What makes an action plan “100% me”? Think aloud interviews about CVD prevention tools for varying health literacy needs
Abstract
Issue Addressed
Health behaviour change can be difficult to maintain. Action plans can address this issue, however, there has been little qualitative research to understand how to optimise action plan interventions. This study explored how people engage with a specific type of action plan intervention, the “volitional help sheet,” in a cardiovascular disease (CVD) prevention context.
Methods
Twenty adults in the target age for CVD risk assessment (45 to 74 years) with varying health literacy participated in interviews and created an action plan to change their behaviour. Transcripts were analysed using framework analysis.
Results
Participants described how engagement with plans was related to how personally relevant the target behaviour and the options within the plan were. Also important was participants visualising themselves enacting the plan when deciding which option to choose. Amongst participants who already engaged in a target behaviour, some did not perceive the plan was useful; others perceived the plan as a helpful prompt or a formalisation of existing plans. For some, the barriers to behaviour change were out of the scope of an action plan, highlighting the need for alternative supports.
Conclusion
This study provides qualitative insights into unanticipated ways that people with varying health literacy use action plans, providing new guidance for future developers.
So What?
Not all action plans are created equal. Careful selection of behavioural targets and plan options and encouraging users to imagine the plan may enhance user engagement. Alternative behaviour change strategies should be available if key barriers cannot be addressed by the plan.
Abbreviations
-
- CVD
-
- cardiovascular disease
-
- HHL
-
- high health literacy
-
- LHL
-
- low health literacy
1 INTRODUCTION
A key recommendation for reducing cardiovascular risk is to engage in health behaviours such as physical activity, healthy eating and smoking cessation.1, 2 However, these behaviours are often difficult to change and maintain in the long term. This is observed even when people are well-informed about the benefits for cardiovascular health and motivated to implement these changes. An extensive body of research has shown that self-regulatory strategies such as planning are effective at helping people translate their intentions into long-term behaviour change.3-5
Behaviour change models differentiate between two types of planning. “Action plans” ask individuals to specify broad parameters for behaviour change (eg when, where) and the sequence of action (“how”). In contrast, “action plans” focus on addressing anticipated barriers to behaviour change. Behavioural theories such as the Health Action Process Approach posit that both are important for bridging the gap between intention and behaviour and maintaining that behaviour in the long-term.4, 6
A specific form of planning that has a strong evidence-base is “implementation intentions”.5, 7, 8 These are a type of plan that use an “if-then” structure. Participants choose a situation where they may be more likely to perform an unwanted behaviour (“if”) and a solution—a new behaviour that they can do instead (“then”). These are then combined, for example, “if I want to snack because I am drinking coffee, then I will listen to my favourite podcast.” Although initially created via a deliberate and conscious process, implementation intentions are thought to operate via automatic, non-conscious processes that mimic habit formation and through repeated enactment, result in reduced effort to engage in the target behaviour.9 There is a large amount of evidence, including meta-analyses and systematic reviews, demonstrating that implementation intentions are effective at encouraging healthy eating,10 increasing physical activity11 and even promoting recycling behaviours.12
However, not all implementation intentions are created equal. Quantitative research has identified several factors which influence their effectiveness, including impulsivity, self-efficacy and intention (Table 1). Research on plan quality has also shown that people with low health literacy may find standard instructions to form an implementation intention inadequate.13, 14 The “volitional help sheet” addresses many of these issues relating to plan formation.15 It involves breaking down plan formation into several steps, starting with providing users with a pre-determined list of situations and solutions. The sheets then explicitly ask participants to “link” (eg, by drawing a line) between the selected options to formulate their plan. Volitional help sheets have demonstrated effectiveness across a range of behaviours, including healthy eating, increasing physical activity and smoking cessation.15-21 This type of plan is well suited to online formats14, 22-24 which allows for easy distribution, scale-up, adaptation to different contexts and inclusion with other online resources such as decision aids or patient education.25-27 Recent research indicates they may be a particularly useful action plan format for groups with varying health literacy levels.13, 26
| Factor | Description |
|---|---|
| Cognitive/behavioural factors | |
| High intention strength6, 28 | Higher strength of intentions to pursue the desired behaviour |
| High self-efficacy6, 28, 29 | High confidence in one's ability to achieve the goal; that you can carry out the implementation intention in the future |
| Weaker habit strength6, 29 | Habit strength for the existing and undesired behaviour is weaker |
| High perceived social support29 | People who feel they have more social support |
| Plan formation factors | |
| The cue is easily recognisable or frequently occurring6 | The cues for the “if” part of the plan are relevant to the individual or the behaviour they are trying to change and are associated strongly with the behaviour. They also happen often |
| Specifying an unwanted behaviour6, 10 | The “then” option chosen is to enact an alternative behaviour, rather than to avoid a behaviour (eg, “If I feel sad then I will not eat chocolate” vs “If I feel sad then I will eat an apple”) or to simply not do the unwanted behaviour |
| Writing “if” and “then” as sentences9 | Participants should write down the “if” of the plan, in a phrase starting with the word “if.” The “then” should also be written down, in a phrase starting with “then.” Finally, these should be written down together in one sentence to link the plan components together |
| Repeating the completed plan9, 30 | Saying the complete plan aloud, writing it down again or imagining doing the plan |
| Personality/dispositional factors | |
| Low impulsivity6 | Those who are more impulsive and act spontaneously without thinking |
| Lower socially prescribed perfectionism28 | People who evaluate their behaviour based on other people's opinions |
| Lower conscientiousness6, 28, 31 | People who have this personality trait are described as hardworking, ambitious, self-disciplined, self-organised and deliberative; studies have observed ceiling effects for people with high conscientiousness |
Despite the evidence-base underpinning implementation intentions and volitional help sheets, there is little qualitative research to understand how users engage with this kind of intervention, or what the implications might be for their design and implementation. This study aimed to explore qualitatively how people with varying health literacy needs engage with an online volitional help sheet to improve cardiovascular health behaviours: reducing smoking, increasing levels of physical activity, or eating fewer unhealthy snacks.
2 METHODS
2.1 Design
This was a qualitative interview study. Ethical approval was received from the University of Sydney Human Research Ethics committee (project number 2019/774).
2.2 Participants
Participants were recruited from a trial to evaluate the effectiveness of an online cardiovascular decision aid.24 Trial participants were Australian adults aged 45 to 74 years, with no established cardiovascular disease and who were not taking cardiovascular disease prevention medications. After recruitment via an online market research panel (Qualtrics) and completion of the trial, participants were invited to express interest in the current sub-study. Of 27 who did so, 20 were invited to take part across 4 rounds of user-testing (5 participants per round), as recommended for developing digital health interventions.32 Purposive sampling ensured that participants had a range of health literacy, age, gender and cardiovascular risk. Participants were interviewed between December 2020 and March 2021. Health literacy was assessed using the Newest Vital Sign, a 6-item performance-based and widely-used health literacy instrument.33 Scores less than 4 indicate a high likelihood/possibility of limited healthy literacy (referred to as “low health literacy” in this paper). Scores of 4 or more indicate adequate health literacy (referred to as “high health literacy” herein). Cardiovascular risk was assessed using the Framingham algorithm to calculate risk of a cardiovascular event in the next 5 years and heart age, based on Australian and New Zealand guidelines that were current at the time of the study.34 During the initial trial, participants self-reported the variables used to calculate cardiovascular risk. If blood pressure or cholesterol were not known, an average using their age and sex was imputed based on an Australian cohort study.
2.3 Procedure
The interviews comprised two sections: (i) “think aloud”; (ii) semi-structured interview. “Think aloud” is a method of cognitive testing in which participants say their thoughts out loud as they interact with a stimulus (in this case, the action plan). Think-aloud studies provide insight into users' assumptions and initial impressions that may not be available through observation alone.35, 36 In the interview, participants were asked to work through the action plan, whilst speaking their thoughts aloud. They were prompted to keep talking if they were silent for more than 5 seconds. After creating the plan, participants were asked questions to further reflect on their experiences and any user feedback that they had, using a semi-structured interview schedule.
The interview schedule and think-aloud task were piloted with 2 individuals who met the eligibility criteria for the study and then refined based on their feedback. CAB, a behavioural scientist with experience of qualitative methods, interviewed all participants.
Interviews were conducted via Zoom, with recordings of audio and visual recordings of the screenshare. Audio recordings were transcribed verbatim. Notes during and after the interview were also recorded based on interviewer observations and reflections. Interviews lasted on average 38 minutes.
CB, CAB and JA used interview data to direct discussions about how to iteratively improve the action plan. These changes were then implemented before the next round/stage of interviews began, for a total of 4 rounds, as reported elsewhere.24
2.4 Interview stimulus
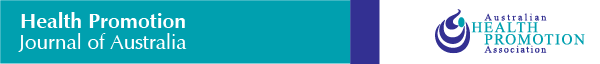
The action plans used in these interviews were part of a wider study looking at a cardiovascular disease risk calculator and decision aid.24 In the interviews, participants used the risk calculator and decision aid first and then were prompted to create an action plan. They could choose to create a plan to reduce smoking, increase physical activity, or reduce unhealthy snacking. For details of the steps involved in creating the plan, see Table 2; for screenshots of an example plan, see Figure 1. The design of the planning tool was shaped by several health literacy principles including a volitional help sheet format15 to break the planning process down into manageable steps and strategies from a Universal Precautions Approach to health literacy such as directly addressing the user where possible and using simple language and illustrative images.37
| Step | Action | Description | Reference in Figure 1 |
|---|---|---|---|
| 1 | Choose behavioural target | Asked to select a lifestyle behaviour change to focus on, out of smoking, exercise and snacking: this is the “behavioural target”. Note: in the exercise action plan, users are asked to select a form of exercise, for example, walking or swimming |
B |
| 2 | Choose 3 situations | User is presented with a list of predetermined barriers to the behavioural target. They are prompted to select three situations where they enacted the unwanted behaviour that occurred the most often in the last week | C |
| 3 | Choose key situation | User selects the situation from their list of 3 that they would be happiest to change | D |
| 4 | Choose solution | They select a different solution or new behaviour from a list of potential options | E |
| 5 | Reflecting on difficulty | Shown their plan and asked to rate how hard it would be to enact over the next month on a scale of 1 to 10 (10 being the most difficult). If they rate the plan a 7 or higher, they are asked to choose an easier solution and again asked to rate this out of 10 Note: this was changed after P8 to asking the user to rate how likely they would be to enact the plan in the next month out of 10 (10 being not at all likely) |
F and G |
| 6 | Final action plan | User shown their final action plan, prompted to say it aloud and asked if they'd like to print/screenshot/be emailed their plan | F and H |
2.5 Analysis
Audio recordings were transcribed verbatim and analysed using thematic Framework Analysis38, 39 to explore how participants engaged with the action plan. CAB familiarised herself with the transcripts before applying initial coding to each transcript. CAB and JA discussed these codes and developed preliminary themes by grouping codes into categories and sub-categories. Themes were refined through iteratively discussing the themes, applying them to the data and discussing with a third reviewer (CB). Once themes were finalised, data were then charted into a spreadsheet in which each row represented a participant and each column a theme or sub-theme. Interpretation of the themes was refined through discussion with all authors. To help future action plan developers integrate this research into their development process, theme names were reframed as practical questions. The content described in each theme explores why that particular question is relevant and how it relates to user engagement with the action plan. The sample size of 20 had sufficiently rich data to answer the research question.40
3 RESULTS
We interviewed 12 female and 8 male participants aged 46–74 years (Table 3; Appendix A). Eleven out of 19 participants who created an action plan had inadequate health literacy. Thirteen chose snacking as their behavioural target, 5 chose exercise and 1 smoking. We developed 5 themes and framed these as questions to guide action plan tailoring and design. Each theme then explores why that particular question is relevant when developing an action plan.
| Characteristic | N (%) |
|---|---|
| Gender | |
| Female | 12 (60) |
| Male | 8 (40) |
| Age (years) | |
| 40–49 | 1 (5) |
| 50–59 | 9 (45) |
| 60–69 | 6 (30) |
| 70+ | 4 (20) |
| CVD riska | |
| Low CVD risk | 19 (95) |
| Medium CVD risk | 1 (5) |
| Health literacyb | |
| Low health literacy | 11 (55) |
| High health literacy | 9 (45) |
- Note: One participant (12) did not reach the stage of the interview for creating an action plan as their internet cut out.
- a CVD risk category refers to absolute risk of having a CVD event (eg, heart attack) in the next 5 years, where “low” corresponds to <10% risk and “medium” corresponds to 10% to 15% risk. No participants were in the high risk (>15%) category.
- b Health literacy refers to NVS scores for those with limited/possibility of limited (low) and adequate (high) health literacy.
3.1 Is the target of the action plan relevant?
The following participant also felt the concept of creating their own plan was engaging because it aligned with other beliefs about personal responsibility:I'm not a physical activity sort of person, but maybe I would, but mine overall is definitely the improve, reduce unhealthy snacking (P10, 57, M, LHL[low health literacy])
For others, the behavioural targets in the action plan were not perceived as meaningful personal goals (“this doesn't do anything for me to be honest…yeah, I don't see a huge amount of value in this.”; P5, 66, M, LHL). These participants were dismissive and did not think the plan would be useful, often because they had already made lifestyle changes related to the behavioural targets. Some participants responded defensively if they felt they were being asked to change behaviours they didn't feel could be further improved.I think we should try and give less, how do I say, less pressure on the health system by encouraging you know, people to try and reduce your own risk yourself first before … you just jump onto the health system (P2, 51, F, LHL)
Well, my diet's really good. I can't change my diet any different and my physical activity can be only completed when they get this leg working (P4, 65, F, LHL)
it sort of sets it in concrete and you can look at it and think yeah, I really need to do more exercise and I need to look after myself better (P19, 66, F, HHL[high health literacy])
3.2 Would the action plan work in real life?
For some participants, many situation and solution options were relevant (“I had of that list I could have put in…12 out of that page”; P6, 56, M, LHL). Those who found relevant options quickly expressed how strongly this resonated with them (“all those three that are there are 100% me”; P6, 56, M, LHL). One participant felt that “probably 90% of people would go for [that situation]”; (P10, 57, M, LHL). Participants who identified options that were relevant, but unexpected, described how the plan gave them a new perspective on their behaviour change strategies: “music just makes me feel so much better…I hadn't considered it in terms of having a snack” (P17, 54, F, HHL).
However, there were some participants who did not find any options that seemed relevant (“I don't know what I can really put in there”; P6, 56, M, LHL).
Many participants prioritised situations and solutions by imagining how they fit into their life. For example, by thinking carefully about moments they didn't feel like exercising or ate snacks. This also helped participants feel that the chosen solution would be realistic and achievable (“I've always got music nearby. So it's an easy thing to do…I've always got music on, or handy”; P17, 54, F, HHL). Doing so also helped some participants anticipate what they needed to prepare in advance, such as buying fruit to be readily available:Yeah reasons not to swim. No, no …it's not ‘[lack of] time’, no. No… I can't see all that it's ‘boring’….Yeah, [when] I'm in pain, that could be a good one (P4, 65, F, LHL)
This process prompted some participants to switch to a different option that would be more appropriate or feasible. For example, this participant initially created the plan: “if I don't want to exercise because I am too busy, then I'll tell myself that exercising will make me happier and healthier.” After imagining enacting this, they changed it to something more realistic:I want to make sure the next time I go out for grocery shopping I should buy more fruits and make sure I eat them… (P2, 51, F, LHL)
maybe going out [for a walk] with someone who will always be like… okay, come on we have to go now… I guess that would probably be obviously the better option (P7, 46, F, LHL)
3.3 Does the action plan motivate an existing habit?
If participants were already habitually engaging with the action plan they created, this was not necessarily perceived as a negative. Perceiving a consistency between existing plans and the action plan, gave participants more confidence in their behaviour change efforts:sometimes [I'm in] so much pain it's awful, but…my biggest problem is I feel lazy…[so my action plan is] if I'm tempted not to exercise cause I feel lazy then I will tell myself that exercising will make me a healthier happier person, which I do (P8, 61, F, LHL)
Similarly, a participant mentioned that this action plan was reminiscent of a plan that their dietician recommended to them. This added credibility to both the plan and their dietician and increased their confidence in making behavioural change for the better.I like multiple choice in that you can see if the choice you make, there might be a better one… when I can see other choices, and other excuses, or other multiple choice areas…it makes me feel good that I'm choosing the right one (P8, 61, F, LHL)
that's what my dietician recommended to me…the way that you've set the survey up regarding this is very similar (P6, 56, M, LHL)
3.4 Is the plan likely to address the user's key barriers?
For these participants the action plan was perceived as less useful or relevant; they seemed less excited about the plan and voiced reluctance about using it to make changes in their life. Some participants expressed that their main barrier to changing their behaviour was lack of motivation. These participants already had ideas about how to change their behaviour (“it's almost told me what I know”; P3, 59, F, LHL) but did not feel that a plan would be address low motivation:there's no likely scenario [in which I would do this action plan] at this point without seeing a doctor I think (P10, 57, M, LHL)
Sometimes the prompt “how hard will it be to enact this plan in the next week” elicited these attitudes. Participants at times responded by expressing that the plan was feasible, but did not reflect their key reason for not changing behaviour:I don't think it's…completely motivating, because it's something you already know, so it's still like a mindset (P14, 51, F, HHL)
A further barrier to change which the plan did not address related to social or family roles. For example, a participant described how family commitments seemed to be a key barrier to exercising (“No I can't go to gym classes it clashes with [my granddaughter's] singing [class]”; P19, 66, F, HHL), adding that setting aside time for exercise would be “selfish”. For this participant, the behavioural substitution format of the action plan did not address their main barrier. However, creating the plan did seem to help this participant clarify the barriers they faced (for example, setting boundaries or navigating social and family roles) and perhaps prompting them to find ways to get around them:it's not hard [to do the exercise action plan] but it's just like, okay I can get this much work or studying done or this much work done in this hour [instead of exercising]. So I just keep telling myself, okay, I'll [exercise] next week (P7, 46, F, LHL)
…So I should do [the dance video] when I come home. I think I might have to start saying that [to my family]. Yep. I'll say to all of them, bugger off this is my time, because I'm a selfish old lady now (P19, 66, F, HHL)
3.5 Is the action plan tool easy to use?
Some participants did experience issues. This detracted from how quickly they could go through the plan. For example, some participants found the instructions difficult to understand. These participants would often apologise to the interviewer and/or have to read the instructions more than once, suggesting they felt flustered or confused. These moments slowed down their momentum when using the plan.It's easy to do. It's clear. Not too long-winded (P3, 59, F, LHL)
However, when people experienced these issues, it did not seem to interfere with their overall level of engagement. Minor user experience issues did not appear to affect whether participants saw value in creating an action plan; with the exception of an internet access issue that prevented one participant from using the plan.sorry I think I've done something wrong, it says at the top in red no more than one choice” (P8, 61, F, LHL)
4 DISCUSSION AND CONCLUSION
4.1 Discussion
4.1.1 Key findings
This study outlined key issues that influence how people with varying health literacy needs engage with an online action plan tool to support lifestyle behaviour change for cardiovascular disease prevention. Perceived personal relevance of the tool was important at all stages, from the kinds of behavioural targets offered (snacking, exercising or smoking cessation), through to the specific pre-determined situations and solutions offered to participants to form their plans. Imagining how to enact the different solutions could help people to select the option that was best suited to their daily life. The action plan tool was also used in unintended ways, such as formalising existing plans for healthy habits.
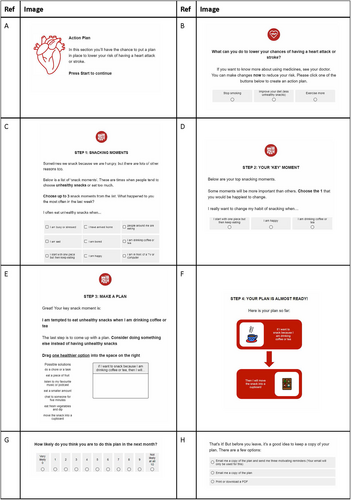
We identified a novel set of questions that behaviour change tool developers can use to ensure that action plans are as relevant and tailored as possible for the target audience, which we formatted into a checklist (Figure 2): (i) is an action plan likely to address the user's key barriers, (ii) is the behaviour target relevant, (iii) would the plan work in real life, (iv) does it match an existing plan and (v) is the planning tool easy to use. The study shows how problem solving and visualisation can help users switch to a more personally relevant plan to overcome potential barriers to behaviour change, even when minor usability issues are encountered.
4.1.2 Links to existing literature
Findings from this study support broader literature on factors that influence the effectiveness of implementation intentions (if-then plans). Previous research has described how intention strength and the salience of cues are important for effective implementation intentions.6, 28 Findings from our study suggest these factors also influence how engaged people feel when creating the action plan. In line with behavioural models such as the health action process approach which posits that a motivational phase precedes the volitional (action) phase,4 this study highlights the importance of bolstering intentions prior to planning and adds that engagement in planning can be further enhanced by emphasising that situations and solutions should be relevant to the user's life.
Previous research has also investigated imagining oneself enacting the action plan,30 often described as “mental contrasting”.41 Studies have found that using this alongside implementation intentions is more effective than either on its own42, 43 (eg, for reducing unhealthy snacking44 and smoking45), perhaps due to increasing clarity about obstacles to changing the unwanted behaviour.44 However, in previous research, participants are encouraged to use mental contrasting to generate appropriate situations and solutions for their behaviour change.43 In this study, we found that the same technique can also help users reflect on the most suitable situation or solution from a list.
Lastly, our findings also showed that some people may need other kinds of support before an action plan will be useful. Such strategies are notably absent from some behavioural models such as the health action process approach4 and may be better captured by broader models such as self-determination theory46, 47 which places a greater emphasis on social relationships.
4.1.3 Strengths and limitations
A strength of this study was the rigorous process used in analysis of the data. Two researchers were involved in analysis, with input from a third researcher, all of whom have experience in qualitative research and developing behaviour change tools. Themes were developed iteratively and the data were returned to continually. A further strength is the inclusion of participants with differing levels of health literacy, providing insight into perspectives that are often absent from digital health research.48
4.1.4 Practical implications
Our study identified that for audiences with varying health literacy levels, designs should include instructions to imagine the plan in order to make sure user's solutions are realistic and achievable. It is also important to have situations and solutions that feel personally relevant to the user, emphasising the importance of involving consumers in intervention design.
Since we found that the action plan format was outside the scope of some participants' needs, implementation efforts should also carefully consider the context in which the action plan is used. For example, patients expressing low motivation or confidence may benefit from education or counselling. Support that more directly influences the patient's access to physical, social and financial resources may also be more appropriate.49 As an online tool, this may involve, for example, identifying other available resources such as free helplines or local walking groups.50
More broadly, the design of the action plan incorporated health literacy design principles throughout (eg, breaking down tasks into smaller steps, using simple language and illustrative images). We also did not observe distinct patterns for people with low and high health literacy. This observation is consistent with a universal precautions approach to health literacy, which argues that everyone benefits from simpler, more accessible health resources.37
4.2 Conclusion
This study qualitatively investigated how people with varying health literacy levels engage with a type of action plan called a volitional help sheet. It supports previous quantitative literature in the field and provides new findings, highlighting the importance of imagining plans and the need to consider alternative behaviour change strategies if the plans are unlikely to address the user's main barriers.
ACKNOWLEDGMENT
This study was funded by a Vanguard Grant from the National Heart Foundation of Australia (ID 102215). Open access publishing facilitated by The University of Sydney, as part of the Wiley - The University of Sydney agreement via the Council of Australian University Librarians.
CONFLICT OF INTEREST STATEMENT
JA and CB are directors of a health literacy consultancy (Health Literacy Solutions Ltd, Pty). The company provides health literacy advice to health services/organisations to support increased access to health information for low literacy adults. Any revenue raised is used to support the development of tools to support health literacy document design. No personal income is received by JA or CB.
ETHICS STATEMENT
This study has Ethics Approval from the University of Sydney Human Research Ethics Committee (ID 2019/774).
Appendix A
See Table A1.
| Participant | Age | Gender | CVD risk percentage | Health literacy | Behavioural target | Situation | Solution |
|---|---|---|---|---|---|---|---|
| 1 | 59 | Female | 5 | inadequate | Snacking | I am drinking coffee or tea | eat a piece of fruit |
| 2 | 51 | Female | 0 | inadequate | Snacking | I have a craving | eat a piece of fruit |
| 3 | 59 | Female | 5 | inadequate | Smoking | I am stressed | think of what this means for people I care about |
| 4 | 65 | Female | 2 | inadequate | Exercise | I am in pain | ask someone to come with me |
| 5 | 66 | Male | 8 | inadequate | Snacking | I am in front of a TV or computer | eat a piece of fruit |
| 6 | 56 | Male | 1 | inadequate | Snacking | I have arrived home | eat a piece of fruit |
| 7 | 46 | Female | 1 | inadequate | Exercise | I am too busy | tell myself that exercising will make me a healthier happier person |
| 8 | 61 | Female | 3 | inadequate | Exercise | I feel lazy | tell myself that exercising will make me a healthier happier person |
| 9 | 72 | Male | 7 | inadequate | Snacking | I am drinking coffee or tea | move the snack into a cupboard |
| 10 | 57 | Male | 8 | inadequate | Snacking | I am in front of a TV or computer | eat a piece of fruit |
| 11 | 63 | Female | 3 | adequate | Snacking | it is part of a celebration or special event | eat fresh vegetables and dip |
| 12 | 74 | Male | 6 | adequate | N/A | N/A | N/A |
| 13 | 72 | Female | 4 | adequate | Snacking | I am drinking coffee or tea | eat a smaller amount |
| 14 | 51 | Female | 0 | adequate | Exercise | I am too tired | do a short exercise at home |
| 15 | 72 | Male | 12 | inadequate | Snacking | I have a craving | drink a large glass of water |
| 16 | 69 | Female | 0 | adequate | Snacking | I want to reward myself | drink a large glass of water |
| 17 | 54 | Female | 2 | adequate | Snacking | I am busy or stressed | listen to my favourite music or podcast |
| 18 | 54 | Male | 1 | adequate | Snacking | it is part of a celebration or special event | eat fresh vegetables and dip |
| 19 | 66 | Female | 4 | adequate | Exercise | I don't feel motivated | think of how my inactivity affects those around me |
| 20 | 55 | Male | 9 | adequate | Snacking | I have a craving | eat a smaller amount |
Open Research
DATA AVAILABILITY STATEMENT
All data are included in this published article (and its supplementary information files).