REPLY:
We appreciate the interests and comments by A. Kulkarni et al. In our study, in intention-to-treat (ITT) analysis, there was a greater number of hepatorenal syndrome (HRS) candidates in the ITT-deceased donor liver transplantation (ITT-DDLT) group compared to the ITT-living donor liver transplantation (ITT-LDLT) group (65.5% vs. 53.8%, respectively; P = 0.034).(1) This was a result of a longer waiting time in the ITT-DDLT group. With LDLT, the median waiting time was only 7 days. LDLT allowed an earlier access to transplant, and in a such setting, the response to terlipressin became less relevant given that patients would be transplanted once a live donor was available.
Hepatitis B remains the most common indication for transplantation at our locality. Currently, we do not adopt any bridging therapies, such as artificial liver support systems. Although they may not increase overall survival, we agree that it may lengthen the window of opportunity for transplant. Only 13 patients (8 [7.1%] in ITT-DDLT and 5 [2.4%] in ITT-LDLT) in our study had decompensated alcohol-associated cirrhosis and none had alcohol-associated hepatitis, given that active drinking in patients with alcohol use disorder would preclude liver transplantation currently at our center. With the recent evidence showing that survival can be significantly improved for a highly selected subgroup, consideration is now given for early transplantation, but only in highly selected persons and with an available living donor.
We agree that the major advantage of LDLT is the significantly shortened time to transplant.
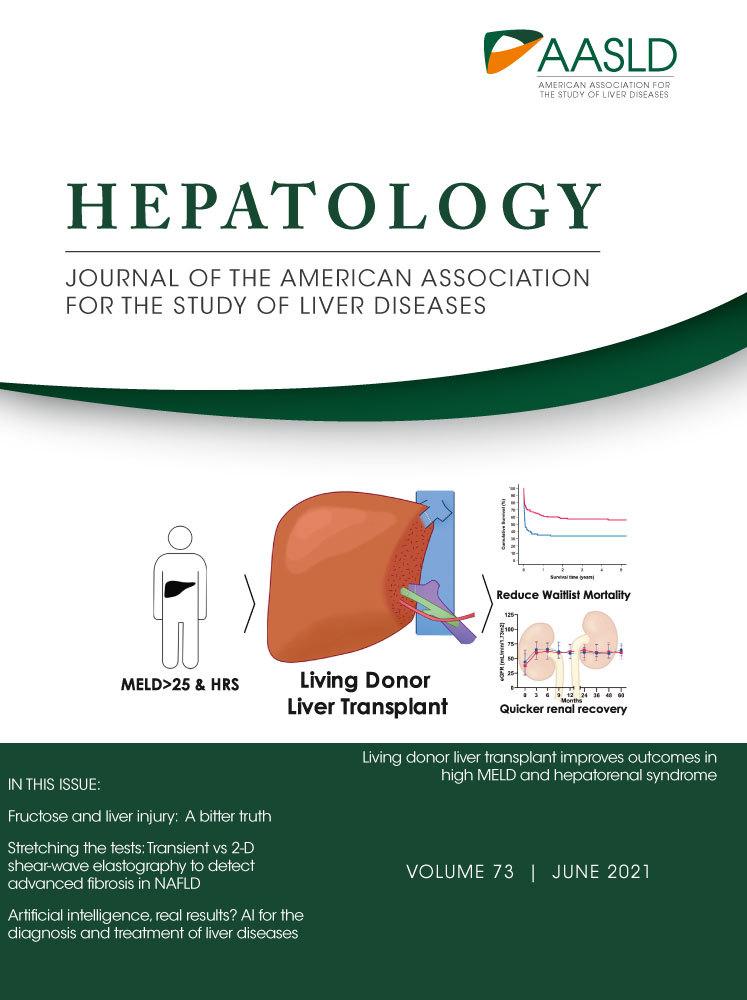
In our study, we have demonstrated that LDLT approach reduced waitlist mortality by providing an earlier access to transplant, particularly within the first month after listing when mortality risk without transplant was the highest. This is particularly important for regions such as ours whereby donor organs remain scarce, and we have to rely on LDLT as an additional source of organs in addition to DDLT. LDLT is not common in many parts of the world given that it requires more intensive training, together with the perceived risk to the donor. However, LDLT is a well-established treatment in parts of Asia and remains an essential component in many transplant centers. Therefore, as A. Kulkarni et al. suggested, it is important to educate and provide training for LDLT, especially in regions where organ availability remains low.
Author Contributions
T.C.L.W. and J.Y.Y.F. were responsible for drafting, interpretation and review of the manuscript.