Value Evaluation for Urban Medical Groups in China: A Case From Dapeng New District in Shenzhen
ABSTRACT
Background
An urban medical group in Dapeng New District was established in 2017 with the objective of enhancing outcomes for common diseases and reinforcing primary care by integrating high-level hospitals with primary health services. This study aimed to evaluate the performance of the urban medical group using the triangular value chain framework.
Methods
The evaluation was conducted using the Donabedian model, focusing on three key dimensions: safety and quality, accessibility, and affordability. Longitudinal data were collected from 2016 to 2022 through government annual reports, the medical insurance bureau, and hospital information systems. Preprogram and postprogram outcome measurements were compared to assess differences and trends, providing a clear picture of the program's effectiveness.
Results
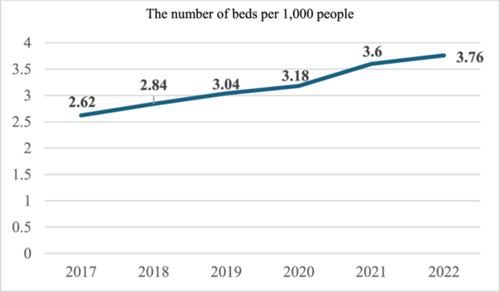
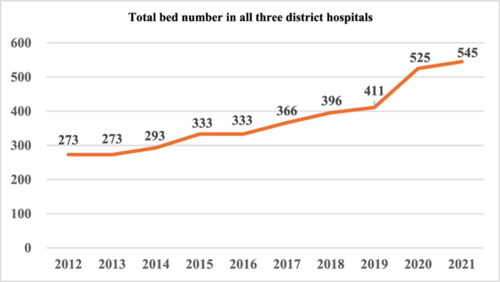
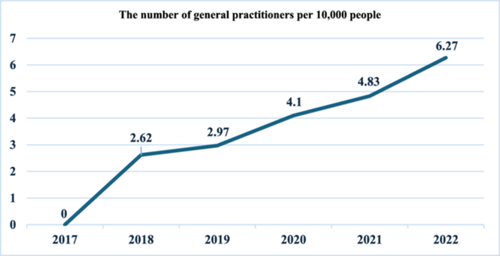
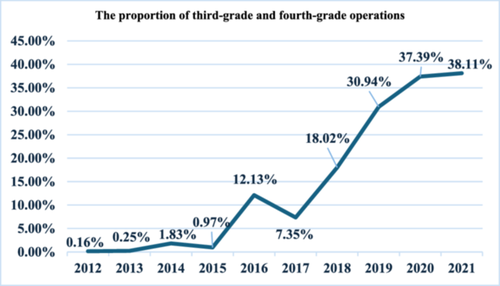
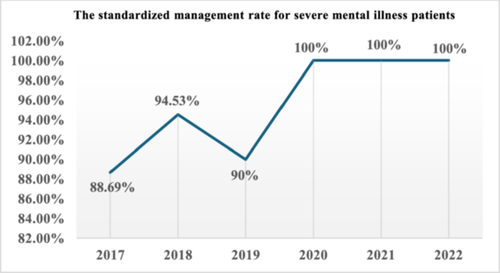
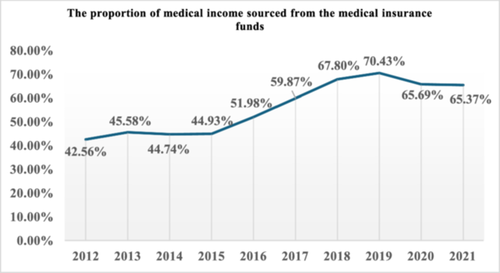
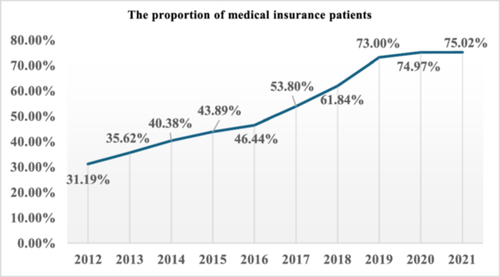
Accessibility improved significantly, with the number of hospital beds per 1000 residents increasing from 2.62 in 2017 to 3.76 in 2022. The availability of general practitioners (GPs) also rose markedly, from 0 per 10,000 residents in 2017 to 6.27 in 2022. Regarding safety and quality, the proportion of complex medical procedures conducted within the New District expanded substantially, from 7.35% in 2017 to 38.11% in 2021. Additionally, there was an enhancement in the standardized management rate of chronic diseases. Affordability assessments showed that the proportion of medical income derived from the medical insurance fund increased by nearly 22.81 percentage points between 2012 and 2021. By 2021, 75.02% of medical patients were covered by medical insurance, representing an increase of approximately 44 percentage points from 31.19% in 2012.
Conclusions
The implementation of the urban medical group in Dapeng New District has led to substantial improvements in healthcare accessibility, safety and quality, and affordability. Future initiatives will focus on advancing the “Dapeng Mode” to generate exemplary healthcare outcomes and minimize disparities in basic health services and health status between urban and rural populations. The reform agenda includes piloting payment reforms and innovative payment models within the Dapeng group, complemented by a health assessment and performance incentive system aimed at encouraging healthcare institutions to prioritize health management.
Abbreviations
-
- ICs
-
- integrated care services
-
- ICUs
-
- intensive care units
1 Background
To advance global health, the World Health Organization redefined primary care in the 1978 Declaration of Alma-Ata as fundamental healthcare services that meet over 80% of the population's medical needs [1], establishing the foundational “triple aims” or “triangular value chain” of healthcare: accessibility, safety, and affordability. Following this declaration, developed nations initiated efforts to enhance collaboration between healthcare providers and the public, while constructing high-quality, efficient healthcare systems. China's “Healthy China 2030” initiative has further emphasized that public health is a prerequisite for all future economic and social development [2].
China's healthcare reform has achieved notable successes, yet significant challenges remain in enhancing medical service accessibility, safety, and affordability. These challenges include the fragmentation of medical services and the suboptimal allocation and utilization of healthcare resources [3]. For example, a shortage of qualified healthcare providers at the grassroots level has led to increased unnecessary and avoidable hospitalizations [4]. Primary care centers often struggle with providing accurate initial diagnoses, as advanced medical equipment and high-tech instruments are predominantly available only in tertiary hospitals. Additionally, the referral system is imbalanced, with upward referrals being more accessible than downward referrals [5]. Simultaneously, China faces demographic pressures from an aging population and a continuous rise in chronic disease prevalence [6]. This demographic transition has driven an epidemiological shift from communicable to noncommunicable diseases, leading to three emerging social issues associated with early-stage aging [7]. First, many older people experience prolonged hospitalizations, including stays in intensive care units (ICUs). Second, frailty is often mismanaged as a disease, resulting in unnecessary treatments and hospitalizations. Third, there is a pressing need to address the specific healthcare needs of the elderly. Traditional health systems, which are accustomed to providing fragmented care for acute conditions, are not well-equipped to deliver the integrated, long-term, and proactive care required by elderly and chronically ill patients. Therefore, a restructured health system is needed to offer continuous, integrated services that encompass prevention, treatment, and rehabilitation to effectively manage chronic illnesses [8].
In response, China has adopted a top-down strategy to build integrated care services (ICs), promoting the development of medical consortia within healthcare organizations [9]. This approach aims to address the aforementioned needs of the elderly by enhancing primary care capacity, advancing a hierarchical medical system, and accelerating integrated care reforms. The medical consortium model facilitates the integration of healthcare resources, aligning with the principles of integrated care by establishing a cohesive entity responsible for both healthcare delivery and population health management. Composed of healthcare institutions at different levels, the consortium model seeks to optimize medical resource allocation and utilization. Consequently, the medical consortium has gained recognition as a critical strategy, continuously evolving in form and function [10]. Urban medical groups, a prominent type of medical consortium, are particularly advocated in cities, with leadership provided by tertiary public hospitals [11]. These groups aim to expand and decentralize high-quality healthcare services while encouraging patients to seek care at the appropriate levels through medical insurance payment reforms. Successful implementations have shown promise in managing minor ailments at primary health centers and severe conditions at hospitals, establishing a standardized referral system, and improving public access to healthcare [12]. Therefore, establishing a robust value evaluation system is imperative to facilitate the advancement of urban medical groups.
From 2018 to 2023, the central government implemented a series of assessment policies aimed at advancing the development of an integrated care system. These assessments encompassed multiple critical indicators, including policy implementation, management outcomes, technical quality, and quality of care, thereby establishing a robust foundation for the objective evaluation of healthcare integration [13-17]. The effectiveness of an urban medical group depends on the seamless integration of a robust primary care system with secondary and tertiary care through enhanced connectivity, data exchange, and information sharing among providers and between providers and patients. Establishing regional medical groups is fundamentally a mechanism for optimizing resource allocation. In the era of digital healthcare, the triple aims of healthcare—accessibility, safety, and affordability—have evolved to incorporate new dimensions. Accessibility now emphasizes that resource allocation should begin with the integration of community healthcare and family physicians to ensure the continuity of medical services. Safety is increasingly defined by quality management and safety control, leveraging intelligent monitoring, medical big data, and evidence-based medicine to guide the application of appropriate drugs and technologies. Affordability is addressed through strategies such as global budgeting, rational pricing, cost management, and third-party payment systems, ensuring broad acceptance of basic healthcare services [18]. A critical challenge, therefore, lies in evaluating urban medical groups using the triangular value chain framework. This study aims to identify management mechanisms that enhance medical resource allocation, facilitating urban medical groups in achieving the triple aims, with Dapeng New District in Shenzhen City serving as a case study.
Dapeng New District, located in eastern Shenzhen, historically exhibited medical standards below the city's average. Healthcare facilities in the district were in remote areas and offered lower quality of care compared with other districts. Notably, none of the three public hospitals—Kwai Chung People's Hospital, Dapeng New District Maternal and Child Health Hospital, and Nan'ao People's Hospital—attained tertiary status [19]. Furthermore, healthcare institutions in this district faced significant challenges in accessing medical resources and recruiting or retaining qualified medical staff. Before 2017, over 90% of residents spent 1–2 h traveling across districts to access high-quality medical care in other districts, contributing to substantial economic burdens for patients. Therefore, improving accessibility, safety, and affordability within this district emerged as a pressing need.
In contrast, the Shenzhen Second People's Hospital, located in the Futian District of Shenzhen, has established itself as a leading tertiary hospital over its 40-year history. It has the highest number of national and provincial key disciplines in Shenzhen. In 2019, the hospital ranked 52nd nationwide among tertiary public hospitals and fourth at the provincial level, underscoring its pivotal role within this urban medical group.
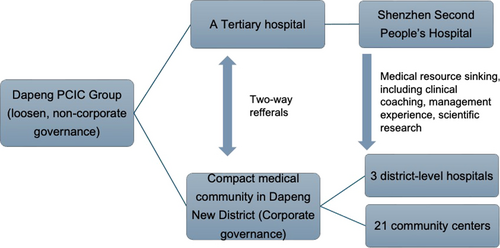
In June 2017, Dapeng New District integrated the Shenzhen Second People's Hospital into its healthcare system, forming an urban medical group that brought together three district-level public hospitals and 21 community health centers. This integration represents a “discipline alliance + compact medical community” model, characterized by a loosely structured, noncorporate governance consortium. The “discipline alliance” describes the collaborative relationship between the Shenzhen Second People's Hospital and healthcare institutions in Dapeng. As a tertiary hospital, it focuses on diagnosing and treating acute, critical, and complex diseases while also advancing medical disciplines, talent development, scientific research, and clinical education. The “compact medical community” comprises the three district hospitals and 21 community health centers and operates under a corporate governance model. This model centralizes control over human resources, finances, property, and management, fostering a unified approach to healthcare delivery. The institution aligns shared interests and responsibilities to enhance the health of regional residents, representing a defining feature of this cross-regional medical consortium (Figure 1).
After 6 years of operation, this model offers an opportunity to assess interim outcomes. As outlined above, this approach could reveal management mechanisms that optimize medical resource allocation, supporting urban medical groups in achieving the triple aims. Ultimately, this model holds potential for broader national implementation.
2 Methods
2.1 General Goal and Specific Objectives to Be Achieved
This study aimed to evaluate the value of an urban medical group in Dapeng New District, Shenzhen City, China, from 2017 to 2022. Accessibility of care was assessed using indicators such as the number of general practitioners (GPs) per 10,000 people and the number of beds per 1000 people. Quality and safety were evaluated through metrics related to the proportion of complex surgeries and the standard management rate of chronic diseases. Affordability was assessed by analyzing the proportion of medical income derived from the medical insurance fund and the proportion of medical insurance patients.
2.2 Logic Model of the Improvement Project
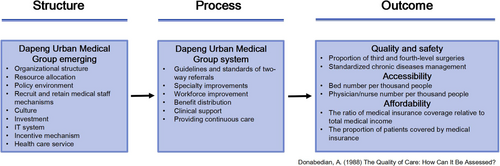
Donabedian's “structure–process–outcome” analysis model, widely recognized for its operational feasibility and effectiveness, was employed to evaluate healthcare system performance [20]. The “structure” component encompasses the medical service environment, including organizational structure and resource allocation. The “process” dimension evaluates the application of structural attributes in practice, focusing on medical service delivery. The “outcome” represents the performance resulting from the process, serving as a critical measure for assessing health service improvements. Structure underpins the process, with process development and enhancement following structural establishment. An effective process contributes to improved outcomes, enabling a comprehensive evaluation of medical service performance through an integrated assessment of structure, process, and outcome. In this study, “structure” referred to the establishment and organizational structure of the medical group, whereas “process” encompassed operational activities, such as two-way referrals. Enhancements in structure and process were anticipated to improve the quality of care and efficiency.
The Donabedian model also provided a robust framework for evaluating integrated medical services, offering a structured approach to measuring organizational structure, service processes, and outcomes at multiple levels. Medical consortia can leverage this model to establish a comprehensive and effective evaluation system for integrated medical services [21]. The evaluation focused on three core aspects: quality and safety, accessibility, and affordability (Figure 2).
2.3 Unit of Analysis and Data Source
This study employed a case study design to assess the effects of performance improvement within an urban medical group consisting of 25 medical institutions, considered as a single setting for the analysis. In evaluation research, the unit of analysis can vary across different levels, such as individual or community health conditions [22]. In this study, the organizational level was selected as the unit of analysis, as the primary objective was to evaluate performance improvement across health institutions. A mixed-methods approach was utilized, incorporating both qualitative and quantitative methodologies. Data collection and evaluation methods were guided by the Comprehensive Performance Evaluation Plan for Medical Consortium and aligned with relevant government policies [13-15]. The sample size was considered adequate, with longitudinal data collected from 2017 to 2022 in Dapeng New District, including some data spanning over a decade.
Secondary data sources were used in this evaluation. These sources included interviews, questionnaires, records, and official government documents. Qualitative data were obtained through interviews and administrative records, such as policy documents and narrative reports. The interviewees comprised 32 individuals, including top and middle managers, presidents, institutional directors, and family physicians from community health centers. This qualitative approach provided insights into implementation realities at the grassroots level and helped identify both organizational achievements and challenges. Consequently, the qualitative approach data contributed to a deeper understanding of organizational structure and processes, offering valuable insights into how and why the medical group achieved its study objectives [23].
Quantitative data for the outcomes section were sourced from government annual reports, medical insurance bureau records, and hospital information systems. Evaluating effectiveness was facilitated by analyzing temporal trends, with data collected longitudinally from 2017 to 2022. Comparisons of preprogram and postprogram outcomes were conducted to identify differences and trends, primarily visualized through charts.
2.4 Measurement of Variables and Analysis
All indicators (Table 1) were derived from established government policy documents and internationally recognized healthcare management criteria [13-18, 22]. Six specific indicators were selected from the 2020 government evaluation standards, tailored to align with Dapeng's contextual needs [15].
| Outcome | Indicators |
|---|---|
| Accessibility | The number of beds per 1000 people |
| The number of general practitioners per 10,000 people | |
| Quality and safety | The standardized management rate of severe mental illnesses |
| The proportion of third- and fourth-grade surgeries in hospitals | |
| Affordability | The proportion of medical income sourced from the medical insurance funds |
| The proportion of medical insurance patients |
The absence of a control group in this evaluation study posed challenges in accurately determining the intervention's effects. A critical aspect of the analysis involved selecting an appropriate referent or benchmark for comparison. Collecting data relative to the benchmark is crucial for assessing performance as inferior, superior, or consistent with the benchmark's standard [24]. In scenarios lacking a control group and where external organizational indicators or official standards are unavailable, before-and-after time-series designs are a widely accepted methodological choice [25]. This design enabled the evaluation of the organization's performance by comparing historical data on identical indicators [24]. Therefore, the historical performance of the study group served as the primary referent for this research. This longitudinal approach allowed for direct comparisons of identical indicators over time. The use of structure and process descriptions further facilitated the interpretation of performance trends through the before-after method. By analyzing differences in structure, process, and outcome, the study generated valuable insights and conclusions that informed subsequent reporting and recommendations [24]. Microsoft Excel was utilized to visualize trends through matrices, figures, and graphics.
3 Results
3.1 Accessibility
The availability of hospital beds per 1000 population improved significantly, increasing from 2.62 in 2017 to 3.76 in 2022 (Chart 1). The number of beds is a key metric for evaluating healthcare accessibility, as a higher bed capacity generally reflects enhanced hospital readiness to provide medical services. Over the past decade, the total bed count across the three district hospitals demonstrated a sustained upward trajectory, particularly following the establishment of the Dapeng Medical Group in 2017. This establishment marked a period of accelerated growth in bed availability compared with the previous 5 years, reaching 545 beds by 2021—representing a remarkable 99.63% increase since 2012 (Chart 2).
The density of GPs per 10,000 population rose from 0 in 2017 to 6.27 in 2022 (Chart 3). The number of GPs is a crucial indicator for assessing the availability of primary care within a specific region. For example, the Maternal and Child Health Hospital in Dapeng District, which focuses on medical treatments and preventive healthcare for women and children, demonstrated a notable shift. Before the formation of the Dapeng Medical Group, only two GPs were recorded in 2015, with no other GPs available in prior years. However, the period between 2018 and 2022 marked a significant breakthrough in primary care capacity, as the number of GPs increased from zero despite initially limited availability.
3.2 Safety and Quality
The three district hospitals in Dapeng are all classified as second-level facilities, inherently limiting the scope and complexity of procedures they can perform. Following the formation of the hospital group, experts from the leading hospital were deployed to these hospitals to perform high-level surgeries. An analysis of the proportion of third- and fourth-grade surgeries conducted in the New District demonstrates a significant increase, from 7.35% in 2017 to 38.11% in 2021 (Chart 4). Before 2016, this proportion remained relatively low. However, a marked rise occurred after 2017, underscoring the considerable improvement in healthcare quality and accessibility attributed to the introduction of advanced surgical equipment and enhanced medical expertise. This development has led to a significant elevation in the medical capacity of the group, enabling it to meet the treatment demands for third- and fourth-level surgeries.
The management of chronic diseases has also shown promising outcomes. For instance, in mental health management, the standardized management rate of patients with severe mental illness, based on clinical guidelines, improved from 88% in 2017 to 100% in both 2021 and 2022 (Chart 5).
3.3 Affordability
The proportion of medical income derived from medical insurance funds has demonstrated a marked upward trend, with a notable increase of 22.81 percentage points in 2021 compared with 2012 (Chart 6).
Since the establishment of the Dapeng group, concerted efforts have been made to explore and optimize the role of medical insurance payment mechanisms within the group. Consequently, the proportion of medical insurance patients has shown a substantial increase (Chart 7). By 2021, medical insurance patients accounted for 75.02% of the total, representing a significant rise of approximately 44 percentage points from 31.19% in 2012.
4 Discussion
The Donabedian model's outcome domain evaluates the effects of structure and process on healthcare delivery [20]. The results presented above demonstrate improvements in accessibility, safety, and affordability. To further elucidate the underlying mechanisms, examining the structural and process-related elements within the urban medical group provides insights into the “how” and “why” of these advancements [25].
First, the medical group functioned as a loosely structured, noncorporate governance consortium, organized under a “municipal tertiary hospital + (district hospitals + community health institutions)” model. This framework was unified by management, technology, and talent integration. The “district hospitals + community health institutions” component established a compact medical community characterized by uniform management of staff, finances, and resources. A Hospital Management Committee was established, accompanied by a formalized charter, whereas institutional affiliations, personnel identities, asset ownership, and policies—including financial inputs—remained consistent across the three district hospitals and associated community health centers.
Second, clear delineation of institutional roles contributed to efficient operations. As the leading entity, Shenzhen Second Hospital focused on the diagnosis and treatment of acute and critical conditions and complex diseases, alongside responsibilities in discipline development, talent training, scientific research, and clinical teaching. The three public hospitals in Dapeng adopted differentiated development strategies, emphasizing common disease management, integration of general practice with specialties, and fostering continuity of care between the municipal hospital and community health institutions. Community health service institutions served as “gatekeepers” of resident health, delivering primary medical care, public health services, and comprehensive health management.
Third, at the primary level, the group implemented an extensive departmental management system comprising seven internal departments: Comprehensive Management, Resource Management, Operation Management, Logistics Support, Community Health Service Management Center, Financial Management Center, and Information Management Center. This structure operated within the “Twelve Integration” operational framework (Figure 3), which promoted equitable medical resource allocation and enhanced recruitment and retention of healthcare professionals within the New District. The organizational structure not only provided a solid foundation for effective operations but also played a critical role in decentralizing medical resources, facilitating bidirectional referrals, promoting specialist clinical practice, and supporting mentorship programs, all of which contributed to improved accessibility and quality of care within the district.

Following the establishment of the group, 64 experts were permanently assigned to each district hospital and community health center. In 2021 alone, 1855 experts were dispatched, demonstrating the system's effectiveness. The increasing proportion of complex surgeries highlighted the residents’ growing recognition of high-quality medical resources within the district. Additionally, more patients with severe conditions opted for treatment within this integrated system, significantly reducing patient outflow. The group also made notable advancements in chronic disease management by prioritizing the development of general practice at the grassroots level, thereby enhancing the accessibility and quality of primary care services. It established the city's first community center dedicated to mental health service management, forming a specialized mental health team that adopted a “professional service + family management” home-based rehabilitation model. This model incorporated a tiered management system for mentally ill patients and a chronic disease case management system. For severely mentally ill patients, the three-tiered linkage and bidirectional referral system were fully utilized, contributing to a 100% standardized management rate for severe mental illness patients for three consecutive years.
To further improve healthcare affordability, the group increased subsidies for essential medical care, public health initiatives, family doctor contract signing, family bed establishment, and family doctor visits. The removal of the medical insurance cap for community health centers, along with the pricing advantages granted to these centers, strengthened financial sustainability. Additionally, the government increased the proportion of health insurance coverage and expanded the scope of free medication availability. These measures enabled patients to access treatment for serious illnesses within the district while reducing their out-of-pocket expenses.
This study has several limitations. First, a formal mechanism for interest sharing within the group has not yet been established. Second, practical challenges related to bed availability and the geographic distance of the leading hospital may hinder the smooth operation of many referral processes. Finally, the absence of a control group in this evaluation limits the ability to robustly assess its effects, as comparisons can only be made against historical performance. While the Dapeng urban medical group appears to effectively meet three key needs, it remains unclear whether this outcome is unique to this district. For example, the Luohu District has also been recognized as a successful urban medical group, albeit with different management mechanisms [26]. Evaluating the Dapeng model against alternative benchmarks may not provide effective standards [24].
5 Conclusions
The Dapeng urban medical group represents a loosely structured, noncorporate governance consortium exemplifying the “discipline alliance + compact medical community” model. This framework has enabled the establishment of a preliminary hierarchical medical system, characterized by the principle: “minor ailments are managed within communities; emergencies are addressed within Dapeng; and serious conditions do not leave the group.” The findings from this evaluation, based on the triangular value chain, provide valuable insights into the group's impact on accessibility, safety, quality, and affordability of healthcare in Dapeng New District.
The accessibility of basic healthcare services in Dapeng New District has significantly improved. The number of beds in the group's medical institutions increased by 99.63% compared with 2012, demonstrating substantial expansion in healthcare capacity. The growth in medical personnel has been equally notable, with the number of GPs per 10,000 people rising from 0 in 2017 to 6.27 in 2022. Although the COVID-19 pandemic led to temporary increases in bed capacity, these figures were not included in these data, ensuring the accuracy of long-term trends.
Safety and quality of healthcare services have been effectively maintained. There has been a continuous enhancement of specialized medical services and a substantial increase in primary healthcare capacity. Initial success in managing chronic diseases at the grassroots level is evidenced by a 100% standardized management rate for serious mental illnesses in 2020. The active involvement of experts from the leading hospital in advanced procedures within the New District has improved healthcare accessibility, with a positive trend in the performance of complex surgeries indicating strengthened safety and service quality.
Affordability of healthcare services has also improved in the New District. The proportion of medical income derived from medical insurance funds has increased, alongside a higher proportion of medical insurance patients, effectively reducing the financial burden on patients. From 2019 to 2023, outpatient visits decreased by an average of 1.24% annually, and inpatient visits declined by 0.19%. In 2023, the inpatient rate was 8.06% per 1000 population, significantly lower than the national average of 21.4%. The average cost per hospitalization within the group was 5345.64 yuan, well below the national average of 10,315.80 yuan. The basic medical insurance fund covered approximately 84% of outpatient and 86% of inpatient medical expenses, with individual burden rates of 16% and 14%, respectively. These outcomes reflect effective management of the economic burden on medical institutions and individuals.
Future initiatives aim to further enhance the Dapeng urban medical group's impact. The first step involves promoting the group as a model of exemplary outcomes, offering a practical institutional design that could serve as a valuable reference for regions with medical resource allocation imbalances. The “discipline alliance + compact medical community” model offers a national-level tertiary public hospital a pathway to support grassroots development, addressing disparities in health service levels between urban and rural populations. Second, a pilot program for payment reform and innovation will be introduced within the group to explore suitable payment models for primary care and chronic diseases. Integrating a capita-weighted budget with a global budget, supported by a health assessment and performance incentive system, will encourage medical institutions to strengthen health management. This approach is expected to enhance chronic disease management, optimize the use of medical insurance funds, and curb the excessive growth of medical expenses [27].
Author Contributions
Yan Cui: conceptualization (equal), data curation (equal), formal analysis (equal), methodology (lead), writing – original draft (lead), writing – review and editing (equal). Leiyu Shi: conceptualization (equal), methodology (equal), writing – review and editing (supporting). Shilan Tang: data curation (equal), writing – original draft (supporting). Yansui Yang: conceptualization (lead), formal analysis (equal), methodology (lead), writing – review and editing (supporting). Lijie Ren: data curation (equal), methodology (equal), writing – review and editing (equal).
Acknowledgments
The authors have nothing to report.
Ethics Statement
The authors have nothing to report.
Consent
The authors have nothing to report.
Conflicts of Interest
Prof. Leiyu Shi and Prof. Yansui Yang are Health Care Science Editorial Board members. To minimize bias, they are excluded from all editorial decision-making related to the acceptance of this article for publication. The remaining authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.




