Choices of medical institutions and associated factors in older patients with multimorbidity in stabilization period in China: A study based on logistic regression and decision tree model
Abstract
Background
As China's population ages, its disease spectrum is changing, and the coexistence of multiple chronic diseases has become the norm with respect to the health status of its elderly population. However, the health institution choices of older patients with multimorbidity in stabilization period remains underresearched. This study investigate the factors influencing the choices of older patients with multimorbidity to provide references for the rational allocation of healthcare resources.
Methods
A multistage, stratified, whole-group random-sampling method was used to select eligible older patients from September to December of 2022 who attended the Community Health Service Center of Guangdong Province. We adopted a self-designed questionnaire to collect patients' general, disease-related, social-support information, their intention to choose a healthcare provider. A binary logistic regression and decision tree model based on the Chi-squared automatic interaction detector algorithm were implemented to analyze the associated factors involved.
Results
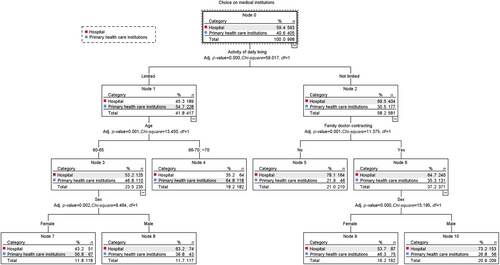
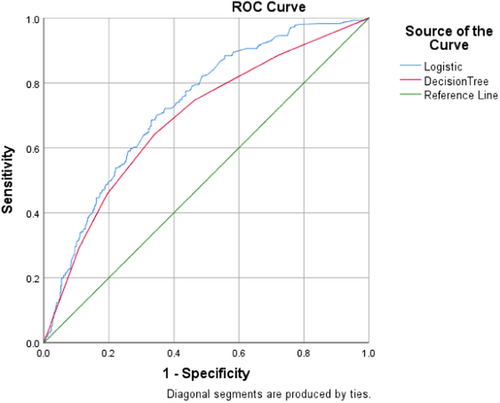
A total of 998 patients in stabilization period were included in the study, of which 593 (59.42%) chose hospital and 405 (40.58%) chose primary care. Our binary logistic regression results revealed that age, sex, individual average annual income, educational level, self-reported health status, activities of daily living, alcohol consumption, family doctor contracting, and family supervision of medication or exercise were the principal factors influencing the choice of medical institutions for older patients with multimorbidity (p < 0.05). The decision-tree model reflected three levels and 11 nodes, and we screened a total of four influencing factors: activities of daily living, age, a family doctor contract, and patient sex. The data showed that the logistic regression model possessed an accuracy of 72.9% and that the decision tree model exhibited an accuracy of 68.7%. Prediction using the binary logistic regression was thus statistically superior to the categorical decision-tree model based on the Chi-squared automatic interaction detector algorithm (Z = 3.238, p = 0.001).
Conclusion
More than half of older patients with multimorbidity in stabilization period chose hospitals for healthcare. Efforts should be made to improve the quality of healthcare services and increase the medical contracting rate and recognition of family doctors so as to attract older patients with multimorbidity to primary medical institutions.
Abbreviations
-
- AUC
-
- areas under the ROC curve
-
- CHAID
-
- Chi-squared automatic interaction detector
-
- ROC
-
- receiver operating characteristic
1 INTRODUCTION
Multiple morbidities or “multimorbidity” is defined as two or more coexisting chronic diseases in the same individual [1]. With China's proportion of aging individuals increasing, the coexistence of multiple chronic diseases has gradually become the norm for elderly Chinese, reducing the quality of life, adding to the financial burden on families and society, and placing enormous pressure on the healthcare system. Due to the irrational allocation of healthcare resources in China, large hospitals have occupied high-quality healthcare resources, while the lack of service capacity of primary healthcare institutions has led to an inverted triangle with respect to the supply of healthcare resources [2]—the exact opposite of the right-side-up triangle reflecting patient needs. Since its new healthcare reform, China has vigorously promoted hierarchical medical treatment, making chronic disease management a major component of health services in primary care. However, many patients with multimorbidity in China presently still choose tertiary hospitals for their direct medical treatment [2]. Patients travel to and from various medical specialties and medical institutions, leading to an increased risk of multiple-medication use and poor continuity of care.
By 2022, there were a total of 1812 hospitals in Guangdong Province, including 270 tertiary hospitals and 644 secondary hospitals/county hospitals. There were a total of 56,636 primary healthcare institutions, including 2729 community health service stations, 25,304 village health offices, and 1169 community health service centers/township health centers. In 2022, the total number of visits to medical institutions in the province reached 804 million, of which 378 million were in hospitals and 377 million were in primary care institutions. It revealed that hospitals were responsible for more than half of the health care services, different from the pattern of hierarchical medical treatment. Guangdong Province's hierarchical medical treatment policy required that by 2025, most counties (cities and districts) will have an in-county hospitalization rate of about 85% and an in-county primary care rate of more than 65%. If the majority of elderly people with multimorbidity go to hospitals for treatment, which will lead to serious shortcomings such as fragmentation and inefficiency in our healthcare delivery system. If primary healthcare institutions are better able to provide basic medical, preventive and rehabilitation services, residents will be able to obtain medical services at a lower cost and will naturally have better health. That is, patients with multiple morbidities in stabilization period should be treated at primary healthcare institutions with the requirement of hierarchical medical treatment. Therefore, it is essential to explore the factors influencing the choices of healthcare institution for older patients with multimorbidity in stabilization period and the ways to attract them to primary healthcare institutions.
There are currently few studies on the choices of medical institutions and their associated factors made by older patients with multiple morbidities in China. Chen et al. [3] explored the associated factors of residents' medical treatment behavior and put forward countermeasures and suggestions. Zhu et al. [4] explored the awareness and compliance of patients with multimorbidity with hierarchical medical treatment policy, the factors affecting whether they choose to go to community health service centers for first consultation. There is a lack on the study about factors influencing the choices of healthcare institution for older patients with multimorbidity in stabilization period. In this study, we investigated the factors influencing the choices of older patients with multimorbidity using both logistic regression and decision tree models to provide references for the further promotion of hierarchical medical treatment and the rational allocation of healthcare resources.
2 METHODS
2.1 Study design and data selection
A cross-sectional study was conducted between September and December of 2022 in Guangdong, China. Adopting the Guangdong Province Community Health Record Information System, we initially executed a multistage, stratified, whole-group random-sampling method to select three cities based on their economic level and geographical location, then randomly selected three districts in each city, and finally randomly selected three communities in each district for the survey. After obtaining informed consent from the subjects by paper, the survey respondents were screened according to our inclusion and exclusion criteria. Inclusion criteria were as follows: (1) having two or more chronic diseases simultaneously, (2) age ≥60 years, (3) provision of informed consent and willingness to participate in this study, and (4) ability to cooperate in completing the questionnaire. This survey was conducted offline by a team of trained hospital management postgraduates, general practice trainees, community general practitioners, and nurses; and questionnaires with missing items were removed. The data were evaluated by a reviewer, and after confirmation as correct, the data were entered in a two-person parallel entry process and assessed for consistency using EpiData 3.1 software. We have recruited 1100 patients, a final sample of 998 cases was thus included, the effective completion rate was 90.73%.
2.2 Measure of medical-treatment choices
A self-designed questionnaire based on the Chinese version of the 36-item Short Form Health Survey Questionnaire (SF-36) [5], the Chinese version of the Health-Promoting Lifestyles Profile (HPLP-C) [6], and the Morisky Medication Adherence Scale-8 (MMAS-8) [7] was used in this study. The questionnaire was revised and improved through a presurvey in the Nanshan District, Shenzhen, and the validity of the questionnaire was assessed through the Delphi expert-consultation method, leading to the final version of the questionnaire. The questionnaire principally included (1) general information—that is, age, sex, educational level, marital status, region of residence, type of residential address, and individual average annual income; (2) disease-related information—that is, level of disease understanding, self-reported health, activities of daily living, smoking status, and alcohol consumption; (3) social support—that is, a contractual relationship with a family doctor, family supervision of healthy behaviors, and social interactions; and (4) intention to choose and relevant factors involved in choosing medical institutions, including “What type of medical institutions do you usually go to?”. Hospitals included secondary hospitals/county hospitals and tertiary hospitals; while primary healthcare institutions included community health service stations/village health offices and community health service centers/township health centers.
2.3 Statistical analysis
Categorical variables were reported as ratios and percentages, and Chi-squared tests were executed to examine the differences between the two distinct medical-treatment option groups. The variables that were statistically significant in the Chi-squared test were comprised in logistic regression and decision-tree models so as to identify the correlations among the variables. The exhaustive Chi-squared automatic interaction detector (CHAID) growth method—with a maximal growth depth of 3—was used to obtain the optimal model. The CHAID growth method (referred to as the Chi-squared automatic-interaction detector) encompasses the Chi-squared test principle to optimally segment the data and automatically judges and groups multivariate contingency tables according to the p-value, and this can efficiently mine the primary influencing factors. We set the minimal sample sizes of the parent and child nodes to 200 and 100, respectively, and a 10-level cross-sectional model was subsequently exploited for validation. We used receiver operating characteristic (ROC) curves and the areas under the ROC curve (AUC) to compare the predictive abilities of logistic regression and decision-tree models and conducted statistical analysis using SPSS software (version 26), with a two-tailed p < 0.05 considered to be statistically significant.
3 RESULTS
3.1 Characteristics of participants
A total of 998 subjects were enrolled in the present study, and their baseline characteristics with regard to their different medical treatment choices are summarized in Table 1. With respect to the choices of medical institution, 593 (59.42%) participants chose a hospital setting and 405 (40.58%) subjects chose a primary care clinic. Among them, 366 (36.67%) patients chose to visit a secondary hospital/county hospital, 228 (22.85%) patients chose a tertiary hospital, 42 (4.21%) patients chose a community health clinic/village health office, and 362 (36.27%) patients chose a community health center/township health center. We found significant statistical differences between the two groups in the dimensions of age, sex, educational level, individual average annual income, level of disease understanding, self-reported health, activities of daily living, smoking status, alcohol consumption, establishment with a family doctor, and family supervision of healthy behaviors (p < 0.05).
| Characteristic | Total N (%) | Choices of medical institutions (N = 998) | p | |
|---|---|---|---|---|
| Hospital (n = 593) N (%) | Primary health care institutions (n = 405) N (%) | |||
| Age, year | 0.013 | |||
| 60–65 | 633 (63.43) | 398 (67.12) | 235 (58.02) | |
| 66–70 | 304 (30.46) | 161 (27.15) | 143 (35.31) | |
| >70 | 61 (6.11) | 34 (5.73) | 27 (6.67) | |
| Sex | 0.006 | |||
| Male | 518 (51.90) | 329 (55.48) | 189 (46.67) | |
| Female | 480 (48.10) | 264 (44.52) | 216 (53.33) | |
| Educational level | <0.001 | |||
| Middle school and blow | 220 (22.04) | 107 (18.04) | 113 (27.90) | |
| High school and above | 778 (77.96) | 486 (81.96) | 292 (72.10) | |
| Marital status | 0.519 | |||
| Married | 935 (93.69) | 558 (94.10) | 377 (93.09) | |
| Other | 63 (6.31) | 35 (5.90) | 28 (6.91) | |
| Residential regions | 0.122 | |||
| Urban | 821 (82.26) | 497 (83.81) | 324 (80.00) | |
| Rural | 177 (17.74) | 96 (16.19) | 81 (20.00) | |
| Type of residential address | 0.056 | |||
| Living alone | 57 (5.71) | 27 (4.55) | 30 (7.41) | |
| Not living alone | 941 (94.29) | 566 (95.45) | 375 (92.59) | |
| Individual average annual income | 0.036 | |||
| <50,000 yuan | 528 (52.91) | 330 (55.65) | 198 (48.89) | |
| ≥50,000 yuan | 470 (47.09) | 263 (44.35) | 207 (51.11) | |
| Medical insurance | 0.057 | |||
| Urban medical insurance | 664 (66.53) | 412 (69.48) | 252 (62.22) | |
| Medical insurance for urban and rural residents | 313 (31.36) | 170 (28.67) | 143 (35.31) | |
| Out of pocket | 21 (2.11) | 11 (1.85) | 10 (2.47) | |
| Level of disease understanding | <0.001 | |||
| Good | 838 (83.97) | 520 (87.69) | 318 (78.52) | |
| Poor | 160 (16.03) | 73 (12.31) | 87 (21.48) | |
| Self-reported health | <0.001 | |||
| Good | 373 (37.37) | 263 (44.35) | 110 (27.16) | |
| General | 489 (49.00) | 272 (45.87) | 217 (53.58) | |
| Poor | 136 (13.63) | 58 (9.78) | 78 (19.26) | |
| Activity of daily living | <0.001 | |||
| Not limited | 581 (58.22) | 404 (68.13) | 177 (43.70) | |
| Limited | 417 (41.78) | 189 (31.87) | 228 (56.30) | |
| Smoking status | 0.022 | |||
| Nonsmoker | 847 (84.87) | 516 (87.02) | 331 (81.73) | |
| Current or former smoker | 151 (15.13) | 77 (12.98) | 74 (18.27) | |
| Alcohol consumption | <0.001 | |||
| Nondrinker | 755 (75.65) | 473 (79.76) | 282 (69.63) | |
| Current or former drinker | 243 (24.35) | 120 (20.24) | 123 (30.37) | |
| Family doctor contracting | 0.001 | |||
| Yes | 644 (64.53) | 359 (60.54) | 285 (70.37) | |
| No | 354 (35.47) | 234 (39.46) | 120 (29.63) | |
| Family supervision of healthy behavior | <0.001 | |||
| Frequently | 763 (76.45) | 481 (81.11) | 282 (69.63) | |
| Occasionally | 206 (20.64) | 98 (16.53) | 108 (26.67) | |
| Never | 29 (2.91) | 14 (2.36) | 15 (3.70) | |
| Social interaction | 0.936 | |||
| Frequently | 854 (85.57) | 507 (85.50) | 347 (85.68) | |
| Hardly | 144 (14.43) | 86 (14.50) | 58 (14.32) | |
| Number of comorbidities | 0.325 | |||
| 2 | 345 (34.57) | 205 (34.57) | 140 (34.57) | |
| 3 | 455 (45.59) | 279 (47.05) | 176 (43.46) | |
| ≥4 | 198 (19.84) | 109 (18.38) | 89 (21.97) | |
| Years of suffering from chronic diseases | 0.287 | |||
| ≤5 years | 387 (38.78) | 238 (40.13) | 149 (36.79) | |
| >5 years | 611 (61.22) | 355 (59.87) | 256 (63.21) | |
3.2 Results of logistic regression analysis
A binary logistic regression was conducted with the choice of institution as the dependent variable (assigned values: 0 = hospital, 1 = primary healthcare institution). In order not to incorporate more confounding factors, we delete marital status, residential regions, type of residential address, medical insurance, social interaction, number of comorbidities and years of suffering from chronic diseases for futhur analysis, chose the statistically significant variables in the univariate analysis were designated as the independent variables (Table 2). The results of logistic regression analysis showed that age, sex, educational level, individual average annual income, self-reported health, activities of daily living, alcohol consumption, family doctor contracting, and family supervision of healthy behaviors were the factors that influenced the choice of medical institution (p < 0.05). Compared with choosing a hospital, age between 66 and 70 years (odds ratio [OR] = 1.503; 95% confidence interval [CI], 1.103–2.049), gender being female (OR = 2.022; 95% CI, 1.478–2.767), educational level below middle school (OR = 0.531; 95% CI, 0.370–0.763), individual average annual income ≥ 50,000 yuan (OR = 1.776; 95% CI, 1.308–2.412), poor self-reported health (OR = 1.791; 95% CI, 1.298–2.471; OR = 1.712, 95% CI, 1.076–2.724), limited activities of daily living (OR = 2.128; 95% CI, 1.572–2.880), current or former drinker (OR = 1.689; 95% CI, 1.176–2.425), family doctor contracting (OR = 0.582; 95% CI, 0.426–0.795), and occasional family supervision of healthy behaviors (OR = 1.807, 95% CI, 1.266–2.580) were the contributing factors for choosing a primary healthcare institution.
| Variables | OR | 95% CI | P |
|---|---|---|---|
| Age, years | |||
| 60–65 | |||
| 66–70 | 1.503 | (1.103, 2.049) | 0.010 |
| >70 | 1.234 | (0.691, 2.204) | 0.478 |
| Sex | |||
| Male | |||
| Female | 2.022 | (1.478, 2.767) | <0.001 |
| Educational level | |||
| Middle-school and below | |||
| High school and above | 0.531 | (0.370, 0.763) | 0.001 |
| Individual average annual income | |||
| <50,000 yuan | |||
| ≥50,000 yuan | 1.776 | (1.308, 2.412) | <0.001 |
| Level of disease understanding | |||
| Good | |||
| Poor | 1.098 | (0.731, 1.651) | 0.652 |
| Self-reported health | |||
| Good | |||
| Average | 1.791 | (1.298, 2.471) | <0.001 |
| Poor | 1.712 | (1.076, 2.724) | 0.023 |
| Activities of daily living | |||
| Not limited | |||
| Limited | 2.128 | (1.572, 2.880) | <0.001 |
| Smoking status | |||
| Nonsmoker | |||
| Current or former smoker | 1.240 | (0.787, 1.954) | 0.354 |
| Alcohol consumption | |||
| Nondrinker | |||
| Current or former drinker | 1.689 | (1.176, 2.425) | 0.005 |
| Family doctor contracting | |||
| Yes | |||
| No | 0.582 | (0.426, 0.795) | 0.001 |
| Family supervision of healthy behaviors | |||
| Frequently | |||
| Occasionally | 1.807 | (1.266, 2.580) | 0.001 |
| Never | 2.079 | (0.903, 4.787) | 0.085 |
- Abbreviations: CI, confidence interval; OR, odds ratio.
3.3 Results of the decision-tree model
The results of the decision-tree model based on the CHAID algorithm are shown in Figure 1. The decision-tree model incorporates three levels, 11 nodes, and six terminal nodes. Activities of daily living, age, the family-doctor relationship, and sex were the primary factors influencing the choice of healthcare institution for elderly multimorbid patients. The first level of the decision tree comprised the activities of daily living, indicating that the ability to perform daily-living activities reflected the highest correlation with the choice of healthcare institution. Patients with a restricted ability to perform daily living activities were more likely to choose a primary care institution (54.7%) than a hospital (45.3%), and patients with an unrestricted ability to perform daily living activities were more likely to choose a hospital for consultation (69.5%) than a primary care institution (30.5%). Among patients with a limited ability to perform the activities of daily living, those aged 65 years and over were more likely to choose primary care (64.8%) and those aged below 65 years were more likely to choose a hospital (53.2%). Among patients with a limited ability to perform the activities of daily living and who were under 65 years of age, 56.8% of women chose primary care—which was much higher than the proportion of men who chose primary care (36.8%). For elderly patients with multiple morbidities who did not exhibit a limited ability to perform their daily living activities, patients who had contracted with a family doctor were more likely to choose primary care (35.3%) than those who had not signed on with a family doctor (21.9%). For patients with unrestricted mobility and had signed up with a family doctor, women(53.7%) were less likely to choose hospital than men (73.2%).
3.4 Comparison of predictive results between models
According to the predicted probabilities obtained by the two models as test variables, ROC curves were constructed, as shown in Figure 2. The ROC curves for both models were a distance from the diagonal line, indicating that both models showed favorable predictive ability and similar classification effects. However, there were differences between the two models. The influencing factors in the logistic regression model—that is, educational level, individual average annual income, self-reported health, alcohol consumption, and family supervision of healthy behaviors—were eliminated in the decision tree model. The AUC for the binary logistic regression model was 0.729 (0.698–0.761), with a sensitivity of 70.1% and a specificity of 65.3%. The AUC for the decision tree model was 0.687 (0.653–0.721), with a sensitivity of 64.2% and a specificity of 65.9%. A comparison of the specific classification results of the two models is shown in Table 3. The sensitivity of the binary logistic regression model was the higher of the two models, while the specificity of the decision tree model based on the CHAID algorithm was greater than that of the former; and the overall predictive ability of the binary logistic regression was superior to that of the decision-tree model based on the CHAID algorithm (Z = 3.238, p = 0.001).
| Model | AUC | Sensitivity | Specificity | S.E. | p | 95% CI |
|---|---|---|---|---|---|---|
| Binary logistic regression model | 0.729 | 70.1% | 65.3% | 0.016 | <0.001 | 0.698–0.761 |
| Decision-tree model | 0.687 | 64.2% | 65.9% | 0.017 | <0.001 | 0.653–0.721 |
- Abbreviation: AUC, area under the curve.
4 DISCUSSION
In this study, we explore the factors influencing the choices of healthcare institution for older patients with multimorbidity in stabilization period and the ways to attract them to primary healthcare institutions. A total of 998 older subjects with multiple morbidities were included in this study, of which 405 (40.58%) chose primary care institutions for medical treatment. Although chronic disease treatment constitutes the principal service provided by primary healthcare institutions in China, the utilization rate of primary healthcare institutions by older patients sitll remains low, indicating a trend of individuals seeking higher level medical care, which caused the waste of healthcare resources. This suggests that further promotion of hierarchical medical treatment is needed. The primary factors that patients considered when choosing a medical institution included medical standards, medical conditions, medical costs, medical insurance reimbursement, and familiarity with healthcare options [8-10]. This to some extent explains why patients preferred hospitals for medical treatment. The majority of medical resources in China are currently concentrated in hospitals, while primary healthcare institutions have insufficient medical resources and lag behind in service quality, leading to a lack of trust in primary care institutions for patients and a tendency to choose hospitals when seeking treatment [11].
The decision tree model breaks the traditional linear processing method by eliminating the collinearity among variables and including a series of logical decisions. Also, it can visually display the interaction between independent variables and the importance of independent variables in the form of tree diagram, and graphically present the percentage of patients' medical treatment choices with various characteristics. The joint use of the decision tree and logistic regression models can complement each other and improve the analysis performance. The decision tree's topmost layer was the ability to perform the activities of daily living, indicating that it was the most significant influencing factor in the choice of healthcare institution. Patients with limited ability to perform the daily living activities tended to choose primary healthcare institutions for medical treatment, while those with unrestricted ability to perform daily living activities tended to choose hospitals. The reason for this may be the characteristics of hospitals, such as high patient volume and long waiting times, making it more inconvenient for patients with limited ability to perform their daily living activities to visit hospitals. In contrast, primary healthcare institutions typically have shorter waiting times, and patients who have an existing relationship with a family doctor can receive medical services at home, greatly facilitating the daily visits to patients with poor self-care abilities [12].
The second layer of the decision tree consisted of age and whether the patient had an existing relationship with a family doctor, indicating that both were important factors influencing a patient's choice of healthcare institutions. Our results thus showed that the older the patient with comorbidities, the more likely they tended to prefer primary healthcare institutions for medical treatment, consistent with the findings of many related studies [13, 14]. Patients in older age experience a decline in physical function, and as the number of illnesses increases, the frequency of various minor physical discomforts also increases, leading to an increased number of medical visits. Compared to the complex medical procedures characteristic of hospitals, primary healthcare institutions offer convenience in terms of medical consultations, and family doctors profess a relatively better understanding of a patient's condition. Most cases of minor physical discomfort can be addressed at the primary healthcare level, and, therefore, the older the patient with comorbidities, the more likely they prefer to choose primary healthcare institutions.
Whether a patient has an existing relationship with a family doctor also influences the choice of healthcare institution. Family doctors can provide comprehensive, effective, and continuous medical services, including long-term prescriptions for chronic diseases. For patients with multiple morbidities, seeking treatment at hospitals requires navigating between multiple departments, posing risks in taking multiple medications or in treatment discontinuation. In contradistinction, family doctors can provide a one-stop solution for the medical needs of patients with comorbidities, offering continuous and individualized treatment and health management plans [15]. Therefore, a higher proportion of patients who have an existing relationship with a family doctor choose primary healthcare institutions. However, it should be noted that among patients with no restrictions on their ability to perform daily activities (and even for those with an existing relationship with a family doctor), only 35.3% choose primary healthcare institutions for medical treatment, with the majority still choosing hospitals. This indicates that family doctors reflect insufficient appeal to elderly patients with comorbidities. The primary reason for this is the lack of comprehensive care that can be provided by most family doctors in China, resulting in a limited scope of medical services provided and leading to a lack of trust among patients toward family doctors [16].
Patient sex is also a factor that influences the choice of healthcare institutions. Among older patients with multiple chronic conditions, the proportion of women who choose primary healthcare institutions remains higher than the proportion of men who choose the same, consistent with previous studies [17]; and women may exhibit a greater awareness of their personal health and thus be more likely to notice when they experience a slight discomfort. Since such symptoms are relatively mild visiting primary healthcare institutions can provide a solution. Therefore, the proportion of women choosing primary healthcare institutions remains higher than the proportion of men choosing the same.
In contrast to the logistic regression model, the variables of educational level, individual average annual income, self-reported health, alcohol consumption, and family supervision of healthy behaviors were not included in the decision-tree model. The reason for this could be attributed to our limited sample size and the restrictions imposed by the number of samples at each node and the depth of the decision tree; the influence of these variables on healthcare choices may also only have been manifested at deeper levels of the decision tree. Additionally, it is possible that these variables exerted relatively weaker effects on healthcare choices compared to other variables, and during the data analysis process, these were pruned and excluded as confounding factors.
The utilization of family doctors is an important influencing factor for patients in choosing a primary healthcare institution for treatment. The rate of using family doctors in China has continuously increased in recent years [2], with patients with chronic diseases constituting the largest group. However, studies have shown that most patients only engage in the act of signing on with doctors, with only a very few actually utilizing them [18]. The results of this study indicate that the proportion of patients with multiple chronic conditions who choose to visit hospitals is still higher than the proportion of patients choosing primary healthcare institutions, indicating inadequate utilization of family doctors by patients with multiple chronic conditions [19]. Therefore, improving the utilization rate of family doctors is an important means to enhance patient trust and the clinical visit rate to primary healthcare institutions. Previous research has identified reasons for the low utilization of family doctors, including patients' lack of trust in doctors, lack of targeted services, and unclear referral systems [20]. Therefore, it is important to enhance the service capabilities of family doctors by rehiring retired doctors, formulating policies to attract family doctors, enhancing individualized treatment and guidance services for patients with multiple morbidities, and providing regular healthcare lectures to improve patients' trust in family doctors [21].
Primary healthcare institutions are characterized by simple medical procedures, short waiting times, and continuous treatment and are therefore becoming the preferred choice for older patients with limited ability to perform their daily living activities and for female patients [22]. Older patients with multiple chronic conditions often experience minor discomfort, and their chronic disease management requires regular medical visits and follow-ups. Therefore, primary healthcare institutions comprise the optimal source for the treatment and management of chronic and multiple diseases. There is presently a low level of awareness among the general population regarding hierarchical medical services and family doctors in China [23], and this results in a low utilization rate of primary healthcare institutions. Therefore, efforts should be made to promote hierarchical medical services and family doctors to raise awareness among older patients with multiple chronic conditions regarding the convenience, continuity, and individualized treatment provided by primary healthcare institutions, so as to attract them to medical care at these institutions [19].
This study has some limitations. First, the questionnaire that we used was self-designed. Although a presurvey and validity test that deployed the Delphi expert-consultation method, we haven't test the reliability and validity of the questionnaire, and the questionnaire still lacked comprehensive investigational information, some questions were evidently still not detailed enough; and this may have had an impact on the survey results. Second, the survey was conducted in Guangdong Province, which possesses a relatively developed economy and medical services but is hardly representative of the overall situation in China. Moreover, this was a cross-sectional investigation with a limited inference of causality, and therefore, the study results need to be verified by conducting a high-quality cohort study.
5 CONCLUSIONS
Primary healthcare institutions possess advantages such as strong continuity of care, lower medical costs, and convenient access. Activities of daily living, age, contractual relationships with a family doctor, and sex were the primary factors that influenced the healthcare choices of older patients with chronic and multiple diseases in stabilization period. Therefore, primary healthcare institutions should strive to improve the quality of medical services, accessibility to care, and continuity of care—as well as reflect a greater role in healthcare so as to attract more patients with multiple chronic conditions who seek medical care at the primary level.
AUTHOR CONTRIBUTIONS
Xiaoran Wang: Conceptualization (equal); data curation (lead); formal analysis (equal); investigation (supporting); methodology (equal); project administration (supporting); resources (supporting); software (lead); supervision (supporting); validation (equal); visualization (lead); writing—original draft (lead). Dan Zhang: Conceptualization (equal); data curation (supporting); formal analysis (equal); funding acquisition (lead); investigation (lead); methodology (equal); project administration (lead); resources (lead); software (supporting); supervision (lead); validation (equal); visualization (supporting); writing—original draft (supporting); writing—review and editing (lead).
ACKNOWLEDGMENTS
This work was supported by the National Natural Science Foundation of China (72004112).
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ETHICS STATEMENT
This article does not address any ethical concerns, as we did not study any human or animal subjects, nor did we collect any sensitive data.
INFORMED CONSENT
Informed consent was obtained from all patients before inclusion.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




