Hepatocellular carcinoma complicating hepatitis E virus–related cirrhosis
Potential conflict of interest: Nothing to report.
Abbreviations
-
- HCC
-
- hepatocellular carcinoma
-
- HEV
-
- hepatitis E virus
Hepatitis E virus (HEV) was revealed in 2008 as a new cause of chronic hepatitis and cirrhosis in immunocompromised patients.1, 2 Chronic hepatitis E results in liver inflammation and fibrosis that may lead to liver cirrhosis. To date, however, no case of HEV-related hepatocellular carcinoma (HCC) has been reported. We present a case of HCC complicating chronic hepatitis E.
Clinical Observation
A 65-year-old man was diagnosed with a liver mass by ultrasonography in November 2015. This patient had been treated for follicular lymphoma between 1999 and 2004 (rituximab, cyclophosphamide, doxorubicin [hydroxydaunomycin], vincristine [oncovin], and prednisone, followed by autologous stem-cell transplantation and rituximab). Since May 2004 the patient was considered cured of his lymphoma and did not receive specific therapy. However, he presented cerebral toxoplasmosis, necessitating surgical therapy in December 2005, with a relapse in November 2006 that was medically treated. At admission, biological tests showed liver cytolysis (alanine aminotransferase, 164 IU/L; aspartate aminotransferase, 117 IU/L; gamma-glutamyltransferase, 246 IU/L; alkaline phosphatase, 91 IU/L). Serum bilirubin (3 µmol/L), albumin (43 g/L), and international normalized ratio (0.94) were normal. Serum alpha-fetoprotein level was 50 ng/mL. A computed tomographic scan showed a 25-mm hypervascular liver nodule with a washout during the portal phase. Nontumoral liver biopsy showed histological cirrhosis with mononuclear infiltrate suggestive of chronic viral hepatitis. HCC complicating Child-Pugh A cirrhosis was diagnosed, and the patient underwent tumor resection. At the time of surgery the liver was nodular, and histological examination confirmed cirrhosis and HCC (Fig. 1).
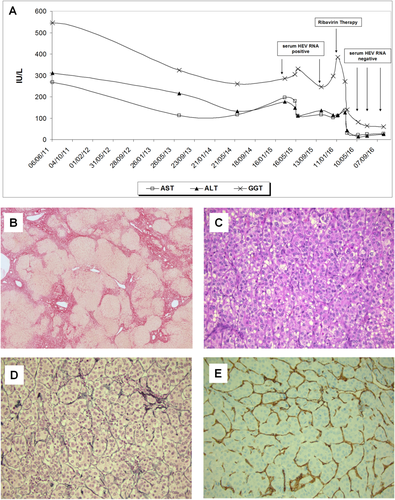
(A) Evolution of liver biological tests. Alanine aminotransferase (ALT), aspartate aminotransferase (AST), and gamma-glutamyltransferase (GGT) levels were found within normal range up to 2004. From 2006 to diagnosis of HCC (November 2015) ALT, AST, and GGT levels fluctuated between 5-fold and 10-fold the normal range. Results are presented from 2011 to 2016. (B-E) Histological examination of liver. (B) Typical pattern of liver cirrhosis in the nontumoral liver showing sirius red staining of collagen, original magnification ×50. (C) Tumor examination showing atypical hepatocytic cellular proliferation. Hematoxylin, phloxine, and saffron staining, ×200. (D) Loss of sinusoidal architecture. Reticulin staining, × 200. (E) Anti–cluster of differentiation 31 immunostaining showing capillarization of tumorous endothelial cells.
Retrospective analysis of liver biological tests showed chronic liver cytolysis since 2007 (Fig. 1). The patient, a butcher, did not report any chronic alcohol intake or uncooked pork meat consumption. All other major etiologies of chronic hepatitis were ruled out: serology for hepatitis B virus and hepatitis C virus was negative. The patient did not present metabolic syndrome, and his body mass index was lower than 25 kg/m2. Serum ferritin was normal, and liver-directed autoantibodies were all negative. HEV testing performed in November 2015 showed the presence of immunoglobulins G and M (Wantai, China) and HEV RNA (quantitative real-time PCR3; 6.2 log10copies/mL) in the serum. In addition, serum collected 6 months earlier tested retrospectively positive for HEV RNA (6.1 log10copies/mL). HEV open reading frame 2 sequencing3 showed that virus was of genotype 3 (GenBank accession no. KX580027-KX580034). HEV RNA was also detected by quantitative real-time PCR in tumorous and nontumorous liver. HEV open reading frame 2 sequences obtained from serum collected at the time of liver surgery and 8 months earlier were 99% identical to each other. Ribavirin therapy administered from January 2016 through March 2016 resulted in the rapid normalization of liver transaminases concurrently with HEV RNA clearance (Fig. 1).
Discussion
In the present observation, chronic hepatitis E developed, although therapy for lymphoma was completed since 2004. This is unusual. Nevertheless, cerebral toxoplasmosis in 2005-2006 and hypogammaglobulinemia at the time of HCC diagnosis indicated that the patient has remained severely immunocompromised. In addition, the absence of other possible etiologies and the rapid normalization of liver tests in parallel with HEV RNA clearance suggest that HEV was the cause of chronic hepatitis in this patient since 2007.
Chronic HEV infection is not a classical cause of HCC. This could be explained by the overall small number of HEV-related chronic hepatitis and cirrhosis cases worldwide3 and the efficacy of ribavirin therapy.4 Thus, in our institution, only 2 patients were diagnosed with HEV-associated cirrhosis, including the present case who developed HCC.5 As suspected for HCV, HEV infection may promote HCC through chronic inflammation. Specific mechanisms involved in liver carcinogenesis remain to be investigated.
In conclusion, HEV joins hepatitis B/C viruses as a potential cause of HCC in chronically infected patients. This observation highlights the importance of diagnosing and treating chronic HEV infection in immunosuppressed patients to prevent evolution toward liver cirrhosis and HCC, and it warrants systematic testing for HEV infection in patients with HCC of unknown cause.