Drug-induced postinfantile giant cell hepatitis†
Potential conflict of interest: Nothing to report.
We have read with great interest the article by Björnsson et al.1 on the topic of drug-induced autoimmune hepatitis (AIH). The authors concluded that a significant proportion of patients with AIH have drug-induced AIH. Together with different types of drugs, medicinal herbs and cosmetics may be involved in liver damage.2 Postinfantile giant cell hepatitis (PGCH) is a rare entity secondary to a nonspecific reaction to toxins, drugs, or viruses, although no causative agent has been found in many cases.3, 4 Importantly, several patients have exhibited autoimmune characteristics and have responded to immunosuppressive therapy.5, 6 The clinical spectrum of PGCH is variable; according to some authors,3, 7 the disease in its natural course is usually fulminant and within months progresses to cirrhosis, which will lead to death or a requirement for liver transplantation. However, a benign course in these patients can also be observed. Here we discuss a 38-year-old woman who, having PGCH and features of AIH associated with a drug used to prevent hair loss, responded to corticosteroids plus azathioprine.
The patient, presenting progressive jaundice (total bilirubin level = 28.7 mg/dL) without pain during the previous 3 weeks, was admitted to our hospital. The laboratory investigation revealed elevated serum levels of aspartate aminotransferase (714 IU/L), alanine aminotransferase (465 IU/L), gamma-glutamyltransferase (98 IU/L), and alkaline phosphatase (268 IU/L), and she was positive for antinuclear antibody (titer = 1/160) with normal immunoglobulins. The only relevant previous history was her treatment for more than 10 months with Pil-Food (Laboratorio Serra Pamies, Reus, Spain) to prevent hair loss. An ultrasonography examination found only regular hepatomegaly, and percutaneous liver biopsy was performed. A histological study (Fig. 1) showed not only a conserved architectural structure but also extensive areas of multinucleate giant cells, portal tract enlargement with bridging necrosis, intense inflammation of the parenchyma, and liver cell necrosis with regenerative changes and hyperplasia of the mononuclear phagocytic system. Furthermore, marked intracanalicular and hepatocellular cholestasis was observed. When she was admitted to the hospital, the Pil-Food therapy was stopped, and treatment with ursodeoxycholic acid (14 mg/kg/day) was initiated; substantial analytical changes were not attained. Because of the probable AIH component, a course of methylprednisolone (60 mg/day) was started, and the dose was subsequently tapered until total remission was achieved. As a unique maintenance therapy, azathioprine (50 mg/day initially and 25 mg/day after the first year) was used. In month 12 after the diagnosis and treatment, the biochemical investigation was completely normal (aspartate aminotransferase level = 14 IU/L, alanine aminotransferase level = 12 IU/L, total bilirubin level = 0.5 mg/dL, alkaline phosphatase level = 62 IU/L, and gamma-glutamyltransferase level = 12 IU/L); her antinuclear antibody positivity persisted (titer = 1/80). After more than 5 years of follow-up, the patient's liver test findings continued to be normal, and she remained asymptomatic.
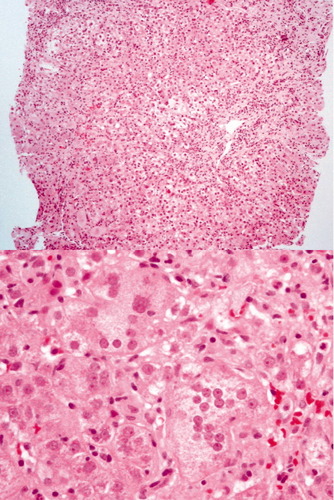
Conserved architectural structure with extensive areas of multinuclear giant cells, portal tract enlargement with bridging necrosis, inflammation, regenerative changes and mononuclear cells hyperplasia.
The cause of PGCH is unknown and probably multifactorial; possibilities include a virus,8, 9 drugs and herbal remedies,10 and autoimmune changes.11, 12 In addition, reports have been published about patients who have undergone liver transplantation.13, 14 Our patient received Pil-Food. Severe changes in liver function tests occurred, she was positive for antinuclear antibody autoreactivity, and a histological examination found abundant areas of multinucleate giant cells with marked periportal and parenchymal hepatocellular necrosis and inflammation. Because all the aforementioned alterations appeared during the long-term ingestion of Pil-Food [a composition developed by Synthelabo that contains D,L-methionine, L-(+)-cysteine hydrochloride, L-cysteine, enzymes and animal protein hydrolysates, millet extract, calcium pantothenate, vitamin B2 phosphate, vitamin B6, biotin (vitamin H), and vitamin E] and a successful corticosteroid response was attained, we speculate that this hepatic autoreactivity could be related to the Pil-Food treatment.15, 16 Moreover, just like patients with drug-induced AIH,1 our patient did not require long-term immunosuppressive therapy. We believe that this case highlights (1) that the breakdown of immune tolerance by drugs is able to trigger liver autoreactivity and (2) that some cases of PGCH may present a rapid and effective response to corticosteroid therapy instead of a fulminant or progressive course.
References
Ricardo Moreno-Otero M.D.* , Maria Trapero Marugán M.D.* , Luisa García-Buey M.D.* , Asunción García-Sancchez M.D. , * Digestive Diseases Service, Hospital Universitario de La Princesa, Universidad Autónoma de Madrid, Madrid, Spain, Pathology Service, Hospital Universitario de La Princesa, Universidad Autónoma de Madrid, Madrid, Spain, Centro de Investigación Biomédica en Red, Instituto de Salud Carlos III, Madrid, Spain.




