Exercise at an onsite facility with or without direct exercise supervision improves health-related physical fitness and exercise participation: An 8-week randomised controlled trial with 15-month follow-up
Abstract
Issue addressed
Physical activity and exercise participation is limited by a perceived lack of time, poor access to facilities and low motivation. The aim was to assess whether providing an exercise program to be completed at the workplace with or without direct supervision was effective for promoting health-related physical fitness and exercise participation.
Methods
Fifty university employees aged (Mean ± SD) 42.5 ± 11.1 years were prescribed a moderate- to vigorous-intensity aerobic and resistance exercise program to be completed at an onsite facility for 8 weeks. Participants were randomly allocated to receive direct exercise supervision or not. Cardiorespiratory fitness (V̇O2max) and maximal muscular strength were assessed at baseline and 8 weeks. Self-report physical activity was assessed at baseline, 8 weeks and 15 months post-intervention.
Results
Attendance or exercise session volume were not different between groups. Cardiorespiratory fitness (Mean ± 95% CI); +1.9 ± 0.7 mL·kg·min−1; P < .001), relative knee flexion (+7.4 ± 3.5 Nm·kg−1%; P < .001) and extension (+7.4 ± 4.6 Nm·kg−1%; P < .01) strength increased, irrespective of intervention group. Self-reported vigorous-intensity physical activity increased over the intervention (mean ± 95% CI; +450 ± 222 MET·minutes per week; P < .001), but did not remain elevated at 15 months (+192 ± 276 MET·minutes per week).
Conclusion
Providing a workplace exercise facility to complete an individually-prescribed 8-week exercise program is sufficient to improve health-related physical fitness in the short-term independent to the level of supervision provided, but does not influence long-term participation.
So what?
Lower cost onsite exercise facility supervision is as effective at improving physical health and fitness as directly supervised exercise, however ongoing support may be required for sustained physical activity behaviour change.
1 INTRODUCTION
Physical inactivity1 and low cardiorespiratory fitness (CRF)2 are significant cardiovascular, metabolic and mortality risk factors; with evidence that CRF has a greater effect on cardiovascular risk reduction than physical activity per se.3 Independent of traditional cardiovascular risk factors such as age, smoking, family history of premature coronary heart disease, diabetes, hyperlipidaemia and hypertension, people with low CRF have a 2- to 3-fold increase in mortality risk.2, 4 Increased mortality risk is additionally associated with low muscular strength,5 which is a greater predictor of mortality than muscle mass.6 Despite these well-recognised risks and the widely documented physical and psychological benefits associated with an active lifestyle,7 41% of men and 48% of women living in high-income countries fail to meet advocated aerobic physical activity targets.8 Furthermore, even fewer adults meet the recommendations for muscle-strengthening activity.9 Given the substantial costs of managing the increasing burden of chronic diseases, facilitating exercise participation as a health promotion strategy is needed to improve known modifiable risk factors including physical activity, CRF and muscle strength.
A lack of time and access to facilities are commonly reported barriers to increasing exercise participation and improving health.10 Onsite workplace exercise programs have the potential to overcome these barriers for large numbers of individuals given that two-thirds of adults in developed countries have ongoing employment, and as such, the World Health Organisation recommends the workplace as a setting for exercise promotion.11 Furthermore, improved health through health promotion programs offer potential benefits for both the employee and employer by reducing the burden of employee health issues (absenteeism), moderating medical costs, increased productivity and boosting employee morale.12 Universities may be advantageous settings in which to investigate workplace exercise participation strategies as these institutions often possess existing infrastructure, resources and expertise required to deliver and monitor appropriate exercise or health-promotion programs.13 Small-to-moderate magnitude increases in physical activity levels and reductions in cardiometabolic disease risk factors have been observed following onsite workplace exercise interventions.14-16 However, there is an absence of longitudinal follow-up data investigating the effect of short to moderate duration onsite exercise programs with or without direct exercise supervision on continued physical activity participation and ongoing physical health outcomes.17
Sustained increased exercise participation is required to maintain the myriad of associated physical health benefits.7, 18 Studies involving people with intermittent claudication19 and obesity20 have reported increased participation, greater health (fat loss)20 and improved fitness (maximal walking distance)19 with supervised compared to unsupervised (home-based or completing a prescribed program at a gym without direct supervision) exercise after 6 weeks to 12 months. Improved exercise participation and health might be achieved with supervision through increased participant motivation19 and exercise adherence.20 In contrast to these findings in clinical non-workplace populations, exercise studies involving office workers with neck and shoulder pain and overweight-obese individuals from the community did not find any greater improvements to musculoskeletal21 or metabolic22 outcomes respectively, for supervised compared to minimally supervised (ie, supervision for the first 2 weeks only) or unsupervised (instruction provided at program commencement only) resistance21 and combined aerobic and resistance22 exercise over 5 and 6 months. Therefore, the effectiveness of direct exercise supervision to improve long-term physical activity behaviour and associated cardiometabolic risk factors in apparently healthy populations over and above the provision of an exercise program to complete at an onsite exercise facility without direct individual supervision, remains unknown. Direct exercise supervision however, is expensive to administer. If direct exercise supervision is no more effective than providing access to an onsite exercise facility in promoting ongoing exercise adherence along with health and fitness improvements, there is little value in implementing this as a broad health promotion strategy. Given the limited effect of previous interventions to date,13 and the potential adherence and health benefits that direct exercise supervision might offer, it is pertinent to establish the effectiveness of providing direct (1:1) exercise supervision as a health promotion strategy as opposed to only providing an onsite facility in which to complete a prescribed exercise program. Therefore, the aim of this study was to assess whether providing an exercise program to be completed at the workplace with or without direct supervision was effective for improving CRF and muscle strength. This study further investigated whether such participation was effective for increasing physical activity participation both over the short and longer-term.
2 METHODS
2.1 Study population and design
This 8-week parallel group, randomised controlled trial with 15-month self-report follow-up (ACTRN12613000453785) was conducted from April 2013 to March 2015 in accordance with the CONSORT statement.23 Recruitment took place by advertisement on the university research webpage, flyers placed throughout campus buildings and employee mailboxes. Interested employees provided written informed consent to participate in the study, which was approved by the university Human Research Ethics Committee. Computer-generated concealed randomisation stratified by sex was used to allocate 50 university employees from a single Australian university campus to either directly supervised exercise (SUP; n = 25) or exercise without direct supervision (CON; n = 25) following baseline testing. Randomisation was implemented using individual opaque envelopes by a person independent of the investigators. Individuals aged 18-65 years, currently employed by the university and free from any condition for which exercise is contraindicated24 were eligible for participation. Limitations of funding and expertise dictated that assessors conducting outcome testing were not blinded to participant grouping. Physical activity behaviour was followed up at 15 months by self-report questionnaire. Primary outcomes were CRF, muscular strength and exercise volume (exercise session attendance, aerobic and resistance training volume). Secondary outcomes were body mass, waist circumference and physical activity behaviour (walking, moderate and vigorous-intensity physical activity). All participants were instructed to maintain their usual dietary intake and to avoid strenuous exercise for the 48 hours prior to each testing session.
Cardiometabolic assessments of total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), triglycerides (TG), glucose and high-sensitive C-reactive protein (CRP) were conducted at baseline using Roche Cobas c701 and c502 instruments. Low-density lipoprotein cholesterol (LDL-C) was calculated using the Friedewald equation.25 Anthropometric measurements (body mass, stature, waist circumference and body mass index) were measured at baseline and after the 8-week intervention using standardised protocols.24
2.2 Exercise capacity
Cardiorespiratory fitness was assessed using a multi-stage protocol24 on a cycle ergometer (Monark 828E, Sweden). Following a 3-minute warm-up (work-rate (watts):body mass (kg) ratio = 0.5:1), each subsequent 3-minute stage increased by 25 W until the participant reached 85% of their predicted maximum heart rate (HRmax), estimated using the equation: HRmax = 206.9-(0.67 × age).24 Maximal oxygen consumption (V̇O2max; mL·kg·min−1) was estimated with a validated equation at each stage and extrapolated to predicted HRmax.24
Maximal knee flexion and extension strength were assessed by isokinetic dynamometry (Biodex Medical Systems, USA) using a standardised setup.26 Following 5 submaximal warm-up/familiarisation repetitions and 2 minutes of passive rest, 5 maximal concentric knee flexion and extension repetitions at 60°sec−1 were performed, with verbal encouragement provided by the assessor. Upper body strength (isometric grip strength of the dominant hand) was assessed using a digital hand-held dynamometer (Jamar Plus, Patterson Medical, Bolingbrook, IL) with the elbow at 90 degrees flexion and the maximum of three trials recorded.27
2.3 Exercise volume and physical activity behaviour
Exercise session duration, mode, intensity (cycling watts, walking and jogging speed) and RPE were recorded for aerobic exercises and for any activities performed outside of the study. Aerobic training volume and activities performed outside of the study were calculated as MET·minutes of energy expenditure using the compendium of physical activities.28 Sets, repetitions, weight and RPE were recorded for resistance exercises. Resistance training volume (kg) was calculated using the equation: sets × repetitions × mass lifted (kg).29 The short-form International Physical Activity Questionnaire (IPAQ)30 was used to assess physical activity behaviour at baseline, after the 8-week intervention and at 15-month follow-up and compared with current recommendations.31 Weekly energy expenditure (MET.min) was calculated using the validated IPAQ formula32 to classify individual physical activity levels.
2.4 Exercise supervision
Participants were required to complete a minimum of one and a maximum of 5 onsite exercise sessions per week at any of the following gymnasium opening times that suited them on any given day (0730-0930; 1130-1400; and 1600-1830; Monday to Friday). Direct individual (1:1) supervision for every exercise session was provided to those allocated to SUP. Those allocated to CON received access to an exercise facility in which to complete the prescribed exercise, overseen by floor staff for safety, with assistance provided only if requested or required as is typical in a standard gym setting. The exercise programs were prescribed and implemented by the same accredited exercise physiologist who guided all participants through their individual program at the beginning of the intervention, and at the beginning of week 5 when new exercises targeting the same muscle groups were introduced. Trained undergraduate exercise science students assisted with the day-to-day delivery of the programs (ie, provided the exercise supervision for SUP and facility supervision for CON) under the guidance of an accredited exercise physiologist. No dietary advice was provided to participants.
2.5 Exercise programming
Each participant was prescribed an 8-week moderate- to vigorous-intensity progressive aerobic and resistance exercise program at an onsite gymnasium, using American College of Sports Medicine (ACSM) guidelines for mode and intensity prescription.24 Participants were able to select their frequency of participation. 20-30 minutes of aerobic exercise (stationary cycling and outdoor walking and jogging) was prescribed in each session at 64-74% of HRmax for the initial 4 weeks and progressed to 74%-91% HRmax.24 Three sets of 8-12 repetitions of a combination of 3 multi-joint (eg, bench press, squat and lunge) and 3 single-joint (eg, bicep curl, calf raise and abdominal curl) resistance exercises for the development of upper- and lower-body muscular strength were also prescribed in each session with a between-set rest period of 30-120 seconds.24 Resistance load was adjusted to maintain an intensity of 15-18 on the Borg RPE scale.33
2.6 Statistical analysis
All data were analysed using the Statistical Package for Social Sciences (SPSS for Windows, vers. 24.0, SPSS Inc., Chicago, IL, USA). Data were inspected visually and statistically for normality prior to analysis, and are presented as mean ± SD unless otherwise indicated. An alpha level of 0.05 was set as significant for all statistical testing. An a priori sample size calculation using previous literature22 suggested 100 participants were required, however post-hoc power calculations for change to CRF between groups on data collected up until the summer break indicated an effect size double that utilised for the a priori calculation (0.53 with 99% power from our sample of 50 participants); therefore recruitment was discontinued.
To assess the effect of the intervention on fitness and anthropometric outcomes, two-way (supervision × time) ANOVA were conducted using an intention-to-treat method whereby missing values were substituted with the last known observation. Findings from per-protocol analyses excluding the four withdrawals (SUP n = 3, CON n = 1) were not different to intention-to-treat analyses, therefore only intention-to-treat analyses are presented. Sex, working hours and employment role have previously been shown to not influence the physical activity levels of university employees,34 therefore were not included as covariates in the two-way ANOVA analyses. Effect sizes (ES) are reported to indicate the magnitude of the effects. Partial eta squared are reported to better account for within group variation with a value of ≤0.06 indicating a small effect, between 0.06 and 0.14 indicating a moderate effect, and >0.14 indicating a large effect.35 Pearson's correlation coefficient (r) was used to assess effect size for non-normally distributed physical activity outcomes. Independent t tests (two-tailed) compared overall training volume completed during the 8-week intervention. Repeated measures analyses of variance (ANOVA) were used to investigate attendance throughout the intervention period.
Physical activity behaviour (ie, walking, moderate, vigorous and total physical activity) were analysed using non-parametric tests (Friedman with Wilcoxon Signed Rank post-hoc) to assess change in the 34 participants (SUP = 15; CON = 19) who completed follow-up at 15 months. Mann-Whitney's U-test compared physical activity between groups at each time point (ie, baseline, 8 weeks and 15 months), and also the change in physical activity for walking, moderate, vigorous and total physical activity between groups across each time period. A Chi-square test investigated associations between supervision and physical activity behaviour at baseline, post and 15 months after the exercise program. Cochrane's Q test investigated changes in the proportion of participants meeting physical activity guidelines across the three time-points. A standard multiple regression was used to determine the predictors of physical activity behaviour at 15-month follow-up, using change in CRF, strength and anthropometric measures as the postulated independent predictors.
3 RESULTS
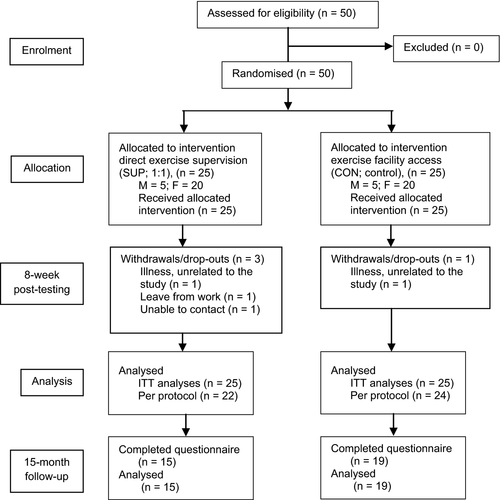
Participant recruitment and withdrawals are presented in Figure 1, and participant baseline characteristics are presented in Table 1. Nineteen participants completed at least one exercise session every week in accordance with the prescribed minimum (SUP = 10; CON = 9). Cardiorespiratory fitness, relative isometric grip strength, and both relative isokinetic knee flexion and extension strength significantly increased over the 8-week intervention (P < .01; partial eta squared effect sizes ranged from 0.16 to 0.41; large effects) with no interaction or group effects (Table 2). The exercise intervention reduced waist circumference (P < .001) with no interaction or group effects, but did not change body mass at the immediate 8-week follow-up (Table 2). Aerobic training volume (mean ± SD; SUP = 1610 ± 1268; CON = 1487 ± 1219 MET·minutes per week; P = .73), resistance training volume (mean ± SD; SUP = 35 858 ± 27 999 kg; CON = 34 659 ± 26,189 kg; P = .88) and other physical activities (mean ± SD; SUP = 3002 ± 3712; CON = 2786 ± 7169 MET·minutes per week; P = .90) completed over the intervention period were not different between supervision groups.
| Exercise group | ||
|---|---|---|
| SUP (n = 25) Mean ± 95% CI | CON (n = 25) Mean ± 95% CI | |
| Sex (male/female) | 5/20 | 5/20 |
| Age (years) | 42.2 ± 4.3 | 42.8 ± 4.9 |
| Height (cm) | 168.1 ± 3.3 | 168.0 ± 4.1 |
| Body mass (kg) | 74.6 ± 6.0 | 71.2 ± 5.4 |
| BMI (kg·m−2) | 26.3 ± 1.7 | 25.2 ± 1.6 |
| Waist circumference (cm) | 86.5 ± 5.6 | 83.1 ± 4.9 |
| High-sensitive CRP (mg·L−1) | 3.3 ± 1.6 | 1.5 ± 0.5 |
| Glucose (mmol·L−1) | 5.2 ± 0.3 | 5.1 ± 0.1 |
| Total cholesterol (mmol·L−1) | 5.1 ± 0.3 | 5.0 ± 0.4 |
| Triglycerides (mmol·L−1) | 1.2 ± 0.3 | 1.2 ± 0.2 |
| LDL cholesterol (mmol·L−1) | 3.0 ± 0.4 | 3.0 ± 0.4 |
| HDL cholesterol (mmol·L−1) | 1.54 ± 0.19 | 1.41 ± 0.21 |
- CON, control group; SUP, directly supervised group; n = number of subjects.
| SUP (n = 25) | CON (n = 25) | Effects (group) | Effects (time) | Effects (group × time) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Δ | Pre | Post | Δ | P | P | Mean ± 95% CI | P | |
| Fitness (primary) outcomes | ||||||||||
| Predicted V̇O2max (mL·kg·min−1) | 24.1 ± 1.5 | 25.7 ± 1.8 | 1.6 ± 0.8 | 23.0 ± 2.1 | 25.2 ± 2.2 | 2.2 ± 1.1 | .53 | <.001** | 1.9 ± 0.7 | .32 |
| Relative isometric grip strength (kg·kg body mass) | 0.49 ± 0.14 | 0.51 ± 0.13 | 0.02 ± 0.03 | 0.50 ± 0.11 | 0.54 ± 0.13 | 0.03 ± 0.04 | .523 | <.001* | 0.03 ± 0.01 | .331 |
| Relative isokinetic knee extension strength at 60 deg·sec−1 (Nm·kg %−1) | 193.8 ± 20.6 | 200.6 ± 19.2 | 6.8 ± 5.7 | 195.7 ± 22.8 | 203.6 ± 19.8 | 7.9 ± 7.5 | .86 | <.01* | 7.4 ± 4.6 | .81 |
| Relative isokinetic knee flexion strength at 60 deg·sec−1 (Nm·kg %−1) | 98.0 ± 10.3 | 105.3 ± 12.1 | 7.3 ± 5.8 | 101.3 ± 12.5 | 108.9 ± 13.0 | 7.6 ± 4.4 | .67 | <.001** | 7.4 ± 3.5 | .94 |
| Anthropometric (secondary) outcomes | ||||||||||
| WC (cm) | 86.5 ± 5.6 | 84.4 ± 5.3 | −2.0 ± 1.2 | 83.1 ± 4.9 | 81.2 ± 4.6 | −1.9 ± 1.1 | 0.35 | <.001** | −1.97 ± 0.77 | .86 |
| Body mass (kg) | 74.6 ± 6.0 | 74.5 ± 6.0 | −0.1 ± 0.8 | 71.2 ± 5.4 | 71.6 ± 5.4 | 0.4 ± 0.5 | 0.42 | .60 | 0.12 ± 0.47 | .27 |
- Δ, change; CI, confidence intervals; deg·sec−1, degrees per second; CON, exercise facility access only group; (mL·kg·min−1), millilitres of oxygen consumed per kg body mass per minute; (Nm), Newton-meters of torque; (Nm·kg-1 %), Newton-meters of torque as a percentage of body mass; SUP, directly supervised exercise group; WC, waist circumference. Analysis based on intention to treat; n = 25 for SUP group, n = 25 for CON group. Data are presented as mean values ± 95% CI. P values using between-within analysis of variance. Bold font indicates statistical significance (*P < .01; **P < .001). Predicted V̇O2max measured using submaximal cycle test. Isokinetic knee strength measured using Biodex. Grip strength measured using handheld dynamometer.
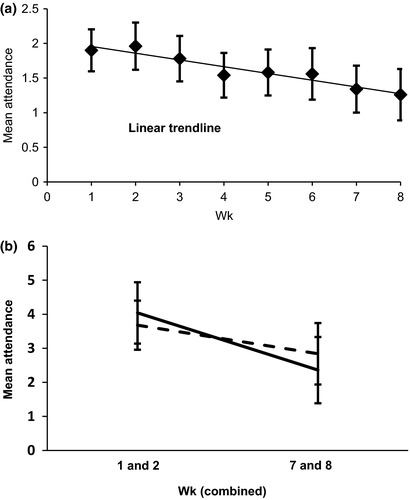
Mean number of sessions attended throughout the intervention was 13.0 ± 8.7 and 12.8 ± 7.1 for SUP and CON groups respectively (equating to an average of 1.6 sessions per week for both groups), with no between-group differences (P = .94). There were no interaction or group effects for attendance, although a negative trend in weekly session attendance throughout the intervention was observed (P < .001; Figure 2A; pooled data). Attendance decreased by a mean 0.06 sessions per week per participant, or 0.5 sessions from week 1 to week 8. Summed training attendance were compared between weeks 1 and 2 and weeks 7 and 8 with a significant time effect (P < .001) confirmed, but no significant interaction or group effects (Figure 2B).
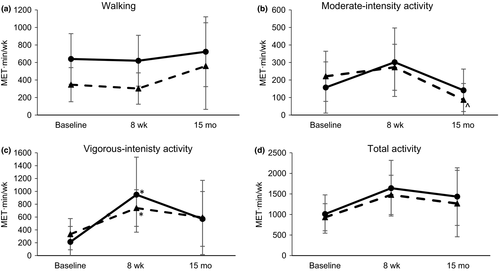
Of the 46 participants (SUP: n = 22; CON: n = 24) who completed the 8-week intervention, 34 (74%) completed the 15-month self-report follow-up. Baseline characteristics were similar between those who did and did not complete the follow-up questionnaire. There was a significant increase in self-reported weekly vigorous-intensity activity from baseline to 8 weeks for both SUP (mean ± 95% CI: +720 ± 595 MET·minutes per week; P = .011; r = .47; medium ES) and CON (+407 ± 246 MET·minutes per week; P = .005; r = .47; medium ES) groups, but no changes in walking, moderate-intensity or total physical activity over this time period. There was a significant decrease in moderate-intensity activity from 8 weeks (post-intervention) to 15-month follow-up for the CON (−188 ± 163 MET·minutes per week; P = .025; r = .37; medium ES) group, which was the only change in physical activity behaviour during this time period. There was a significant change in the proportion of participants reporting meeting physical activity guidelines (P = .04) from baseline (59%), to 8 weeks (82%), to 15-month follow-up (59%), which was not associated with the type of supervision received during the 8-week intervention (Figure 3). Furthermore, no statistically significant differences were identified in physical activity participation at any time point between supervision groups, or in the magnitude of change in physical activity between groups (Figure 3). A greater reduction in BMI over the 8-week intervention was associated (P < .05) with higher weekly vigorous-intensity physical activity at 15-month follow-up.
4 DISCUSSION
Improvements to employee CRF, muscle strength and waist circumference were achieved from an 8-week workplace exercise program, with no greater benefit received by providing direct exercise supervision in addition to access to an onsite exercise facility and prescribed exercise program. The equivalent health and fitness improvements are likely explained by the similar mean exercise session attendance and training volume completed by each group. Furthermore, direct supervision did not lead to greater physical activity behaviour at 15-month follow-up than simply providing an onsite exercise facility and prescribed exercise program.
The improvements to health-related physical fitness during this exercise program support previous research involving 8-12-week exercise interventions in blue- and white-collar workplaces that provided standard exercise supervision.36, 37 Low CRF has been identified as an important independent cardiovascular and all-cause mortality risk factor in both men and women, and even small increases to CRF are associated with reduced mortality.38, 39 Overall, a large effect was observed for CRF improvements in this study. Furthermore, 14 participants improved predicted V̇O2max by 3.5 mL·kg·min−1 (1 MET) or more, a magnitude shown to lower all-cause mortality risk by 8%-14%.38 The remaining 36 participants attended 1.5 ± 1.0 sessions per week for an average CRF improvement of 0.8 ± 1.5 mL·kg·min−1, therefore they are still likely to have experienced reductions in all-cause mortality risk but to a lesser extent than participants who averaged two sessions per week. This finding suggests a minimum frequency of two prescribed and supervised exercise sessions per week are required to achieve the greatest improvements to health through CRF in the short term (8 weeks). Muscular strength is also a key predictor of morbidity and mortality and large overall effects were observed for improvements to both upper and lower body strength. Similarly, previous randomised controlled trials have reported significant strength improvements in university,36 pharmaceutical40 and high-tech company41 employees following exercise interventions of 8-12 weeks in duration conducted at the workplace. Irrespective of the type of supervision provided in this study it did not encourage the majority of participants to meet the current ACSM exercise frequency guidelines for improving CRF and strength.
The current findings suggest that direct exercise supervision may not confer any additional attendance, training volume, health-related physical fitness or physical activity improvements over and above providing a prescribed exercise program and access to an onsite exercise facility over 8 weeks in healthy university employees. Exercise interventions involving obese20 and chronic obstructive pulmonary disease patients42 have demonstrated greater exercise adherence,20 health20 and physical capacity improvements42 after 4-6 months when exercise is directly supervised. Equivalent longer-term follow-up data are not available in apparently healthy individuals to allow comparison of the outcomes reported in this study. It is possible that any additional benefits that may be achieved by providing direct exercise supervision will only become apparent after an extended period greater than eight weeks.
A limiting factor to the effectiveness of many previous exercise interventions is poor compliance, particularly over extended durations.43, 44 Previous 6-month exercise interventions involving ≥3 sessions per week conducted in the workplace with standard exercise facility supervision involving apparently healthy employees report dropout rates of 27%43 and 40%.44 Participant retention was similar between exercise supervision groups in this study (SUP = 88%; CON = 96%). However, whether greater retention or exercise training volume is achieved by providing direct exercise supervision compared with only the provision of an exercise facility and training program over a longer period of time (eg, 6-12 months) is unknown. Given the cost implications of delivering exercise with varying levels of supervision, an understanding of the long-term costs and benefits associated with providing an onsite exercise facility with the capacity for direct exercise supervision is warranted.
Of further interest is whether longer interventions have a greater effect on long-term physical activity participation. Although there were no significant changes to total physical activity behaviour with the intervention, 59% (baseline), 82% (8 weeks) and 59% (15 months) of participants in this study self-reported achieving the minimum 500-1000 MET·minutes of weekly physical activity-related energy expenditure reported to concur health benefits.45 This shows that while a short-term workplace exercise intervention was able to increase physical activity participation, this was not maintained with participants reverting back to their previous physical activity behaviour after 15 months, regardless of the type of exercise supervision they received during the intervention. It must be acknowledged that the actual proportion of employees meeting physical activity guidelines at each time point may have been lower, as self-report measures of physical activity participation are prone to measurement error.46 Specifically, adults have been shown to over-report walking, moderate- and vigorous-intensity physical activity using the short-form IPAQ.47 Nevertheless, the current findings suggest that additional support such as access to an onsite supervised exercise facility may be required to maintain ongoing exercise behaviour. Furthermore, although there were no significant changes in body mass over the 8-week intervention, a decrease in BMI was positively associated with higher levels of vigorous-intensity physical activity participation at 15-month follow-up, indicating that even small amounts of weight loss and a change to body composition had a positive effect on long-term behaviour. An increase in grip strength was negatively associated with long-term moderate-intensity physical activity participation. Increased strength might have meant moderate-intensity activity was supplemented with higher levels of vigorous-intensity activity.
5 CONCLUSION
Providing a suitable workplace exercise facility with appropriate exercise prescription was sufficient to increase short-term vigorous-intensity physical activity participation, CRF and muscle strength. Access to an onsite exercise facility therefore presents a worthwhile health promotion strategy for employers wanting to increase employee physical activity behaviour and improve cardiometabolic health. Clinically meaningful increases to CRF and muscle strength can be achieved by performing an average of two exercise sessions per week for 8 weeks, with exercise session volume or facility attendance not affected by direct exercise supervision. Furthermore, a short-term workplace exercise program with or without direct exercise supervision and support does not result in sustained changes to physical activity participation, therefore additional strategies such as ongoing guidance and support may be required to bring about long-term behaviour change, particularly for employees with low physical activity levels.
ACKNOWLEDGEMENTS
The authors would like to acknowledge Dr James Baglin and Dr Stella Stylianou for their statistical advice, the undergraduate exercise science student leaders who assisted in the delivery of this intervention, and the university staff who participated. This work was supported by internal funding from the School of Health and Biomedical Sciences, RMIT University, Australia, and the lead author was supported by the Australian Postgraduate Award. Trial registration number: Australian New Zealand Clinical Trials Registry (ACTRN12613000453785).
CONFLICT Of INTEREST
The authors declare that there are no financial disclosures or conflicts of interest in connection with this article.
AUTHOR CONTRIBUTIONS
Study conception: JRH, BAG, ACB. Study design: JRH, BAG, NL, SRB, ACB. Acquisition, analysis or interpretation of data: JRH, BAG, SRB, ACB. Drafting of manuscript: JRH. Critical revision of manuscript: JRH, BAG, NL, SRB, ACB. All authors have read and approved the final version of the manuscript, agree to be accountable for all aspects of the work and agree with the order of presentation of the authors.