQOL-54 scale
The MSQOL-54 scale assesses the quality of life of pwMS. It has 54 items and 12 subscales along with two summary scores, and two additional single-item measures. The subscales are: physical function, health perceptions, energy, role limitations- physical, sexual function, role limitations-emotional, bodily pain, social function, emotional well-being, cognitive function, health distress, and overall quality of life. The summary scores include the physical health composite (PHC) and mental health composite (MHC), which are measured by adding several subscales accordingly. The single-item measures are satisfaction with sexual function and change in health. The possible score of each subscale is 0–100. The total score of PHC is calculated through summing the weighted scores of eight subscales, while the total score of MHC is calculated through summing the weighted scores of five subscales. Previous studies confirmed the validity and reliability of this scale.25, 26
2.4.4 Beck Depression Inventory
BDI is an instrument for the measurement of the symptoms and the feedback of patients with depression. It was first developed in 1961, revised in 1971, and published in 1978. It has 21 items and its possible total score is 0–63.27 This inventory has acceptable validity and reliability.28
2.5 Face validity evaluation
Qualitative and quantitative approaches were used for face validity evaluation. For qualitative face validity evaluation, 10 pwMS and 10 experts were asked to comment on the wording, difficulty, relevancy, and ambiguity of MSSMS-R items. The participants were asked to provide items or SM components that should be added to the scale, as well as suggestions for removing scale items. Patients were involved in face validity evaluation because they were directly affected by MS-related problems and challenges. Moreover, for quantitative face validity evaluation, the scale was distributed among a panel of experts and they were asked to rate item importance on a 5-point Likert scale, ranging from 1 (unimportant) to 5 (quite important). Then, the number of people who selected the scores of 4 or 5 for each item, the total scores of each item, and the average scores of each item were determined. Finally, quantitative face validity was calculated using the formula of the item effect (Impact Score = frequency × importance). In this study, an impact score of 1.5 or greater was considered acceptable.
2.6 Content validity evaluation
Content validity was evaluated through quantitative and qualitative methods. In qualitative content validity evaluation, 10 experts were invited to comment on the content, structure, grammar, wording, importance, and allocation of the items. Quantitative content validity evaluation was also performed through calculating the content validity ratio (CVR) and content validity index (CVI). Accordingly, 10 experts (namely two nurses from neurology ward, two neurology specialists, and six nursing experts) were asked to rate item essentiality as either “Essential,” “Useful but not essential,” or “Not essential.” Their rating scores were used to calculate item CVR. Based on Lawshe's table, the minimum acceptable CVR value for 10 experts is 0.62.29 Moreover, the same 10 experts were asked to rate the relevance, simplicity, and clarity of the items on a 4-point scale and CVI values of the items were calculated based on their rating scores. According to Waltz and Basel, the minimum acceptable CVI value for 10 experts is 0.79.30
2.7 Construct validity evaluation
Construct validity was evaluated through performing CFA and evaluating convergent and discriminant validity.
2.7.1 Confirmatory factor analysis
CFA was performed using the maximum likelihood method and model fit indices, namely discrepancy divided by degree of freedom (CMIN/DF), root mean square error of approximation (RMSEA), comparative fit index (CFI), Akaike information criterion (AIC), Incremental fit index (IFI), Tucker-Lewis index (TLI), and Adjusted goodness of fit index (AGFI). AGFI and CFI values greater than 0.9, RMSEA less than 0.9, and CMIN/DF between 1 and 5 confirm the good fitting of the CFA model.
2.7.2 Convergent and discriminant validity evaluation
Convergent and discriminant validity were evaluated using MSSS, MSQOL-54 scale, and BDI. Participants personally completed these instruments in a quiet and calm environment.
2.8 Reliability evaluation
The reliability of the MSSMS-R was evaluated using the test–retest stability and the internal consistency evaluation methods. In the test–retest stability evaluation method, 30 participants two times completed MSSMS-R with a 3-week interval and then, test–retest ICC was calculated. Internal consistency was also evaluated through calculating the Cronbach's alpha of the whole scale and its subscales using the data obtained from all participants.
2.9 Statistical analysis
The SPSS (v.22.0) and the Amos (v.23.0) software were used for data analysis. Statistical methods used for data analysis in the present study were CFA and model fit indexes, Pearson's correlation analysis, ICC, and Cronbach's alpha calculation.
2.10 Ethical considerations
The Ethics Committee of Tehran University of Medical Sciences, Tehran, Iran, approved this study (code: IR.TUMS.FNM.REC.1399.166). Participants were informed about the study aim and methods, were ensured participation voluntariness, and informed consent was obtained from all of them. Study authors adhered to the ethical principles of conducting and publishing studies on human subjects.
3 RESULTS
3.1 Descriptive statistics
In this study, all 210 participants completed the study. Their age mean was 37.06 ± 12.4 years and most of them were female (71.4%) and married (70%) and had an EDSS score of 1–4 (82.85%). 83% of them were supported by family, 70% of them were supported by health insurance, and 38.6% of them were unemployed (Table 1). The mean (SD) of MSSMS-R, MSQOL-54 (PHC), MSQOL-54 (MHC), MSSS, and BDI total score in 210 samples were 94.48 (13.19), 59.15 (19.97), 55.6 (22.1), 45.73 (10.01), and 16.85 (11.94). Also, Table 2 shows dispersion measures of the SM scale of people with MS.
| Participants (N = 210) | ||
|---|---|---|
| Characteristic | n (%) | |
| Gender | ||
| Male | 60 | 28.6 |
| Female | 150 | 71.4 |
| Marital status | ||
| Single | 63 | 30 |
| Married | 147 | 70 |
| Educational level | ||
| Below diploma | 58 | 27.6 |
| Diploma | 61 | 29 |
| University | 91 | 43.3 |
| Place of residence | ||
| Urban areas | 193 | 91.9 |
| Rural areas | 17 | 8.1 |
| Disability by EDSS score | ||
| 1–4 | 174 | 82.85 |
| 5–8 | 36 | 17.15 |
- Abbreviation: EDSS, Expanded Disability Status Scale.
| Variables | Items | Min | Max | M | SD | Variance | Skew | Kurt |
|---|---|---|---|---|---|---|---|---|
| MSSMS-R | 24 | 42 | 117 | 94.48 | 13.19 | 174.20 | −0.66 | 0.64 |
| HPRC | 6 | 6 | 30 | 24.97 | 5.18 | 26.85 | −1.43 | 2.17 |
| TA/B | 7 | 14.00 | 35.00 | 26.58 | 4.59 | 21.09 | −0.30 | −0.39 |
| S/FS | 3 | 3.00 | 15.00 | 11.51 | 2.79 | 7.79 | −0.91 | 0.71 |
| MSKI | 4 | 6.00 | 20.00 | 16.30 | 3.11 | 9.68 | −1.009 | 0.46 |
| HMB | 4 | 4.00 | 20.00 | 15.10 | 3.42 | 11.74 | −0.91 | 0.67 |
- Abbreviations: HMB, health maintenance behavior; HPRC, healthcare provider relationship/communication; MS, multiple sclerosis; MSKI, multiple sclerosis knowledge and information; MSSMS-R, Multiple Sclerosis Self-Management Scale-Revised; S/FS, social/family support; TA/B, treatment adherence/barriers.
3.2 Validity
3.2.1 Face validity
Face validity was assessed using both quantitative and qualitative approaches according to experts' and patients' opinion. For qualitative face validity, experts and patients confirmed that the appearance of the items reflects the whole purpose of the scale. Therefore, no items were changed in qualitative face validity. Quantitative face validity was assessed by measuring the impact score for each item, and since the score of all 24 items was above 1.5, all items were considered for further steps.
3.2.2 Content validity
In qualitative content validity evaluations, the experts confirmed that the items were congruent with the aim of the scale and had appropriate wording, grammar, structure, and allocation. In quantitative content validity evaluation, the CVR values of all items were more than 0.62 and their CVI values were more than 0.79.
3.2.3 Construct validity
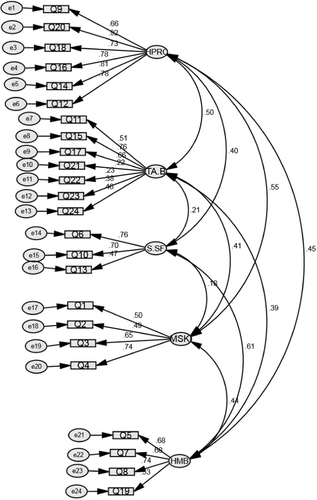
In construct validity evaluation, all 210 participants completed the study. CFA was used to evaluate the factor loading of each item with its own factor. Primary CFA showed an unfit model (χ2 = 507.15; df = 242; p < 0.01; TLI = 0.82; RMSEA = 0.072) (Table 3 and Figure 1). After model correction, omission of items 21 and 22, and determination of the correlation among the errors of measurement, all model fit indices confirmed the good fitting of the model (χ2 = 329.151; df = 198; p < 0.01; TLI = 0.90; RMSEA = 0.056; Table 3). Table 4 displays the scale items and loadings (for absolute values > 0.3) for the five factors. Also, the relationship among the factors confirmed the good fitting of the model (Table 5).
| Model | χ2 | CMIN/DF | RMSEA | CFI | IFI | AIC |
|---|---|---|---|---|---|---|
| Primary | 507.15 | 2.09 | 0.072 | 0.84 | 0.85 | 623.155 |
| Corrected | 329.151 | 1.66 | 0.056 | 0.92 | 0.92 | 439.151 |
- Abbreviations: AIC, Akaike information criterion; CFI, comparative fit index; CMIN/DF, discrepancy divided by degree of freedom; IFI, Incremental fit index; RMSEA, root mean square error of approximation.
| Item | TA/B | HPRC | MSKI | HMB | S/FS |
|---|---|---|---|---|---|
| 11. Most decisions in my life I make on my own (or with my partner). | 0.542 | ||||
| 15. I am confident I need to take my medication to be healthy. | 0.803 | ||||
| 17. Taking my medication is a routine part of my regular activities (like brushing my teeth). | 0.660 | ||||
| 23. Sometimes, I still forget to take my medication. | 0.301 | ||||
| 24. I feel like taking my medication is a trial run; I might decide to stop. | 0.390 | ||||
| 9. My medical provider is very willing to answer all of my questions. | 0.653 | ||||
| 12. I am comfortable discussing my questions with my healthcare provider. | 0.794 | ||||
| 14. I talk to my doctor about the side effects from my medications. | 0.793 | ||||
| 16. I feel like I am involved in decisions about my treatment. | 0.766 | ||||
| 18. I have confidence in the treatment approach of my medical provider. | 0.752 | ||||
| 20. My doctor and I have very good communication about my condition. | 0.905 | ||||
| 1. I feel like I understand what MS is. | 0.442 | ||||
| 2. I seek out information about my MS. | 0.628 | ||||
| 3. Since I was diagnosed with MS I have learned very much about it. | 0.591 | ||||
| 4. I have a good understanding of why I take my medications and what they are supposed to do. | 0.835 | ||||
| 5. I try to take a break when I feel myself getting tired. | 0.659 | ||||
| 7. I make sure I eat regular meals. | 0.675 | ||||
| 8. I get enough sleep. | 0.730 | ||||
| 19. I avoid getting overheated when possible. | 0.518 | ||||
| 6. I feel I have a lot of emotional support from my friends or family. | 0.774 | ||||
| 10. My immediate family is very supportive of me in handling my condition. | 0.689 | ||||
| 13. I have friends who are supportive of me in handling my condition. | 0.459 |
- Abbreviations: HMB, health maintenance behavior; HPRC, healthcare provider relationship/Communication; MS, multiple sclerosis; MSKI, multiple sclerosis knowledge and information; S/FS, social/family support; TA/B, treatment adherence/barriers.
| MSSMS-R factor | 1 | 2 | 3 | 4 | M | SD |
|---|---|---|---|---|---|---|
| 1. Healthcare provider relationship/communication | − | 24.97 | 5.18 | |||
| 2. Treatment adherence/barriers | 0.388** | 19.76 | 3.76 | |||
| 3. Social/family support | 0.396** | 0.14* | 11.51 | 2.79 | ||
| 4. MS knowledge and information | 0.434** | 0.277** | 0.16* | 16.30 | 3.11 | |
| 5. Health maintenance behavior | 0.404** | 0.266** | 0.449** | 0.312** | 15.1 | 3.42 |
- Abbreviations: MS, multiple sclerosis; MSSMS-R, Multiple Sclerosis Self-Management Scale-Revised.
- * p < 0.05
- ** p < 0.01.
To assess the construct validity of the MSSMS-R, we assessed its correlation with MSSS, MSQOL-54, and BID. Pearson's correlation was also used to examine convergent and discriminant validity. In convergent and discriminant validity evaluations, the total mean score of MSSMS-R had significant positive correlation with the total mean scores of MSSS (r = 0.36; p < 0.001) and the MSQOL-54 scale (Physical health: r = 0.31; p < 0.001 and Mental Health: r = 0.39; p < 0.001) and significant inverse correlation with the total mean score of BDI (r = –0.28; p < 0.001). These correlations are presented in Table 6.
| Scale | n | Mean (SD) | Correlation with MSSMS-R | p |
|---|---|---|---|---|
| MSSMS-R | 210 | 87.71 (12.64) | - | - |
| MSQOL-54 | ||||
| Physical Health | 147 | 59.15 (19.97) | 0.31 | p < 0.001 |
| Composite Mental Health Composite | 210 | 55.6 (22.1) | 0.39 | p < 0.001 |
| MSSS | 210 | 45.73 (10.01) | 0.36 | p < 0.001 |
| BDI | 210 | 16.85 (11.94) | −0.28 | p < 0.001 |
- Abbreviations: BDI, Beck Depression Inventory; MSQOL-54, 54-item Multiple Sclerosis Quality of Life; MSSS, Multiple Sclerosis Self-Efficacy Scale; MSSMS-R, Multiple Sclerosis Self-Management Scale-Revised.
3.3 Reliability
In reliability evaluation, the Cronbach's alpha and the test–retest ICC of the MSSMS-R were 0.86 and 0.97, respectively. Moreover, the Cronbach's alpha and the test–retest ICC values of the HPRC, TA/B, S/FS, MSKI, and HMB subscales of MSSMS-R were 0.90 and 0.99, 0.65 and 0.99, 0.65 and 0.95, 0.69 and 0.99, and 0.74 and 0.98, respectively.
4 DISCUSSION
The aim of this study was to evaluate the psychometric properties of the Persian MSSMS-R. In the present study, face validity was confirmed by the panel of experts and patients. Content validity evaluation revealed that the CVR and the CVI values of all items were more than 0.62 and 0.79, respectively. When the number of experts is 10, CVR values more than 0.62 and CVI values more than 0.78 confirm acceptable content validity.29, 31 A previous study in Iran also confirmed the acceptable face and content validity of the Persian MSSMS-R,18 while another study showed that the face validity of the scale should be re-evaluated.15
Previous studies did not evaluate the construct validity of MSSMS-R and recommended its evaluation in future studies. In the present study, the construct validity of the scale was confirmed through CFA and convergent and discriminant validity evaluations. In CFA, items 21 and 22 were omitted due to their low factor loading values. Accordingly, the 22-item MSSMS-R had acceptable construct validity. However, two studies into the psychometric properties of the original and the Persian MSSMS-R revealed that all items had acceptable factor loading values,9, 18 while in a study on the Polish version of the scale, the original factor structure of the scale was not confirmed.32 Items 21 and 22 are on treatment adherence. Regular intake of medications despite knowing their side effects may be difficult for patients and may lead to poor treatment adherence. According to Floyd and Widaman, large number of items, particularly five to eight items per factor, is usually associated with poor model fit.33 The poor fit of the first-factor analysis model in the present study and the subsequent need for omitting items 21 and 22 may be due to the fact that the number of the items of the TA/B subscale of MSSMS-R was 7 and was more than the items of the other subscales.
Study findings showed that the total mean score of MSSMS-R had significant positive correlation with the total mean scores of MSSS and MSQOL-54 scale, confirming the acceptable convergent validity of MSSMS-R. Convergent validity is a quantitative measure that shows the level of intercorrelations of the items on a scale.34 In agreement with our findings, the study into the psychometric properties of the original MSSMS-R showed that the correlations of the mean score of MSSMS-R with MSSS and DTS (quality of life) scale were significant and positive, though the strength of the correlations was less than the present study.9 In a study, there was a significant correlation between the scores of the Polish version of the MSSMS-R and the general Self-efficacy Scale (r = 0.34; p < 0.001).32 Another study reported that SM had significant correlation with self-efficacy among pwMS and noted that multiple physical and mental problems among these patients reduce their competence and confidence in their health management, their control over their functions, and their self-efficacy.2 Therefore, strategies to improve SM can improve self-efficacy and quality of life among pwMS.35
Discriminant validity evaluation revealed that the total score of MSSMS-R had significant inverse correlation with the score of BDI, which confirms the acceptable discriminant validity of the scale. Discriminant validity shows the amount of difference between the items of a factor and the items of other factors. Moreover, it denotes the poor correlation of a factor with irrelevant factors.36 In agreement with our findings, a previous study showed that depression among pwMS is associated with poor treatment adherence, sleep disorders, and daily weakness, which are the symptoms of MS.37 The discriminant validity of the original MSSMS-R was also confirmed through the significant inverse correlation of the total score of MSSMS-R with the scores of the physical and the psychological impact subscales of the Multiple Sclerosis Impact Scale.9
Our findings also showed that the Cronbach's alpha and the test–retest ICC values of MSSMS-R and all its subscales were 0.65 and more, confirming the acceptable reliability of the scale. Previous studies into the psychometric properties of MSSMS-R also confirmed its acceptable reliability with Cronbach's alpha and test–retest ICC values of more than 0.60.9, 10, 15, 18, 19, 32
5 CONCLUSION
The results of the present study showed that MSSMS-R is valid and reliable in Iranian samples. Therefore, it can comprehensively measure the SM of pwMS in different dimensions, such as relationship with health providers, adherence to treatment and its barriers, social-family support, MS knowledge and information, and health maintenance behavior, and can be very important in planning their care and treatment. Of course, further studies on patients from different age groups and different cities are recommended to produce firmer evidence regarding the psychometric properties of MSSMS-R.
6 STUDY LIMITATIONS
One of the limitations of this study was that most participants were young and had low EDSS scores and hence, study findings may not widely be generalizable to patients from other age groups and patients with severe disability. Future studies are recommended to evaluate the psychometric properties of MSSMS-R among patients with high EDSS scores. Another limitation of the study was that test–retest stability evaluation was performed using the data obtained from only thirty patients. Besides, the study was conducted only in two cities in Iran. Studies in different cities are needed to provide more reliable information about MSSMS-R. A further limitation of the study is that it did not assess the outcome of the MSSMS-R utilization and the predictors of the mean score.
AUTHOR CONTRIBUTIONS
Mahnaz Atapour: Conceptualization; data curation; formal analysis; funding acquisition; investigation; methodology; project administration; supervision; validation; visualization; writing—original draft; writing—review and editing. Farzaneh Maghaminejad: Data curation; formal analysis; methodology; validation; writing—original draft; writing—review and editing. Shahrzad Ghiyasvandian: Conceptualization; funding acquisition; investigation; methodology; project administration; supervision; validation; visualization; writing—original draft; writing—review and editing. Mitra Rahimzadeh: Formal analysis; investigation. Samaneh Hosseini: Data curation.
ACKNOWLEDGMENTS
This article sprang from a research project approved by the Research Administration of the Faculty of Nursing and Midwifery of Tehran University of Medical Sciences, Tehran, Iran. The authors would like to thank the Research Administrations of the faculty and the university as well as the participants of the study. The present study was financially supported by the Tehran University of Medical Sciences, Tehran, Iran (code: IR.TUMS.FNM.REC.1399.166).
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
TRANSPARENCY STATEMENT
The lead author Shahrzad Ghiyasvandian affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the first author, Mahnaz Atapour, upon reasonable request.




