Status of epilepsy in the tropics: An overlooked perspective
Jiaqi Liu, Peng Zhang, Qin Zou authors contributed equally to this work.
Abstract
Epilepsy is one of the most common serious chronic neurological diseases affecting people of all ages globally. It is characterized by recurrent seizures. About 50 million people worldwide have epilepsy. Indubitably, people with epilepsy (PWE) may be without access to appropriate treatment. Many studies have examined the molecular mechanisms and clinical aspects of epilepsy; nonetheless, the treatment gap exists in some special areas. In the tropics, the specific geographical and ecological conditions and a lack of medical resources result in neglect or delay of diagnosis for PWE. Herein, we summarized the epidemiology of epilepsy in the tropics and discussed the disease burden and existing problems, aiming to offer a medical environment for patients in need and highlight the importance of reducing the epileptic disease burden in tropical countries.
Key Points
- Epilepsy has been one of the major public health problems worldwide, but PWE in tropical areas is ignored invariably.
- The incidence and prevalence of epilepsy are high in tropical regions, while all-sided data are still lacking, especially in Oceania.
- Multifaceted factors lead to a large treatment gap in tropical areas. Simultaneously, comorbidity and stigma accompanied by epilepsy should be taken seriously.
- The status quo of epilepsy in tropical areas can be improved by multi-party cooperation to provide medical resources, an environment for PWE, and a quality of life.
1 INTRODUCTION
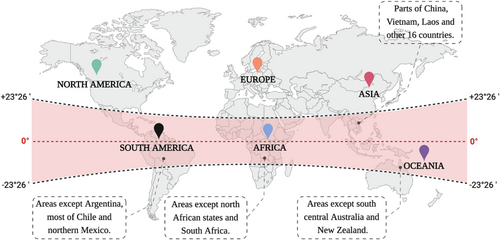
The tropics, a zone between the Tropic of Cancer and the Tropic of Capricorn, lies on both sides of the equator between 23°26′ north and south latitude. Globally, this area includes most of Asia (parts of China, Vietnam, Laos, and other 16 countries), Oceania (south-central Australia and New Zealand), Africa (north African countries and South Africa), and Latin America (Argentina, most of Chile, and northern Mexico), accounting for 39.8% of the global territory (Figure 1). Currently, no obvious temperature variations were detected in this area, which was characterized by a seasonless state accompanied by scorching weather all year round. Despite its abundant ecological resources and biodiversity, the high humidity and sunshine throughout the year increase the range and prolong the cycle of mosquito vectors. Moreover, the social-economic status of this area was low. However, only a few studies have focused on epilepsy pathogens in the tropics. The lack of medical resources and policy support is largely responsible for the fact that the people with epilepsy (PWE) in this area did not receive any necessary medical treatments. Hence, neglecting the unique pathogenic environmental factor in the tropics can lead to health disparities between this and other areas.
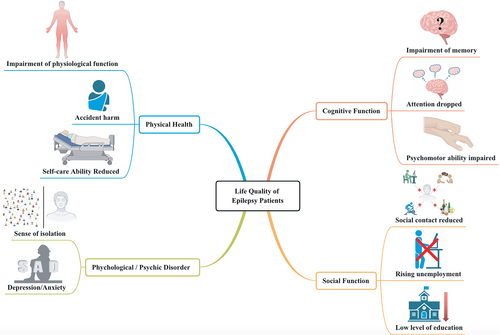
Among the chronic diseases that can significantly impact patients' everyday life, epilepsy is a nervous system disease caused by sudden abnormal firing of neurons, resulting in temporary brain dysfunction. The disease is characterized by repeated attacks and complex clinical manifestations. According to the latest ILAE classification of the epilepsies in 2017, epilepsy seizures can be classified into “focal onset,” “generalized onset,” and “unknown onset.” The primary presenting symptoms can manifest as individual or combined clinical signs, including “consciousness disorder,” “myoclonus”, “absence,” and “other motor-related disorders.”1, 2 Remarkably, the number of patients accompanied by varying psychological disorders has increased substantially over recent years. Previous studies have shown that cognitive dysfunction, anxiety, and depression are common comorbidities among patients with epilepsy, with prevalence rates much higher than in healthy people (30%-40%, 20%-40%, and 20%-60%, respectively).3, 4 Furthermore, different aspects of quality of life (QoL), including physical health, cognitive function, psychological or psychic disorder, and social function, can also be reduced due to this condition (Figure 2). Although this disease is harmful to patients' physical and mental health, it could affect their normal life significantly. Since the prevalence and incidence rate of epilepsy is high in low- and middle-income countries and patients with epilepsy in these countries are reluctant to seek treatment, a heavy disease burden in this area is a logical occurrence.
Currently, there are several studies on PWE. Researchers have taken different approaches, such as focusing on patients with different cultural and family backgrounds,5-7 different ages,8-13 region-specific,14-22 and inter-environmental.23-25 Some studies have focused on the treatment gap,26-30 special etiology,31-36 and disease burden37-40 in the tropics, aiming to formulate appropriate policies41-44 for PWE.
Most of these studies have focused on sub-Saharan Africa (SSA). Together, relevant data for some tropical countries are missing, and there is missing comprehensive evidence for the status of epilepsy in the tropics. Therefore, in this article, we reviewed the status quo of epilepsy in the tropics from an epidemiological aspect, disease status, and burden, and identified the risk factors, challenges, and interventions to offer an improved medical environment for patients in need and provide valuable ideas for reducing the burden of epilepsy at the global level.
2 ABOUT TROPICAL EPILEPSY
The incidence and prevalence of epilepsy in the majority of tropical countries or regions are persistent at a high level (Table 1).
| Continent | Country/province | Year | Incidence rate (cases/100000·year) | Prevalence rate(‰) | References |
|---|---|---|---|---|---|
| Global | — | 2019 | 61.44 | 7.6 | WHO.45 |
| Africa | Burkina Faso | 2015 | 123 | 12.46 | Fawi G, et al.46 |
| Tanzania | 2009 | 81 | 11.20 | Winkler, et al.47 | |
| Ethiopia | 1997 | 64 | — | Tekle-Haimanot, et al.48 | |
| 2021 | — | 5.20 | Yazie TS, et al.49 | ||
| Benin | 2013 | 69 | 12.70 | Houinato, et al.50 | |
| Kenya | 2015 | 46 | — | Kariuki, et al.51 | |
| Zambia | 2004 | — | 13.20 | Birbeck, et al.52 | |
| Nigeria | 2015 | — | 4.30 | Nwani, et al.53 | |
| Rwanda | 2005 | — | 49.00 | Dedeken P, et al.54 | |
| Asia | India | 2002 | 38-49 | 5.00 | Ray BK, et al.55 |
| Hong Kong, China | 2003 | — | 1.50 | Fong GC, et al.56 | |
|
Taiwan, China |
2007 2015 |
72 54 |
6.94 6.86 |
Chou IJ, et al.57 | |
| Hainan, China | 2021 | 24 | 3.06 | Zheng GX, et al.16 | |
| Yunnan, China | 2008 | 18.9 | 1.51 | Yu Z, et al.58 | |
| 2017 | — | 2.10-7.30 | Yu Z, et al.59 | ||
| Guangdong, China | 1985 | 49.04 | — | Yang LC, et al60 | |
| Singapore | 1997 | — | 5.00 | Loh NK, et al.61 | |
| Laos | 2006 | — | 7.70 | Tran DS, et al.62 | |
| Thailand | 2002 | — | 7.20 | Asawavichienjinda T, et al.63 | |
| Latin America | Chile | 1988 | — | 17.70 | Hun C, et al.64 |
| 1992 | 113 | — | Lavados J, et al.65 | ||
| Ecuador | 1992 | 122-190 | — | Placencia M, et al.66 | |
| Martinique | 1995 | 87-102 | — | Carpio A, et al.67 | |
| 1999 | 78 | — | Jallon P, et al.68 | ||
| Honduras | 2003 | — | 5.41 | Medina MT, et al.69 | |
| 2005 | 93 | — | Medina MT, et al.70 | ||
| Panama | 1986 | 22 | — | Gracia, et al.71 | |
Compared to other tropical areas, Asian countries show a lower rate of prevalence and incidence. China has the largest population in Asia. Take Hainan as an example; the prevalence and incidence of epilepsy in rural areas are lower than that in other tropical areas of the world.16 Interestingly, an epidemiological survey of epilepsy in rural areas and ethnic minority areas in China showed a variable prevalence rate among different ethnic groups. Among them, the Bai nationality (living in Yunnan province) has a higher average prevalence rate than the Han nationality, while the Li nationality (living in Hainan Province) has a lower prevalence rate than the Han type.60 This finding suggested that additional factors could be worth exploring the influence of variation in the epidemiological data for epilepsy.
2.1 Epidemiology
According to the 2015 Global Burden of Disease (GBD) study, epilepsy accounted for 0.5% of all disability-adjusted life years (DALY) and 5.0% of neurological diseases DALY. On June 20, 2019, World Health Organization (WHO) Fact Sheet reported that epilepsy accounted for 0.6% of the global disease burden. A previous study assessed the burden of epilepsy in 195 countries and territories between 1990 and 2016 and showed the dissimilarity in age-standardized disability-adjusted annual rates between countries in the lower and higher sociodemographic index (SDI) quintiles. These differences were attributed to high levels of epilepsy in about one-third of the cases in low-income countries.72 More than 50 million people worldwide have epilepsy, and the number continues to increase at a rate of 2.4 million annually.73 Approximately 80% of these patients live in low-or middle-income countries, and 75% did not receive timely treatment. However, the low economic level of most tropical countries is poorly reflected in the medical conditions of these regions. Due to the social conditions attributed to these economic disadvantages that affect education, science, and technology, PWE lacks an understanding of the disease and medical concepts, such as early detection, diagnosis, and treatment. Moreover, due to the lack of medical resources in many tropical countries or regions, there is also a lack of medical facilities. In addition, the psychological problems accompanying PWE are rarely given any attention, resulting in a higher incidence of epilepsy in these areas than in other parts, and most PWEs fail to receive the deserved attention.
2.2 Disease status and burden
According to the available statistics, >85% of the global burden of epilepsy affects 49% of the population living in low- and middle-income countries.74 The incidence and mortality rates of epilepsy are significantly high in these countries,75 suggesting that economic levels influence the burden of epilepsy. However, as the economic level of most of the tropical countries is low, there is a shortage of medical resources with a lack of education and understanding and arrested development of the social and cultural environment, which negatively affects the prevention of epilepsy in tropical areas and the diagnosis and treatment of PWE. Eventually, this increases the burden of epilepsy in these countries and regions, causing a substantial decline in the quality of life of PWE. Therefore, this global health problem should not be ignored.
In Africa, about 10 million people are directly affected by epilepsy, accounting for 20% of PWE worldwide.76 Previous studies have shown that the incidence of epilepsy in tropical SSA is 63–158/100000 people/year, and about 80% of these patients do not receive the required treatment. Concurrently, the rate of injuries due to uncontrolled seizures is extremely high, especially burns and fatal injuries, which are six times higher in this area than in the normal control group.77
In Latin America, about 5 million people have epilepsy, of which 3 million do not receive appropriate treatment.78 The disease burden of epilepsy in Latin America is approximately 14 460 845 DALYs (95% CI: 2.3–0.8 × 106), with years lived with disability (YLDs) as the major component. Mexico, Brazil, and Colombia have the highest rates of epilepsy, with alcohol abuse as the main risk factor.37 Thus, epilepsy remains a major cause of disability in Latin America.
In Cambodia, about 86 000 people suffer from epilepsy. Unlike in Africa, people in Cambodia do not share any religious beliefs that would oppose the treatment, and hence there is almost no obstacle to diagnosing and treating epilepsy in terms of ideology. Moreover, the social environment in Cambodia is more welcoming to PWE than in Africa. As a result, most Cambodians with epilepsy receive good social support and are not discriminated against or treated differently because of their condition.79 In addition, differences are observed in the treatment gap of epilepsy across several countries in Asia, including China (63%), India (50%-70%), Nepal (>70%), Pakistan (urban area > 72%, rural area 98%), and Turkey (70%).80
Approximately 30 million people have epilepsy in the Asia-Oceania region, comprising a large proportion from the tropics,81 that is, tropical Oceania has a high number of epilepsy patients. However, studies on PWE in tropical Oceania are scarce, unlike in Africa. Therefore, future studies should focus on these areas to fill the gap in epilepsy diagnosis and treatment status quo in tropical Oceanian countries. We will also focus on the new results in this research area in the future.
In conclusion, the heavy burden of epilepsy varies globally and across tropical areas, which is related to the economic, cultural, and medical level of each region and country. The currently available data illustrated the relevance of epilepsy to the QoL and lifespan of the people in tropical countries, reflecting the negative impact of epilepsy and suggesting that more attention should be focused on the countries with a high burden of epilepsy.
2.3 Risk factors
Available data have shown that the incidence of epilepsy is two to three times higher in tropical regions than in non-tropical industrialized countries.82 The determination of the etiology of epilepsy is rather challenging. Due to their specific geographical location, climate environment, social environment, population distribution, and religious belief status, the determination of the etiology of epilepsy in tropical areas is complex and likely to include unidentified factors. Herein, we classified the etiology of epilepsy patients in tropical regions and summarized it as follows to provide a relevant reference for clinicians and researchers.
2.3.1 Infectious agent
Due to the complex natural environment of tropical areas, viral infection is the most common cause of epileptic seizures. The causative viruses include malaria, HIV, cysticercosis, Zika virus, tuberculosis, Japanese encephalitis, West Nile virus, dengue fever, Nipah virus, and enterovirus. A community-based study in Nigeria, Tanzania, and Ethiopia found that only 10%-14% of patients had a specific etiology,77 suggesting that the epilepsy etiology needs to be clarified further to provide an accurate direction and strategies for the treatment.
Parasitic infections associated with epilepsy are common in SSA, especially in areas with poor health.83 In such areas, seizures occur in up to 90% of patients with active cysticercosis and in non-active cysticercosis with cerebral calcification. A population-based meta-analysis reported that a 10% increase in onchocerciasis is associated with an average 0.4% increase in the prevalence of epilepsy.77 In Africa, differences in epilepsy were observed in onchocerciasis endemic areas. Generally, the epilepsy onset peaked around the age of 5-18 years, but in the onchocerciasis endemic areas, it peaked at the age of <5 years. Also, the incidence of epilepsy among children younger than 5 years increases with the rising microfilariae load; also, Nods spasm and severe developmental delay are observed.84
In Mali, a West African region well-known for the malaria epidemic, exposure-nonexposure methods included 101 cases of cerebral malaria and 222 cases of asymptomatic type in children aged 0-15 years. According to the reported results, the risk of secondary epilepsy was higher in the cerebral malaria group than in asymptomatic malaria,85 which illustrates that malaria has a major role in induced epilepsy. Moreover, a 2010 study in SSA in a tropical area showed that malaria affects about 174 million people or 81% of the global population, and diseases caused by Plasmodium falciparum and Plasmodium vivax malaria have been responsible for epileptic seizures in children in this region. At a hospital in Kenya, epilepsy was caused by malaria in 69% of hospitalized children.86
Another study conducted in Cameroon, a country in central and western Africa, showed a higher prevalence of epilepsy than in industrialized and other developing countries, and cysticercosis caused by Taenia solium infection was a major cause of epilepsy. In recent years, changes in the prevalence of epilepsy in Latin America have become obvious in countries with prevalent cysticercosis, resulting in a higher incidence compared to western countries and a prevalence that is inversely proportional to the per capita GDP of the country.87
However, whether antiparasitic drugs can improve seizures is yet controversial. Accumulating evidence suggests that treatment with antiparasitic drugs reduces the epileptic seizures in patients with parasitosis, at least by reducing the frequency of progression from focal epilepsy to bilateral convulsive seizures. Another study conducted in Uganda showed that ivermectin-treated onchocerciasis improved seizures in PWE. Moreover, in SSA, about 22.9 million people are living with HIV (57/100 million); a study has shown that 4%-17% of people living with HIV develop new seizures.88
2.3.2 Perinatal illness
Unlike in adults, it is necessary to take the perinatal process seriously in infant patients with epilepsy. Infants and young children are likely to be affected by various factors during the perinatal period, resulting in epilepsy. For example, infectious diseases, including some vertically transmitted diseases, trauma during childbirth, intracranial ischemia, and hypoxia, affect the growth and development of the nervous system in newborns and infants. The effect causes the neurons in the brain to fire abnormally, leading to seizures. A previous study of children with epilepsy aged 0-18 years conducted in Burkina Faso, West Africa, 2016 showed that the average age of onset in 115 children included in the study was 8.2 years, and the condition was predominant in males. This study aimed to statistically analyze the non-genetic factors related to the etiology of children with epilepsy. The results showed that perinatal events accounted for 79.1% of the risk factors in children with epilepsy. Brain sequelae of perinatal adverse events, central nervous system infection, and craniocerebral injury accounted for 34.8%, 14.8%, and 5.2%, respectively, which were the primary causes of non-hereditary epilepsy in children and adolescents.89 Preterm birth is also associated with a high risk of seizures. According to a study that compared the status of epilepsy in Asia and Africa, preterm birth increased the risk of epilepsy five-fold. Among the top 10 countries with the highest number of preterm births, six are in Asia (India, China, Pakistan, Indonesia, Bangladesh, and the Philippines) and two in Africa (Nigeria and the Democratic Republic of the Congo).90 Therefore, the non-genetic etiology of young children with epilepsy in tropical areas also deserves attention.
2.3.3 Stroke
In tropical areas, some stroke patients suffer from post-stroke seizures (PSS), which affects the morbidity and mortality of PWE. A large multicenter study conducted in 15 hospitals across Nigeria and Ghana showed that PSS occurs in 499/3344 (14.9%) adults. A study that included selected stroke patients in Ghana also showed PSS in 1101 participants.91 In another study, 126 patients exhibited post-stroke epilepsy (PSE).92 These post-stroke seizures or seizures led to poor prognosis and posed a significant threat to the patient's nervous system, and even caused other health issues. Therefore, PSS affects the morbidity and mortality of PWE in tropical countries and poses a significant burden to tropical countries, especially those with low economic and medical levels.
2.3.4 Head trauma
Typically, head trauma is a cause of epileptic seizures, but not the most common cause. However, the results of a case–control study in Nigeria and Kenya suggested that head injury is a major risk factor for PWE in this region,77 which might be related to the social situation of some tropical countries. For example, in some African regions, traffic accidents frequently occur due to imperfect traffic laws and regulations, lack of relevant management, and indifferent safety awareness, thereby showing a prevalence of traumatic brain injury. In addition, social factors, such as injuries at work, personal fights, and wars, may increase the incidence of head trauma in the region.93 Thus, the lack of neurosurgeons also aggravates the risk of head trauma among patients, that is, a large number of people may suffer from head trauma and experience epilepsy as they cannot receive timely or appropriate treatment; this issue should be investigated further.
2.3.5 Nutrition
Malnutrition is a perpetual global public health problem, and the correlation between malnutrition and epilepsy is a complicated issue. Due to economic constraints, a part of the population cannot afford proper nutrition needed for normal life activities in the majority of tropical countries. In infants and adolescents, as well as some adults, malnutrition causes growth deprivation of brain tissue in the stage of brain development, which tends to increase the susceptibility to epilepsy.94 Also, the lack of nutrients in the body leads to low immune function and dysplasia of the nervous system, which can cause defects of the nervous system and induce the occurrence or aggravation of epilepsy. On the other hand, epilepsy may also lead to malnutrition. PWE use various drugs in the process of treatment or adhere to the ketogenic diet and other treatment methods. They may also suffer from secondary malnutrition, which aggravates the seizure of epilepsy. Usually, this vicious cycle has a significant impact on the prognosis. A study conducted in Benin showed that the prevalence of malnutrition in PWE (regardless of age) was about 22.1% (9.2% in the control group, P < 0.001).95 Another study based on a large demographic survey showed that the prevalence of malnutrition among children with epilepsy in Africa was about 25.4%.96 Thus, malnutrition does affect epilepsy patients. However, as the onset of epilepsy may contribute to malnutrition, it should be considered in PWE, especially among children.
2.3.6 Culture
The influence of different cultures and the infiltration of religious beliefs propagates a wrong perception of epilepsy in many tropical countries, which places PWE under psychological pressure or stigmatization. Because of the poor understanding of the condition, people do not treat it as a common disease but as some mysterious force on the human body. The consequences of such a wrong perception are very serious, as they can delay the optimal treatment opportunities for patients or completely deprive them of suitable treatment. A link was found between epilepsy and stunting in Ethiopia, raising the possibility of a link between early malnutrition and epilepsy in the tropics. On the other hand, there are some misunderstandings about the treatment of epilepsy. There is no clear understanding of whether epilepsy can be treated by drugs, surgery, and other methods, which might delay the timely treatment of patients. These challenges are attributed to incomplete local publicity and lack of promotion of relevant education. For example, in Africa, most individuals do not think of epilepsy as a neurological disease but as a cultural, religious, or spiritual disease. Also, many people do not know that it can be treated with low-cost antiseizure medication (ASM) and that its onset can be controlled. This makes it difficult to improve the diagnosis and treatment of epilepsy in Africa. Some studies have shown that indigenous, Christian, and Islamic beliefs toward epilepsy in Africa have limited the development of relevant medicine in these areas, as these unscientific attitudes have prevented the African governments from providing adequate resources for the treatment, research, and training of medical professionals.76
2.3.7 Genetics
In Africa, epilepsy was instigated by unclear causes in >60% of children,97 suggesting that the influence of genetic factors in children with epilepsy should be emphasized in determining the etiology when excluding the perinatal factors.
In summary, there are various possibilities that could explain the etiology and inducement of PWE in tropical areas. The universality and particularity between tropical and non-tropical countries should be fully considered in the analysis and research of tropical countries. Specifically, the unique characteristics of tropical areas should be considered, including direct factors, such as the unique climate environment and pathogens, and indirect factors, such as social environment and resource problems. In addition to the factors mentioned above, it is also necessary to consider various indirect causes of epilepsy, such as brain tumors and immune system diseases. Understanding and analyzing the etiology of PWE in tropical areas from multiple angles might improve its diagnosis and treatment status.
3 CHALLENGES AND INTERVENTIONS
3.1 Professionalism and medical resources
Due to the low economic levels, most tropical countries suffer from a lack of medical resources, including shortage of medical equipment and drugs, insufficient medical personnel, and a lack of specialist doctors and grassroot medical staff.
A survey showed that poor health facilities and inadequate training of health workers in Africa76 are the primary reasons for the high prevalence and morbidity of epilepsy and the failure of timely diagnosis and treatment of PWE. Also, the relevant professionals in South Africa were inadequately trained and lacked compassion and respect.98 This prompted negative emotions in PWE while receiving treatment, leading to or further aggravating stigma, in turn affecting their normal social activities and daily life. On the other hand, this phenomenon may give rise to negative feelings about the treatment, thus reducing treatment effectiveness and ultimately leading to a poor prognosis.
In addition, the issue of the shortage of medical personnel needs to be resolved urgently. According to one survey, Bhutan, a low- to middle-income country in Southeast Asia, has no neurologists in its public health care system.99 In Italy, there is an average of one neurologist for every 5000 inhabitants, while in Malawi, there are only two neurologists for about 18.5 million inhabitants.100 The lack of specialists not only strains the health resources of tropical countries but also undermines the health of their population. As epilepsy is a common chronic disease of the nervous system, long-term scientific diagnosis and treatment are the most critical means to promote the rehabilitation of patients. Therefore, tropical countries should focus on the shortage of specialists to ensure that local PWE receives timely diagnosis and treatment and has an improved QoL and prognosis.
3.2 Comorbidity
In recent years, epilepsy comorbidity has become a global topic of interest. As a result, a large number of experts and scholars have focused on the problem of comorbidity in PWE. The current studies on epilepsy comorbidities, also in tropical countries, are mainly focused on mental diseases, such as epileptic comorbidities, anxiety, and depression.
The results of a meta-analysis showed that the prevalence of depression in PWE in SSA was about 32.71%, which is related to the local level of comprehensive treatment.101 Due to insufficient medical resources, many patients with comorbid epilepsy cannot receive a treatment plan tailored to their individual situations. Some specialists ignore the patients' clinical manifestations and treatment needs due to the lack of awareness of comorbidities. In the Republic of Benin, a study of 196 subjects, aged >18 years, showed that PWE might be significantly associated with severe anxiety (79.8%) or depression (89.6%) compared to normal controls (12.3% and 46.9%). Also, women were more likely to be affected than men.102
In conclusion, increasing evidence suggests that the role of comorbidity in the development of epilepsy should not be underestimated. The negative emotions of epilepsy comorbidity may have serious adverse effects on the QoL, including family and social life. Therefore, we urge the governments and medical institutions in tropical countries to focus on the comorbidities in PWE and promote their mental health for early recovery.
3.3 Stigma and psychosocial environment
Unlike other prevalent chronic diseases, such as hypertension or coronary heart disease, a stigma is a common event with a high incidence among PWE. According to Weiss and Ramakrishna, health-related stigma is “a social process or related personal experience characterized by exclusion, rejection, blame, or devaluation that results from experience or reasonable anticipation of an adverse social judgment about a person or group identified with a particular health problem.”103 Similarly, PWE who are frequently stigmatized may equally sustain such distress.
On average, stigma among PWE originates from the disease, the patient's sense of shame, and prejudice from the social environment. From the perspective of PWE, acute epileptic seizures that can occur at any time may give rise to a sense of shame to some extent. Furthermore, this unhealthy psychological state of PWE may increase with time, negatively affecting the patients' mental health and reducing their QoL.
Therefore, the factors leading to stigma among PWE are being investigated. Rice et al.104 recruited a prospective cohort of PWE at the Lgnace Deen Hospital in Conakr, including 249 PWE (112 females and 137 males) and reported that “epilepsy stigma is more of a societal issue than a biological one.” In the study, the stigma scale of epilepsy (SSE) was regarded as the primary outcome measurement. The subjects had an average SSE score of 46.1 points (standard deviation = 14.5, the total score was 0-100). Based on the findings, it could be concluded that the frequency of seizures and depression level was positively associated, while household wealth was negatively associated with stigma, which was consistent with the multivariate analysis model.
Children are a special group of PWE and face multiple burdens. Many children with epilepsy are prevented from attending school in parts of Africa due to discrimination. Some of them are not allowed to eat with their families. Stigma also leaves these children with few or no childhood friends, which might cause severe psychological damage that is difficult to heal.105, 106
Currently, research on stigma among PWE is lacking, including large scientific and valid data as well as targeted analytical methods. Nonetheless, the psychological problems of PWE, except stigma, including depression or anxiety, have gained increasing attention in recent years.
In summary, PWE-associated stigma should be analyzed at multiple levels. As described above, it is a social problem and not only a medical condition. Consequently, a friendly psychosocial environment and a medical professional perspective have significant roles, which is time-consuming and arduous but crucial during this process.
3.4 Policy and normative management
Being a chronic disease, strong policy preference and long-term standardized management are indispensable links in disease diagnosis and treatment for epilepsy. In this aspect, tropical countries have some shortcomings. For example, the public health system for epilepsy control is inadequate; policy is not yet implemented in most regions; lack of epilepsy-related chronic disease management methods and a complete treatment system, including the whole process from prevention and treatment to prognosis. Moreover, community hospitals and other basic medical service institutions have failed to provide the expected services; however, in recent years, many countries in the tropical region have been actively improving the medical environment for PWE.
Currently, there are 21 national epilepsy societies in Africa dealing with social issues and 14 national professional associations dealing with the scientific aspects of epilepsy. Initiatives already underway in Africa include establishing the Epilepsy Society, the Global Campaign Against Epilepsy (GCAE), and the Regional Congress. The Global Epilepsy Society in Africa has several achievements, including the declaration on Epilepsy in Africa, the establishment of new epilepsy societies in the region, and demonstration projects in Senegal and Zimbabwe. Other projects demonstrated that it is possible to manage epilepsy with limited resources. Increased health awareness among the population, availability of affordable medicines, and effective training of health workers are key components of successful epilepsy management.76 In addition, the ongoing restructuring of the health system in South Africa has identified healthcare workers as a critical link in primary healthcare to ensure the sustainability of interventions and reduce the treatment gap for epilepsy in rural South Africa.41 In resource-poor settings in rural Guinea-Bissau, local community rehabilitation services have bridged the gap in epilepsy treatment and improved patient compliance. Furthermore, continuous clinical guidance for complicated cases improves the clinical treatment effect.107 In Ghana, a new mental health bill was passed in 2012, which increased the allocation of health resources for mental disorders and epilepsy.77 In response to the characteristics of tropical regions, many countries are actively improving their environmental health, undertaking malaria eradication activities, reducing transmission, and improving the control of tropical pathogens, such as cysticercosis, cystic echinococcosis, and onchocerciasis, and reducing the risk of infection.
SSA is known for the lack of transition from child care to adult care.77 The problem might also exist in other tropical countries. Thus, we look forward to additional data that would allow professionals to develop prompt and reasonable solutions. Nonetheless, many countries in the tropical region are making efforts to improve the status of epilepsy treatment. Interventions at the government level are showing promising results. As a result, PWE in the tropics is expected to have better access to medical resources.
4 CONCLUSION
In recent years, epilepsy has been understood rather clearly increasingly in most regions worldwide. For different types of epilepsy caused by different reasons, scientists and clinical workers are actively seeking effective treatment strategies and have made remarkable achievements. However, epilepsy has been a common chronic disease of the nervous system. Due to the lack of distinct regional characteristics, only a few individuals have explored its specificity in tropical areas. The current studies have shown that most tropical countries have a high incidence and prevalence of epilepsy,108, 109 a large number of PWE are not properly diagnosed and treated, and there may even be some undiagnosed PWE. This situation places a serious burden on the development of tropical countries. This phenomenon as the focus of the disease and the interests of the patients should be investigated further. First, for some patients who have not been formally diagnosed with epilepsy, due to neglect, cannot receive timely treatment, resulting in a poorer prognosis than in those who have the same condition but receive timely treatment; this affects the long-term QoL of patients and increases the burden of epilepsy diagnosis and treatment in tropical areas. Second, for patients who have been diagnosed with epilepsy, the etiology of the disease in tropical areas has not been fully explored, indirectly leading to the lack of targeted diagnosis and treatment strategy; thus, this subgroup of patients did not receive the correct treatment, which would pose a threat to the long-term QoL of patients and accelerate the progress of the disease, forming a vicious cycle. Therefore, as a neglected perspective of epilepsy in tropical areas, there are many problems that have not been explored but cannot be ignored.
Therefore, in the face of various difficulties and challenges, there is a lot of work required to improve the economic level, improve the health policies and systems supported by the government and society, promote the allocation of medical resources, raise residents' health awareness, improve health conditions in tropical areas, popularize scientific knowledge, adopt effective prevention strategies, train grassroots medical staff, and form a standardized management system. The need to support the diagnosis and treatment of epilepsy in the tropics at the national and governmental level may help to create a favorable climate for PWE at the societal level and reduce the likelihood of comorbidities. At the technical level, relevant inspection and treatment equipment should be improved to ensure an adequate supply of ASM, improve the diagnosis and treatment level of medical personnel in tropical countries, and provide scientific and effective diagnosis and treatment plans for PWE.
From the clinical point of view, it is necessary to establish a systematic clinical management system for tropical epilepsy patients. As a chronic disease, accurate diagnosis and treatment alone cannot fundamentally solve the problem. Furthermore, it is necessary to popularize relevant knowledge for local people, use local cultural advantages, eliminate unscientific disease cognition, correctly understand the disease, prevent the occurrence of disease, and create a good social atmosphere under the premise of respecting different historical backgrounds, religious beliefs of various countries, and perspective of tertiary prevention, in the etiological prevention stage. In the pre-clinical prevention stage, various etiological and epidemiological studies can be carried out in different countries and regions to quickly, comprehensively, and emphatically improve the data bank of tropical epilepsy and improve the diagnosis and treatment level of epilepsy with tropical characteristics. This would achieve early detection, diagnosis, and treatment that might improve the prognosis and QoL of patients. Finally, in the stage of clinical prevention, apart from hiring a large number of professional doctors for treatment, an effective management system between the hospital and the community should be considered (regional management can be considered in some economically underdeveloped areas), family beds should be set up in local grassroots community hospitals, comprehensive management mode centering on epilepsy patients should be advocated, and long-term follow-up mechanism should be established. To carry out community rehabilitation, improve the self-management level of patients, strengthen psychological guidance for patients, reduce the incidence of anxiety, depression, and other comorbidities of patients, and reduce the stigma of patients and their caregivers that would promote the mental health of patients and the recovery of the disease. In addition, there are special age groups of epilepsy patients in the tropics. For young children, attention should be focused on the problems of nutrition and genes; for. For women of childbearing age, attention should be focused on the management of pregnancy and perinatal period, including folic acid supplement. For the elderly population, the presence of other underlying diseases, such as epilepsy, that are neglected in the tropics, the interaction of multiple drugs, and the mental health, and QoL should be monitored closely.
Therefore, we hoped that additional studies on epilepsy patients in tropical countries would update or fill the data gaps. Moreover, in the process of formulating epilepsy management strategies, it is necessary to take into account the historical and cultural differences between different countries in tropical regions and the scientific nature of disease cognition, design respectful and reasonable clinical management policies, and improve the cooperation of patients and their families. Also, we must strive to provide practical and meaningful help for the health of PWE in tropical areas at the earliest.
ACKNOWLEDGMENTS
We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this report is consistent with those guidelines. We also thank the support of grants from the National Natural Science Foundation of China (81960249, 82260270), the Hainan Province Science and Technology Special Fund, Key Research and Development Project of Hainan Province (ZDYF2021SHFZ092, ZDYF2022SHFZ109), the Hainan Province Science and Technology Special Fund, Natural Science Foundation of Hainan Province (822RC832), and the Epilepsy Research Science Innovation Group of Hainan Medical University (2022), Hainan Province Clinical Medical Center (2021), and the Excellent Talent Team of Hainan Province (No.QRCBT202121). These figures were created by Biorender.
CONFLICT OF INTEREST
The authors have declared that they have no competing interests