Reply
This study was partly supported by a grant from the Research Grants Council of the Hong Kong Special Administrative Region (project reference CUHK477813).
Potential conflict of interest: Vincent Wai-Sun Wong has served as an advisory board member for Gilead and Janssen and as a consultant for AbbVie, Merck, and Novo Medica; he has also received paid lecture fees from AbbVie, Echosens, Roche, and Gilead. Grace Lai-Hung Wong has served as an advisory board member for Gilead and received paid lecture fees from AbbVie, Bristol-Myers Squibb, Echosens, Roche, Gilead, and Janssen. Henry Lik-Yuen Chan has served as a consultant for Bristol-Myers Squibb, Gilead, Merck, Novartis, and Roche; received paid lecture fees from AbbVie, Bristol-Myers Squibb, Echosens, Gilead, Merck, Novartis, and Roche; and received an unrestricted grant from Roche for hepatitis B research.
We thank Targher and Byrne for their interest in our work.1, 2 If we were to study the general population or a cohort of patients with or without coronary artery disease, nonalcoholic fatty liver disease (NAFLD) would undoubtedly be associated with coronary artery disease and cardiovascular events. Nevertheless, our cohort was unique in that all patients had clinical indications for a coronary angiogram, and the majority had significant coronary artery disease at the baseline. Our study shows that NAFLD is no longer associated with increased cardiovascular events and mortality if we include only patients with cardiac diseases. The differences in the design of our study and previous ones should be noted.
As discussed in our article,1 we fully agree with Targher and Byrne that the relatively low overall and cardiovascular mortality for our patients with NAFLD was likely due to the disease-modifying effect of cardiac interventions and pharmacological therapy. In response to their suggestion, we have performed a further analysis of the effect of a statin. During follow-up, 511 of 612 patients (83.5%) were treated with a statin; they included 324 of 356 NAFLD patients (91.0%) and 187 of 256 controls (73.0%; P < 0.0001). Three hundred ninety-nine patients (65.2%) were treated with a statin at the time of the index coronary angiogram, and 136 patients (22.2%) were started on a statin afterward. Overall, 70 patients (13.7%) on a statin during follow-up and 36 patients (35.6%) not on a statin died (hazard ratio, 0.30; 95% confidence interval, 0.20-0.45; P < 0.0001; Fig. 1A). Cardiovascular mortality occurred in 21 patients (4.1%) on a statin during follow-up and in 6 patients (5.9%) not on a statin (hazard ratio, 0.55; 95% confidence interval, 0.22-1.37; P = 0.20; Fig. 1B). According to a multivariate analysis, statin use during the follow-up period (adjusted hazard ratio, 0.28) and NAFLD (adjusted hazard ratio, 0.49) remained independent factors associated with lower overall mortality, whereas older age, smoking, and diabetes were associated with increased mortality.
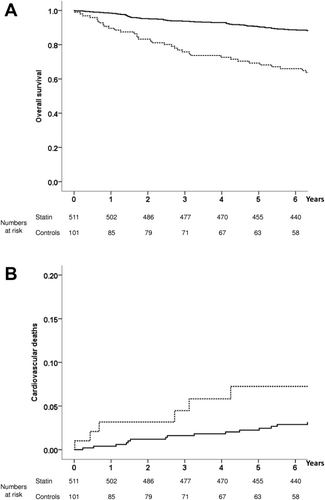
We must, however, highlight that the additional statin analysis is subject to an indication bias and should be interpreted with caution. In any case, our study serves as a timely reminder that the decision on screening for a particular disease should not be based on its prevalence alone.3 As the medical community continues to debate the value of NAFLD screening in different patient groups,4 it should be noted that few patients with cardiac diseases die from liver complications despite a high prevalence of NAFLD, and the presence of NAFLD adds little to the prognostication for such patients.
-
Vincent Wai-Sun Wong, M.D.1,2
-
Grace Lai-Hung Wong, M.D.1,2
-
Henry Lik-Yuen Chan, M.D.1,2
-
1Department of Medicine and Therapeutics
-
Chinese University of Hong Kong
-
Hong Kong
-
2State Key Laboratory of Digestive Disease
-
Chinese University of Hong Kong
-
Hong Kong