Appropriate procedures to increase the adherence of children to blood collection: A cross-sectional study
Abstract
Background and Aim
Venipuncture for blood collection elicits fear and pain in children. We investigated factors that affect satisfaction with health checkups that included blood collection in healthy 7–8-year-old children who underwent blood collection with topical anesthesia.
Method
Two studies, one questionnaire survey, and the other structured interviews were conducted to gather insights and understand the emotions of 492 and 20 children, respectively.
Results
We found that the following six points can be applied to encourage children to assess their experience of blood collection positively: (1) prior information using a pamphlet; (2) telling the children that the volume of blood drawn will be small; (3) carefully explaining the risk and benefit of topical anesthesia; (4) conducting the blood collection process swiftly; (5) praising and thanking the children's effort and cooperation; and (6) explaining the results of the research to the children if their blood is going to be used for research.
Conclusion
The findings indicate that with appropriate measures to reduce pain and fear, children's initial negative feelings toward blood collection can be replaced by positive feelings after the procedure.
1 INTRODUCTION
Puncture elicits pain and fear in children. For example, in a survey of children visiting a public museum in Toronto, Canada, 63% of 1024 children responded that they had a fear of needles.1 However, vaccines and other treatments that involve puncture are effective for maintaining their health.
From the perspective of medical research, collecting blood from children enables to investigation of various health-related risk factors. Cells in blood collected from children with Huntington's disease and other diseases are used to establish disease-specific induced pluripotent stem cells (iPSCs) that are, in turn, used to examine pathologies and therapies for those diseases.2 In addition, Kyoto University, the first institution in the world to establish iPSCs, has launched the “My iPS Project” which seeks to develop technologies that will enable individuals to establish and preserve their own iPSCs at low cost for future treatment for those individuals.3 Although such technologies have yet to be realized, if projects like these bear fruit, they would enable the establishment and preservation of iPSCs from childhood; therefore, they may help individuals to maintain their health.
As mentioned in the Declaration of Helsinki, informed assent is important in the recruitment of children as participants in medical research.4 However, most children are not willing to approve of treatments that evoke fear. According to Flory and Emanuel,5 informed consent is more effective as a dynamic, interactive, and evolving process rather than as a one-time disclosure event. If this idea is to be expanded to informed assent, children's negative feelings toward blood collection may be replaced by positive feelings if appropriate measures are conducted to reduce pain and fear. Thus, this paper investigates factors that affect satisfaction with health checkups that include blood collection.
Pain is the most influential factor in causing negative feelings toward puncture. A guideline published by HELPinKids&Adults, an independent, cross-Canada multidisciplinary team assembled in 2008 to tackle the gap between evidence to mitigate the pain at the time of vaccination and clinical practices, recommends topical anesthetics before puncturing in children.6 However, even if topical anesthesia is an effective method for eliminating pain, it cannot eliminate needle fear or pain completely. For instance, children with intellectual disabilities are more susceptible to needle fear and experience pain more than children without intellectual disabilities, even when topical anesthesia or other forms of pain relief are applied.7 Based on such circumstances, in addition to topical anesthesia, the HELPinKids&Adults guidelines recommend distraction, parental presence, parental education about pain management before the vaccination, and education of parents and children about pain management on the day of vaccination. The guidelines also recommend that aspiration does not take place.
Thus, although various methods are employed to relieve pain, in light of informed assent, further study is necessary. In addition to the education of parents about pain management before the day of vaccination, guidelines and systematic reviews used as evidence in the guidelines8-14 focusing on what medical professionals can do on the day of puncture at medical facilities. In other words, much remains to be examined regarding the effect of providing information on punctures before parents and children visit medical facilities. Moreover, although it must be understood that children find it difficult to verbalize their own experiences, few studies have examined how children assess their experiences of puncture. In addition, as these guidelines focus only on vaccinations, the circumstances for blood collection may differ slightly. In fact, in a study of adults, some participants reported anxiety regarding blood collection, even if they did not fear needles.15
Therefore, we established two objectives to examine methods for understanding and realizing children's positive assessment toward blood collection. The first objective was to examine the effect of providing information in advance on satisfaction with experiences of blood collection using topical anesthesia based on an analysis of questionnaire surveys (Study 1). The second objective was to use interviews with children to examine how and by what processes children assess their experiences of having their blood drawn with topical anesthesia (Study 2).
2 METHODS
2.1 Examined population
This paper analyzed data from healthy 7–8-year-old children who had had their blood drawn after undergoing topical anesthesia. The Japan Environment and Children's Study (JECS) is a nationwide birth cohort study that monitors over 100,000 children from prebirth until age 13 by the Ministry of the Environment, Japan.16 The participants of JECS were recruited from 15 regions in Japan including the Koshinregion, which is constituted of Yamanashi prefecture and Nagano prefecture. The population examined in this paper comprised some JECS participants in the Yamanashi prefecture. The studies of this paper were conducted as the Yamanashi adjunct study of the JECS.
2.2 Context of blood collection of children
In addition to questionnaire-based surveys conducted at regular intervals, the JECS conducts height and weight measurements, urine tests, and computer-based development tests as school-age tests for second-year elementary school students (i.e., ages 7–8 years). Simultaneously, in the Yamanashi prefecture, “comprehensive health checkups,” which include taking blood samples from children, are conducted as the Yamanashi adjunct study of the JECS. These comprehensive health checkups also involve abdominal/thigh circumference measurement, eye exams, and dental exams for children, as well as blood collection and questionnaire surveys for the children's mothers.
School-age tests/comprehensive health checkups are conducted as follows: Before the day of tests/checkups, information including a pamphlet is sent to all participating households. The pamphlet explains tests/checkups including blood collection with illustrations. On the day of the tests/checkups, the child and their parents visit the University of Yamanashi (the test site) at individually determined time slots. The staff explain the procedures using the pamphlet and obtain informed consent from parents, and informed assent from the children for the tests/checkups. At this time, in most cases, anesthesia patches containing lidocaine are applied to the child's arms to relieve the pain of blood collection (in rare cases, anesthesia patches are not applied due to parents' objection or the child's decision). Next, while the child's parent waits in another room, the child undergoes tests other than blood collection until the topical anesthesia begins to take effect. After that, the child and their parent meet, and their blood is drawn. After receiving an explanation of some tests/checkups results, the parent and child return home. The entire process takes roughly 2 h.
At blood collection, the staff confirms the children's assent again because blood collection is not mandatory. In addition to topical anesthesia with anesthesia patches, the following devices are employed to relieve pain: Popular animated character decorations on the walls of the blood collection room, having the child's parent (typically the mother) sit with the child, an explanation of the procedure with a tablet computer (mental preparation), allowing the child to sit on their parent's lap during the procedure if they wish to do so, and tablet computer-based distractions (animation videos and games). Twenty-three gauge needles were used for blood collection. Although there are variations, the time from the child's entry into the room until blood collection is completed for the child is approximately 5–10 min (after blood is taken from the child, blood is taken from the mother in most cases). The time from insertion of the needle until the end of blood collection itself is approximately 1–2 min. The amount of collected blood is 10–13 ml.
2.3 Study1: Questionnaire surveys
2.3.1 Study design
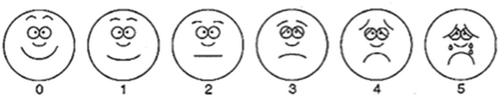
To achieve the first objective of this paper, we analyzed questionnaires submitted by participants following tests/checkups (n = 566). The questions answered by the children themselves inquired the following: the degree of pain of the venipuncture (rated 0–5 on a face scale; Figure 1), satisfaction with the tests/checkups (“How glad are you that you came for the tests today?” 1: not glad, 2: not very glad, 3: kind of glad, and 4: really glad), and information provision before blood collection (whether they read the pamphlet, whether they had heard that their blood would be drawn, and whether they had ever heard of the JECS). Survey questions answered by parents included questions about the provision of information before blood collection (whether they had explained the significance of JECS to the children, and whether they had told the children that their blood would be drawn). The checkups covered in Study 1 were conducted from April 2020 to March 2021.
2.3.2 Data analysis
Data were analyzed using IBM-Statistical Package for the Social Sciences (version 27). As shown in the result, the vast majority responded “Really glad” or “Kind of glad” for the satisfaction with tests/checkups. Therefore, we reclassified responses into “Really glad” versus all the other options and performed binomial logistic regression analysis using the degree of satisfaction as the outcome. In addition to information provision before blood collection and degree of pain, the latter of which is likely directly linked to satisfaction, in light of a finding that needle fear is more common among females than males,1, 17 we also used sex (female/male) as an explanatory variable.
2.3.3 Ethical statements
Study 1 was conducted with the approval of the Institutional Review Board of the University of Yamanashi (Approval Number: 2468) on June 16, 2021, and in accordance with the Ethical Guidelines for Medical and Biological Research Involving Human Subjects by the Japanese government (Ministry of Education, Culture, Sports, Science and Technology, Ministry of Health, Labour, and Welfare, and Ministry of Economy, Trade and Industry). In accordance with these guidelines, we provided participants with the option of opting out of surveys via the University of Yamanashi homepage.
2.4 Study 2: Interviews
2.4.1 Study design
To achieve the second objective of the study, we conducted interviews with children immediately following tests/checkups. These interviews were conducted from July to October 2021. We recruited children whose tests/checkups were completed at a time not just before lunch or in the evening, and who were expected to appropriately respond when interviewed, based on the observed communication with staff during the tests/checkups. Recruitment was terminated when the number of recruits reached 20 (8 males [Nos. 1, 3, 6, 10, 12, 13, 17, 20] and 12 females [Nos. 2, 4, 5, 7, 8, 9, 11, 14, 15, 16, 18, 19]; Nos. 14 and 15 were twins). None of these children demonstrated evident intellectual disabilities. According to the trajectory equifinality model (TEM) employed to analyze the interviews, (1) is the number of interviewees "able to explore the depth of personal experience," (4 ± 1) is the number "able to portray the diversity of experience," and (9 ± 1) is the number "able to grasp the typology of the pathways.18 Although this study aimed to "grasp the typology of pathways," the subjects of this study were children, who were less capable of verbalization than adults and may not have been able to provide sufficient narratives. Therefore, we decided to analyze the data of 20 children as (9 + 1) times 2.
During the interviews, the children were accompanied by their mothers. Including the explanation of the study, the interviews took roughly 20 min per child. Unless we asked the parents to confirm facts, the parents did not speak during any of the interviews. Questions asked in interviews included the following:
-
How did you feel when you first heard your blood would be drawn?
-
How did you feel when you got to the test site?
-
How did you feel when they explained the tests to you here?
-
How did you feel when they put the anesthesia patches on your arms?
-
How did you feel until you went into the blood collection room and they drew your blood?
-
Did you understand why your blood was being drawn?
-
How did you feel when they drew your blood?
-
How much did it hurt when they drew your blood?
-
How long did it feel like it took to draw your blood?
-
What did you think about having your blood drawn after it was over?
-
What did you think was good about the tests/checkups?
-
What did you think was bad about the tests/checkups?
For the questions about the pain of blood collection and the child's assessment of their experience of blood collection, we used the same face scale used to assess pain in the survey. To alleviate the children's tension, we conducted the interviews by showing the children a slide show with animated characters, with questions written on the slides on a laptop computer.
2.4.2 Data analysis
We created verbatim transcripts of the interviews and analyzed the transcripts using TEM,19 which is a methodological research framework to analyze, examine, and describe qualitative data concerning the diversity of trajectories of human development and life courses. It was developed based on the idea called “equifinality.” According to the idea, certain points represent common destinations even though individuals may follow various paths to reach those goals. In this approach, the researchers draw the various paths of interviewees toward common destinations setting up the following concepts: equifinality point (EFP), polarized equifinality point (P-EFP), obligatory passage point (OPP), bifurcation point (BFP), social direction (SD), and social guidance (SG). The EFP is the point at which the idea of equifinality is embodied. The P-EFP is a concept that represents the complementary set of EFP. The OPP is a point through which most interviewees and people having common experiences are thought to pass logically, institutionally, and customary. The BFP is the point at which more than two trajectories diverge. SD is a concept that influences an individual's experience negatively, whereas SG influences it positively.20 In this study, the EFP was a “positive assessment of blood collection” (response of 0, 1, or 2 to assessment of blood collection), whereas the P-EFP was a “negative assessment of blood collection” (response of 3, 4, or 5 to the assessment of blood collection). The OPP was “having blood drawn.” For the BFP, SD, and SG, we applied titles that succinctly represent the content of the children's statements. The validity of the titles was examined by the authors.
3 RESULTS
3.1 Study 1: Surveys
3.1.1 Distributions of variables
Of the children who submitted surveys (n = 566), we first excluded those who did not undergo blood collection (n = 46) and those who did not undergo topical anesthesia due to their parents' wishes (n = 12). Of the remaining 507 children, we then excluded cases with missing values (n = 15). Data for the remaining 492 children including 9 children whose records showed that blood collection was discontinued midway through despite the needle having been inserted were analyzed.
As Table 1 shows, 72% of children answered “Really glad,” 23.2% answered “Kind of glad,” 2.6% answered “Not very glad,” and 2.2% answered “Not glad”; thus, although factors such as children having completed their surveys with medical staff present must be considered, the vast majority of children responded “Really glad” or “Kind of glad” with respect to the level of satisfaction with the tests/checkups. In addition, a total of 60 children (12.3%) responded to the face scale with 3 (n = 21), 4 (n = 19), or 5 (n = 20), demonstrating that anesthesia did not remove pain completely.
| n | % | |
|---|---|---|
| Satisfaction with the tests/checkups | ||
| Not glad | 11 | 2.2 |
| Not very glad | 13 | 2.6 |
| Kind of glad | 114 | 23.2 |
| Really glad | 354 | 72 |
| Degree of pain | ||
| 0 | 246 | 50 |
| 1 | 115 | 23.4 |
| 2 | 71 | 14.4 |
| 3 | 21 | 4.3 |
| 4 | 19 | 3.9 |
| 5 | 20 | 4.1 |
| Sex | ||
| Male | 237 | 48.2 |
| Female | 255 | 51.8 |
| Whether children read the pamphlet | ||
| Yes | 175 | 35.6 |
| No | 317 | 64.4 |
| Whether children had heard that their blood would be drawn | ||
| Yes | 384 | 78 |
| No | 108 | 22 |
| Whether children had ever heard of JECS | ||
| Yes | 355 | 72.2 |
| No | 137 | 27.8 |
| Whether parents had told children that their blood would be drawn | ||
| Yes | 334 | 67.9 |
| No | 158 | 32.1 |
| Whether parents had explained the significance of JECS | ||
| Yes | 154 | 31.3 |
| No | 338 | 68.7 |
- Abbreviation: JECS, Japan Environment and Children's Study.
3.1.2 Factors in satisfaction
As Table 1 shows, the vast majority responded “Really glad” or “Kind of glad.” Therefore, we reclassified responses into “Really glad” versus all the other options and performed binomial logistic regression analysis.
As Table 2 shows, the variables associated with satisfaction were having read the pamphlet (adjusted odds ratio [OR]: 1.73, 95% confidence interval [CI]: 1.05–2.85), pain (adjusted OR: 0.58, 95% CI: 0.50–0.68), and sex (female; adjusted OR: 1.65, 95% CI: 1.07–2.54). Thus, our results showed the following: satisfaction tended to decrease as the pain increased, satisfaction tended to be higher among girls than boys, and satisfaction tended to be higher among children who had read the pamphlet.
| Crude OR (95%CI) | Adjusted OR (95%CI) | |
|---|---|---|
| Whether the children read the pamphlet | ||
| No | 1 | 1 |
| Yes | 1.83 (1.19–2.83) | 1.73 (1.05–2.85) |
| Whether the children had heard that their blood would be drawn | ||
| No | 1 | 1 |
| Yes | 1.54 (0.98–2.43) | 1.30 (0.67–2.51) |
| Whether the children had ever heard of JECS | ||
| No | 1 | 1 |
| Yes | 1.52 (0.99–2.32) | 1.17 (0.71–1.94) |
| Whether the parents had told the children that their blood would be drawn | ||
| No | 1 | 1 |
| Yes | 1.24 (0.82–1.88) | 1.07 (0.5–1.64) |
| Whether the parents had explained the significance of JECS to the children | ||
| No | 1 | 1 |
| Yes | 1.42 (0.91–2.12) | 1.07 (0.64–1.8) |
| Degree of pain | 0.59 (0.51–0.68) | 0.58 (0.50–0.68) |
| Sex | ||
| Male | 1 | 1 |
| Female | 1.59 (1.07–2.37) | 1.65 (1.07–2.54) |
- Abbreviations: CI, confidence interval; JECS, Japan Environment and Children's Study; OR, odds ratio.
3.1.3 Ethical statements
Study 2 was conducted with the approval of the Institutional Review Board of the University of Yamanashi (Approval Number: 2467) on June 16, 2021, and in accordance with the Ethical Guidelines for Medical and Biological Research Involving Human Subjects by the Japanese government (Ministry of Education, Culture, Sports, Science and Technology, Ministry of Health, Labour, and Welfare, and Ministry of Economy, Trade and Industry). In accordance with these guidelines, we explained the nature of the study using printed documents to the mothers and children, who then provided consent/assent through electronic devices and verbally, respectively, at the time of the interviews.
3.2 Study 2: Interview
Figure 2 shows a model of children's feelings from the time they heard their blood would be drawn until blood collection was completed. The model enables tracking of changes in individual children's feelings.
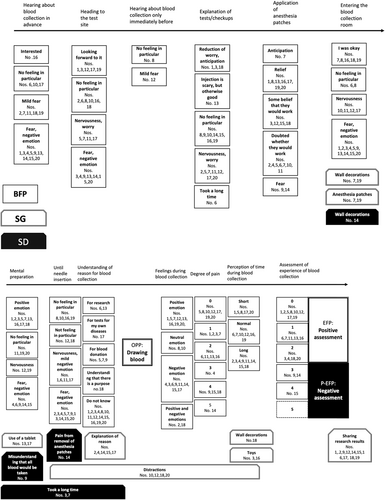
Eighteen children learned about their upcoming blood collection from their parents a day in advance, whereas two children were told only immediately before their blood was drawn. While a small number of children responded that they were “interested” in blood collection or had “no particular feeling” about it, most children were afraid of it. According to the interviews, being told about blood collection only immediately before it took place, did not necessarily ultimately lead to a negative assessment of the experience.
The children's feelings as they headed to the tests/checkups site were generally consistent with their feelings when they first heard their blood would be drawn. Some children responded that they were “looking forward to it” even though they feared blood collection. One reason given for looking forward to tests/checkups was the computer-based development test.
When the children arrived at the site, the tests/checkups were explained to them. Many children talked about feeling worried and nervous at that point, but three children described a “reduction of worry and anticipation.” All three of these children described feeling “fear” when they first heard their blood would be drawn.
After the tests and checkups were explained to the children, anesthesia patches were applied to both arms with the explanation that it would prevent the venipuncture from hurting. Although the anesthesia patches seemed to give most children some sense of relief, two children said the patches evoked “fear.”
Next, after all, other tests/checkups, the children entered the blood collection room. Many children spoke of “nervousness” or “fear and negative emotion” at that time. Children Nos. 10 and 17, who reported “no feeling in particular” when they were told their blood would be drawn, said they felt “nervous.” Moreover, child (No. 19) said, “Because Sumikko (short for Sumikkogurashi, a popular Japanese character, detailed information is available on its official web site21) was there, I would be okay”; the wall decorations functioned as SG. However, as illustrated by another child (No. 14) who said, “There were lots of characters on the walls, so I figured they were going to do something scary”; thus, the wall decorations also acted as SD. As indicated by the statement, “I got anesthesia, so I thought it wouldn't hurt much” (No. 16), the anesthesia patches acted as SG at this point and provided a sense of relief to some children.
After entering the blood collection room, the children underwent mental preparation through an explanation of the procedure using a tablet computer. Although this gave some children relief, it also evoked “fear and negative emotion.” The mere use of a tablet computer, which seemed to amuse some children (Nos. 13, 17), acted as SG. However, the mental preparation also gave rise to misunderstanding, as illustrated by the quote: “I thought they would take all my blood” (No. 9); in this case and others, the tablet computer-based mental preparation acted as SD and exacerbated children's fear.
After mental preparation, the child's blood was drawn. In regard to the feelings before the needle was inserted into the arm, although six children said they felt “nothing in particular,” the other 14 children said they felt nervous and scared. Child No. 14 stated that it hurt when the anesthesia patches were removed from her arm, an action which thus functioned as SD. Although the adults did not emphasize the removal of the patches, child No. 14 emphasized this action in the interview, recalling it as an unpleasant experience.
When we asked in interviews whether the children understood why their blood was drawn, many children responded, “I don't know.” In contrast, some children gave unique answers such as, “For blood donation” and “I get that there's a purpose,” whereas others correctly understood, “For research.” One child had the understanding, “To test for my own diseases;” since we had disclosed that we could share blood composition analysis results with the study participants, in addition to using the results for research, this understanding was not incorrect. When we asked the children who responded that they did not understand the purpose of blood collection whether they wanted us to explain why we drew their blood, five children responded that they did (all other children responded, “either way is fine”); therefore, we classified explanation of the reason for blood collection as SG (or, more accurately, as a potential SG).
With regard to the process from mental preparation until before needle insertion, one child (No. 3) said, “I got scared when all they told about was the puncture,” whereas another (No. 7) said, “I just wanted them to hurry up and give me the puncture and get it over with already. Thinking about too much made it seem painful. I wish they would've done it quickly.” These statements demonstrated that attempting to explain blood collection carefully can cause children to perceive the process as “taking a long time,” which causes the explanation to act as an SD.
Feelings during blood collection varied and are broadly classified into the following categories: “positive emotion” such as, “It didn't feel like they stuck anything in me” (No. 19); “neutral emotion” such as, “I didn't think anything either way” (No. 8); “negative emotion” such as, “I thought I was going to die” (No. 9) and “I had never felt anything that painful” (No. 15); and “positive and negative emotions” such as, “It hurt, but the game was fun” (No. 18). The statement by No.18 referred to distraction using a tablet computer. Therefore, distraction was classified as SG.
Of the assessments of the experience of blood collection, 17 were positive (EFP), whereas three (Nos. 9, 14, and 15) were negative (P-EFP). All three children who assessed the experience negatively spoke of “negative emotion” during blood collection and felt intense pain. Furthermore, these three children felt scared from the time they were told their blood would be drawn, whereas children Nos. 9 and 14 said they also felt scared when the anesthesia patches were applied. The remaining children, who said they initially felt “fear and negative emotion” or “mild fear” at first, ultimately assessed their experiences of blood collection positively even if they felt “negative emotion” during blood collection. These children generally felt only a low degree of pain.
Child No. 18, who enjoyed the blood collection experience despite the pain, said, “I had fun spotting the differences after they finished taking my blood,” suggesting that the wall decorations acted as SG. Her statement referred to two similar pictures on the wall. For children nos. 3 and 16, the puzzle toy given to the children appeared to act as SG apart from the honorarium paid to their guardians. In addition, 10 children responded that they wanted to know the results of the study for which their blood would be used, suggesting that sharing research results could positively affect the experience of blood collection; therefore, sharing research results was classified as SG (or, more accurately, as a potential SG).
4 DISCUSSION
As the questionnaire surveys suggested, satisfaction appeared to be higher among participants who read the blood collection pamphlet in advance. Related to this possibility is the statement in interviews by five children that they wanted to know why their blood was drawn. In regard to informed assent, which we touched upon in the introduction, in the event of a procedure such as blood collection that causes pain, even if a certain level of explanation (informed) is provided and the child formally agrees (assent) to the procedure, as evidenced by the participants' statements about “fear and negative emotion” and “mild fear” in interviews, obtaining active agreement in advance may not be possible. However, even if that is the case, the interview showed that a negative impression of blood collection before it takes place can be changed into a positive assessment after the fact. Moreover, our studies suggest that providing information in appropriate ways in advance may positively influence a child's satisfaction with the blood collection process.
With regard to the relationship between satisfaction and sex, females tended to demonstrate higher satisfaction in the survey. This finding is difficult to interpret when compared with previous studies which found that needle fear is more prominent in females.1, 17 One possibility is that satisfaction here was not limited to the experience of blood collection but included other tests such as the development test. In contrast, all three of the children who assessed their experience of blood collection negatively in interviews were female and felt great fear, since they first heard their blood would be drawn.
The questionnaire surveys and interviews both demonstrated that satisfaction with blood collection is greatly affected by the degree of pain experienced. However, most children answered that they felt almost no pain. Anesthesia patches are not low price (about 340 yen [about $2.43] per sheet), yet can be easily purchased and are highly effective. Thus, it is important to carefully explain not only the risks of topical anesthesia but also the benefits. Meanwhile, a few children felt severe pain even though they applied anesthesia patches. The interviews showed pain is associated with fear. Although wall decorations and other distractions can alleviate fear to some degree, polite encouragement from staff may conversely stoke fear by making children think about the venipuncture more. It is expected that effective distraction would vary depending on the characteristics of each individual child. It may not be appropriate to place too many tools of distraction, as there was a case where wall decorations in only the blood collection room caused fear in the child, contrary to our intentions. Therefore, it may be ideal to collect information on children's characteristics and preferences in advance and provide individualized inputs, such as placing tools that are likely to be of interest to the child.
One circumstance unique to blood collection, as child No. 9 described, is that misunderstandings about blood collection can arise and may increase the fear of blood collection. In addition, unlike vaccinations, collecting the necessary volume of blood takes time, during which the needle remains inserted. If blood collection does not proceed smoothly for some reason, such as in narrow vessels, more time is required. Even if more time is not required, intense pain and fear may subjectively make the procedure feel longer. For the three children who assessed their blood collection experience negatively, collecting the necessary volume of blood took a great deal of time. Thus, for these children, both absolute and subjective time were long, with child No. 9 saying, “it took about an hour.” In addition, having discontinued blood collection regardless of inserting the needle into the arm means that blood collection took a long time.
The above-mentioned observations suggest that the following six points can be applied in blood collection for children to encourage them to assess their experiences of blood collection positively, even if only after the fact. First, provide information in advance with a pamphlet containing illustrations to explain to children why their blood is going to be drawn. Second, tell children in advance that the volume of blood drawn will be small and will not affect their health. Third, carefully explain the risks and benefits of topical anesthesia to guardians. Fourth, conduct the blood collection process (including the advance explanation) swiftly and succinctly while observing the child's demeanor. Fifth, no measures to reduce pain and anguish can completely eliminate cases in which children feel intense fear and pain, or blood collection takes a long time; therefore, as soon as blood collection procedures are concluded, the adults around the child should praise and thank the child for their effort and cooperation. Sixth, if the blood drawn is to be used for research, explain the results of the research to the children in a manner they can understand.
There are some limitations to this study. First, the capability of 7–8-year-old children to verbalize their feelings needs to be considered. Second, the questionnaire measured satisfaction, not only with blood collection but with the tests/checkups overall. Third, a relatively small number of cases were used in the statistical analysis. Fourth, some children's positive evaluation toward blood collection may be because they wanted to give a positive response to the staff and/or parents. Further studies are needed to investigate children's feelings in other situations and across different age groups. However, the fact that we were able to analyze the evaluation of the blood collection experience by the children themselves is a strength of this study.
5 CONCLUSION
We investigated factors that affect satisfaction with health checkups that include blood collection in healthy 7–8-year-old children who underwent blood collection with topical anesthesia. We also examined the significance children ascribed to their own experiences of blood collection.
We demonstrated that the pain and fear associated with venipuncture can often be reduced with certain measures. In addition, we found that initial negative feelings regarding blood collection among children can be changed into positive assessments after the fact. While the vaccination of children is important, the COVID-19 pandemic has increased its significance. This study finds that reducing pain through the use of topical anesthesia, and the provision of prior information to the child leads to a positive perception of the puncture and can be applied to the practice of care.
The conclusions of this paper are solely the responsibility of the authors and do not represent the official views of the government.
AUTHOR CONTRIBUTIONS
Hideki Yui: Conceptualization; formal analysis; investigation; methodology; writing – original draft; writing – review and editing. Sanae Otawa: Investigation; project administration; writing – review and editing. Sayaka Horiuchi: Project administration; writing – review and editing. Megumi Kushima: Project administration; writing – review and editing. Ryoji Shinohara: Project administration; supervision; writing – review and editing. Reiji Kojima: Writing – review and editing. Yuka Akiyama: Writing – review and editing. Tadao Ooka: Writing – review and editing. Kunio Miyake: Writing – review and editing. Hiroshi Yokomichi: Writing – review and editing. Zentaro Yamagata: Funding acquisition; project administration; supervision; writing – review and editing.
ACKNOWLEDGMENTS
The authors would like to express gratitude to the children and their mothers for their cooperation with the present studies. The Japan Environment and Children's Study was funded by the Ministry of the Environment, Japan. This research was supported by AMED, under Grant Number, JP 20bm0904002.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ETHICS STATEMENT
The studies of this paper were conducted with the approval of the Institutional Review Boards of the University of Yamanashi in Chuo, Japan.
MEMBERS OF THE YAMANASHI ADJUNCT STUDY OF THE JAPAN ENVIRONMENT AND CHILDREN'S STUDY GROUP 2021
Zentaro Yamagata (principal investigator, e-mail: [email protected]), Ryoji Shinohara, Sanae Otawa, Anna Kobayashi, Sayaka Horiuchi, and Megumi Kushima (Center for Birth Cohort Studies, Interdisciplinary Graduate School of Medicine, University of Yamanashi, Chuo, Japan); Takeshi Inukai and Emi Sawanobori (Department of Pediatrics, School of Medicine, University of Yamanashi, Chuo, Japan); Kyoichiro Tsuchiya (Third Department of Internal Medicine, University of Yamanashi, Chuo, Japan); Hirotaka Haro and Masanori Wako (Department of Orthopedic Surgery, University of Yamanashi, Chuo, Japan); Takahiko Mitsui (Department of Urology, Interdisciplinary Graduate School of Medicine, University of Yamanashi, Chuo, Japan); Kenji Kashiwagi (Department of Ophthalmology, University of Yamanashi, Chuo, Japan); Daijyu Sakurai (Department of Otorhinolaryngology–Head and Neck Surgery, School of Medicine, University of Yamanashi, Chuo, Japan); Koichiro Ueki and Naana Baba (Department of Oral and Maxillofacial Surgery, Interdisciplinary Graduate School of Medicine, University of Yamanashi, Chuo, Japan); and Hiroshi Yokomichi, Kunio Miyake, Yuka Akiyama, Tadao Ooka, Reiji Kojima, and Hideki Yui (Department of Health Sciences, School of Medicine, University of Yamanashi, Chuo, Japan).
TRANSPARENCY STATEMENT
The lead author Hideki Yui affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
DATA AVAILABILITY STATEMENT
All authors have read and approved the final version of the manuscript. The corresponding author had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.




