How the characteristics of pediatric neurologists in Latin America influence the communication of sudden unexpected death in epilepsy to patients and caregivers
Abstract
Objective
This study aimed to describe the characteristics of pediatric neurologists (PNs) in Latin America (LA) who attend to children and adolescents with epilepsy and convey to them the risk of sudden unexpected death in epilepsy (SUDEP).
Methods
Personal data and details of discussion of SUDEP with families, including relevance of SUDEP disclosure, frequency of such communication, perceived benefits and risks of disclosure, extent of training received on such disclosure, and professional experience with SUDEP, were collected through an online survey of PNs from LA. Their personal experience in carrying out this conversation was obtained through responses to an open question, further used to identify the main barriers.
Results
Of the 442 surveys received, 367 (83%) were analyzed. Most participants (73.8%) responded that the communication of SUDEP risk was relevant or very relevant; however, only 17.9% reported communicating it always or very frequently. Factors that increased the frequency of SUDEP communication included patients with higher levels of complexity (OR = 2.18, P = .003) and the physician's personal experience with SUDEP (OR = 2.305, P < .001). Direct questions from the family and avoiding scaring them about a rare outcome were the main motivations behind discussing and not discussing SUDEP, respectively. In the open question, respondents identified worries about the patient's ability to understand the information and cultural gaps as barriers. “Informing with the intention of improving adherence to treatment” and “establishing an empathic relationship” were significantly related. Further, the concept of “do not scare” was significantly related to “personal difficulties in discussing SUDEP.”
Significance
Although most PNs agree that communication about SUDEP is relevant, only a minority actually engages in it. Participants identified a lack of appropriate training in such communication as a barrier. A better understanding of communication expectations, education of health professionals, and communication techniques have a strong relevance in diminishing the gap between guidelines and practice.
Key points
- Most Latin American pediatric neurologists find it relevant or very relevant to communicate the risk of SUDEP to patients and caregivers
- Pediatric neurologists in Latin America infrequently communicate the risk of SUDEP to all patients
- Risk factors are the main motivation to talk about SUDEP
- Not scaring patients and the absence of effective prevention measures are the main reasons for not talking about SUDEP
- Training of pediatric neurologists in SUDEP and in delivering bad news could be a good strategy for improving standards of care
1 INTRODUCTION
An estimated 50 million people worldwide suffer from epilepsy,1 which represents 0.5% of the global burden of disease. The mortality in patients with epilepsy is 2-3 times higher than that in the general population.2, 3 The main causes of death in patients with epilepsy are related to consequences that occur after a rapid succession of seizures, sudden deaths related to seizures, and accidents resulting from a seizure.4 Sudden unexpected death in epilepsy (SUDEP) is defined as a death that occurs suddenly and unexpectedly, is witnessed or unwitnessed, and is not associated with trauma or asphyxia. It occurs in patients diagnosed with epilepsy, excluding those with documented status epilepticus, whose postmortem anatomical-pathological study does not reveal structural or toxicological underlying signs for the cause of death.4-8 It has been shown that SUDEP is responsible for up to 15% of all deaths in epilepsy.9, 10 In comparison with other neurological disorders, one of the most relevant effects of SUDEP is related to the years of potential life lost (YPLL). This indicator shows the relative burden of this neurological disease. It has been estimated at over 100 000 YPLL among the US population.11
The mechanisms seem to be multifactorial, such as cardiac arrhythmia; respiratory, systemic, and/or cerebral circulatory dysfunction; and metabolic and hormonal changes induced by seizures, with the changes occurring during or after seizures.5, 9
Epidemiological research has been a challenge because of the low reporting of cases, inaccurate death certificates, few postmortem studies of the patients, and the difficulties in establishing a single definition of the concept.7, 8, 12, 13 In a recent retrospective study from Denmark, it was reported that after adjusting for age and sex, persons with epilepsy younger than 50 years had a significant increase in all-cause mortality and high SUDEP risks among others.14 The risk of SUDEP in children is reported to be less common than that in adults, affecting 17.6/100 000 children with epilepsy.15 However, recent studies have revealed that the incidence of SUDEP in children is similar to that reported in adults.16, 17 In a study that analyzed the opinions of 26 young adult patients with epilepsy, the authors concluded that most of the patients and their caregivers wanted to know about the risk of SUDEP and wanted to be told early on and that patients did not have prolonged anxiety due to its disclosure.18 The inability to prevent all cases makes many providers reluctant to talk about SUDEP. Nevertheless, communication of this risk is necessary, but there is no consensus about the best strategies for healthcare professionals to communicate SUDEP to patients.
It may be difficult to identify the appropriate time to address the risk of SUDEP, although experts recommend structuring an early patient-centered plan aiming for clear and empowering communication.6 Few studies have addressed this question, and different answers have been found. Studies through surveys and review of clinical records showed that neurologists and pediatric neurologists report the risk of SUDEP to a minority of their patients with epilepsy and generally do so several months after diagnosis.19-21 The different attitudes of healthcare professionals in communicating the risk of SUDEP to patients and their caregivers reveal fundamental differences in the quality of medical care.
The aim of this study was to describe the personal characteristics, experiences, and attitudes of pediatric neurologists (PNs) in Latin America (LA) who attend children and adolescents with epilepsy and relate these characteristics to their communication of the risk of SUDEP to patients and caregivers. Understanding how the personal characteristics of health providers influence the way they communicate the risk of SUDEP may be beneficial and helpful for creating guidelines that would lead to a more standardized medical care for all.
2 METHODS
2.1 Study participants and data collection
Latin America is the region extending from Mexico all the way down to the most southern permanently inhabited place in the world, the Chilean Patagonia. LA has approximately 650 million inhabitants and is one of the most urbanized regions in the world. The majority of residents live in urban settings; however, some rural areas of South America are extremely remote with very low access to a PN. The gap in access to a PN is significant among LA countries, with 1 to 15 PNs per million inhabitants as extremes. To our knowledge, no studies have explored how LA healthcare professionals communicate the risk of SUDEP to patients and their caregivers.
Pediatric neurologists from LA were invited to participate in an online survey in August 2020. A formal invitation was sent to the Pediatric Neurology Societies for each of the 20 different LA countries, as well as informally through email, WhatsApp, and organizations linked to epilepsy care, with the intention of reaching approximately 2500 PNs registered in all the countries consulted. The invitation contained a link that redirected the participants to the online survey. Consent was required previous to accessing the survey. The questionnaire asked about personal characteristics such as age, gender, medical specialty, city, country, experience treating patients with epilepsy, and complexity of patients with epilepsy attended. Complexity was defined by levels, depending on the severity of the disease. Primary level corresponded to providers in private offices or health centers where nonrefractory patients are attended; secondary level was hospital providers where the diagnosis is done, medical strategies are used, and chronic stable patients are attended; and tertiary level includes mainly refractory patients and potential surgery candidates treated by epileptologist. Relevance and frequency in the communication of SUDEP to patients and caregivers, the opportunity to address this topic with patients and caregivers with whom they talk about this topic, patients included or only with caregivers, the main motivations for talking or not talking about SUDEP, training background in delivering bad news, and whether they had professional experience with SUDEP with some patients were also addressed. Finally, an open question requested information about personal experience in ways to carry out this conversation and the main barriers experienced in the process.
The exclusion criteria for analysis were incomplete responses, physicians who were not PNs, and those who did not attend patients with epilepsy. PNs who attended pediatric patients with epilepsy were included in the study. This study was approved by the Scientific Ethics Committee of Centro de Bioetica—Facultad de Medicina Universidad del Desarrollo—Clínica Alemana de Santiago, Chile. Participants consented to participate voluntarily in the survey.
2.2 Statistical analysis
Continuous variables are described as means, standard deviations, and quantiles. Categorical variables are described as frequencies and percentages. Ordinal logistic regression analysis was used to model factors associated with the relevance and frequency of communication of SUDEP to patients and caregivers. Furthermore, a simple correspondence analysis was performed to show the relevant associated categorical variables and shown by biplot graphs. The association between ordered P-values below .05 was considered statistically significant, and all confidence intervals were at 95%. Data were processed using STATA 16.0 (StataCorp. 2019. Stata Statistical Software: Release 16).
A response coding process was conducted for the open question of the survey. This involved assigning a numerical code to the answers, allowing them to be grouped according to a central theme, and subsequently working them quantitatively in terms of frequency and from the association between concepts with Fisher's exact independence test. The main concepts constructed from the open question were as follows: (a) “Adherence to treatment,” which refers to the fact that the main objective of discussing SUDEP is related to improving adherence to medical treatment; (b) “Understanding of the problem” concept is related to the concern of PNs that patients, their relatives, and caregivers will not understand this information and the effects on their daily lives; (c) the “Do not scare” concept is constructed as the notion that when talking about SUDEP, the goal is not to scare patients and caregivers about a rare event; (d) the “empathy” concept is related to an orientation that considers the emotions expressed by the patient and caregivers, which determines how the topic is communicated; (e) “Informing” was defined as an interest expressed in the open question focused on the delivery of information; (f) “Paternalism” refers to the notion that PNs decide how much information patients and caregivers can handle about this topic; and (g) “The personal difficulty in communicating bad news” refers to the fact that the main idea conveyed in the open question is related to the difficulties and lack of skills of PNs in communicating complex issues and the fear of generating discomfort in the patient and caregivers.
3 RESULTS
A total of 442 surveys were received from 20 countries. Of the surveys received, 367 responses fulfilled the inclusion criteria and were analyzed. Based on the official number of PNs in LA, our survey had a response rate of 18%. The personal characteristics of PNs who participated in this study are presented in Table 1. Of the respondents, 246 of 367 (67%) were women, and 306 of 367 (83%) were between 30 and 60 years old. In addition, 140 of 367 (38%) PNs had more than 15 years of experience attending to patients with epilepsy. Respondents were distributed among care settings to patients at different epilepsy complexity levels: 76 of 367 (21%), primary; 154 of 367 (42%), secondary; and 137 of 367 (37%), tertiary level, and 127 of 367 (34%) of the participants had firsthand experience with SUDEP. Most of the respondents were concentrated in Chile (32%), followed by Brazil (15%), Mexico (11%), Argentina (8%), and Colombia (8%).
| Parameters | n | % |
|---|---|---|
| Gender | ||
| Male | 119 | 32.4 |
| Female | 246 | 67 |
| Personalized | 2 | 0.5 |
| Age (range) | ||
| 20-30 years | 17 | 4.6 |
| 31-40 years | 141 | 38.4 |
| 41-50 years | 89 | 24.2 |
| 51-60 years | 76 | 20.7 |
| 60-70 years | 36 | 9.8 |
| 71-100 years | 8 | 2.1 |
| Years of clinical experience attending to patients with epilepsy (range) | ||
| Less than 5 years | 74 | 20.2 |
| 5-10 years | 96 | 26.2 |
| 11-15 years | 57 | 15.5 |
| More than 15 years | 140 | 38.2 |
| Country of practice | ||
| Argentina | 30 | 8.2 |
| Bolivia | 7 | 1.9 |
| Brazil | 55 | 15.0 |
| Chile | 116 | 31.6 |
| Colombia | 29 | 7.9 |
| Costa Rica | 3 | 0.8 |
| Cuba | 6 | 1.6 |
| Dominican Republic | 4 | 1.1 |
| Ecuador | 7 | 1.9 |
| El Salvador | 6 | 1.6 |
| Guatemala | 4 | 1.1 |
| Haiti | 1 | 0.3 |
| Honduras | 2 | 0.5 |
| Mexico | 39 | 10.6 |
| Nicaragua | 1 | 0.3 |
| Panama | 3 | 0.8 |
| Paraguay | 6 | 1.6 |
| Peru | 7 | 1.9 |
| Uruguay | 22 | 6.0 |
| Venezuela | 19 | 5.2 |
| Level of complexity of patients with epilepsy | ||
| Primary care | 76 | 20.7 |
| Secondary care | 154 | 42.0 |
| Tertiary care | 137 | 37.3 |
| Personal experience with cases of SUDEP | ||
| Yes | 127 | 34.6 |
| No | 240 | 65.4 |
- Abbreviations: SUDEP, sudden unexpected death in epilepsy.
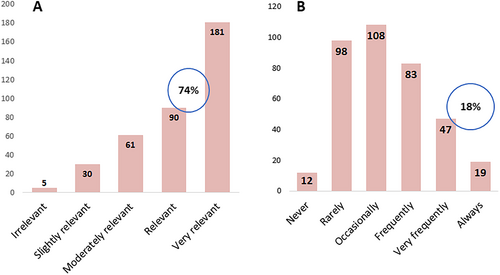
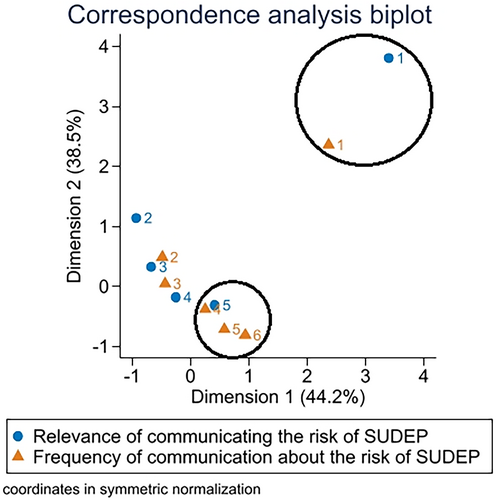
Most participants (271/367 [73.8%]) reported that communication of the risk of SUDEP to patients and caregivers was relevant or very relevant; however, only 66 of 367 (17.9%) participants reported that they frequently or always discussed this risk with families. The perceived relevance and reported frequency of communication about SUDEP are shown in Figure 1. No significant correlations were noted between age of the PN, years of experience, or country with either the perceived relevance or frequency of the communication of SUDEP to the patient and caregivers. A higher level of complexity of patients (OR = 2.18, P = .003) and a physician's personal experience with SUDEP (OR = 2.305, P < .001) significantly increased the frequency of communication of the risk of SUDEP to patients and caregivers. The correspondence analysis biplot shows a close relationship between the perceived relevance and frequency of communication about the risk of SUDEP (Figure 2, marked in circles). PNs who viewed SUDEP discussion as very relevant were significantly more likely to report discussing this very frequently (OR = 5.3, P = .028) or always (OR = 30.2, P < .001) with families.
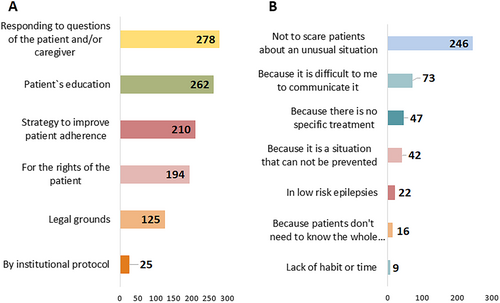
The reasons for communicating or not communicating SUDEP risk are presented in Figure 3. The most frequent motivation for discussing the risk of SUDEP was to answer a patient's direct questions (278/367), as part of the patient's education (262/367), and to improve adherence to treatment (210/367). The only significant association was between the level of complexity of patients and the intention of improving adherence to treatment (primary- to secondary-level OR = 1.9 [CI 1.06-3.4] and primary- to tertiary-level OR = 2.3 [CI 1.2-4.1]). The most reported reason for avoiding such discussion was not to scare patients about an unusual situation (246/367).
When it came to when PNs should talk about this topic, 293 of 367 (80%) participants thought that the risk of SUDEP should be communicated to patients and caregivers when there is a high risk of SUDEP, while only 66 of 367 (18%) thought that it should be discussed at the time of the epilepsy diagnosis.
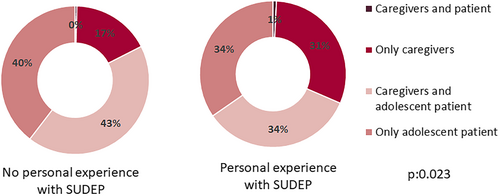
In relation to who should be present during this conversation about SUDEP, participants' responses differed in the case of children and adolescents, with 227 of 367 (62%) PNs speaking only to parents if the patient is a child, and if the patient is an adolescent, 282 of 367 (77%) thought the patient should be present. No association was found between the persons present for communication of SUDEP (patients and/or caregivers), PN's experience (years attending to patients with epilepsy) (P = .20), or the level of complexity of patients (P = .44). On the contrary, participants with firsthand experience of patients with SUDEP more commonly spoke only with parents than those without firsthand experience did (110/367 [30%] vs. 62/367 [17%], P = .003) (Figure 4). Very few respondents reported institutional protocols regarding SUDEP disclosure to which PNs are bound to in LA (25/367, 6.8% [CI 4.5%-9.9%]).
Regarding the results of the open question, the concept “informing” was the one that was repeated the most among the respondents and that is associated with the relevance of informing patients with epilepsy and their caregivers. From an analysis of the association of concepts, a significant relationship was highlighted between “informing” with the intention of improving “adherence to treatment” and establishing an “empathic relationship” with the patient with epilepsy and their caregivers. Another significant association between concepts is that when PNs reported “do not scare” as a factor for not discussing SUDEP, they also mentioned with high frequency the “personal difficulties in discussing SUDEP.”
4 DISCUSSION
Access to PNs is disparate among LA countries, and the majority of respondents worked in the most populous cities in each country. This study had a low participation rate (18%, 367/2039). This situation is similar to other studies where the response rate varies between 10% and 16%.17, 20, 22, 23 Professional experience in epilepsy treatment was a common factor among respondents, as 80% of them had more than 5 years of experience treating patients with epilepsy. A discrepancy was found between what PNs do in a SUDEP consultation and what is recommended in current clinical guidelines, where there is still a debate regarding the ethical position of when to inform patients with low risk of SUDEP,21 among other things. These results (always: 5.17%; never: 3.27%) are similar to those of other investigations that analyzed the attitudes of PNs when discussing SUDEP with their patients and caregivers throughout the world (Table 2). Comparing these results, there is a range between 1% and 20% who provide counseling to all (or almost all) patients and caregivers, and between 1% and 85% who do not provide any counseling. Furthermore, in this study, the frequency of communication was related to personal experience with SUDEP and the level of complexity of patients. As the risk of SUDEP is higher in those cases, it is more frequently communicated at the tertiary level of complexity, which means refractory cases in advanced centers of epilepsy. This is in line with other research where there is evidence of a selection of patients and caregivers who are informed according to the associated risk factors and the possibility of changing behaviors.23
| Study | PNs of LA | Donner 2021 | Kadummukasa 2019 | Galli 2017 | Strzelczyk 2016 | Friedman 2014 | Vegni 2011 | Gayatri 2010 | Morton 2006 |
|---|---|---|---|---|---|---|---|---|---|
| Year of survey | 2020 | 2017-2018 | 2017-2018 | 2015 | 2014 | 2011 | 2009 | 2006 | 2005 |
| Number of physicians | 367 | 369a | 25 | 114 | 519 | 1150 | 190 | 46 | 288 |
| Country included | 20 LA countries | Canada | Uganda | Italy | Aus, Ger, Swit | US, Can. | Italy | UK | UK |
| Rate of counseling all always | 5.20% | 12.2% | 15% > 50%b | 1.80% | 2.70% | 6.80% | 8.90% | 19.60% | 4.70% |
| Rate of counseling never | 3.30% | 1.4% | 85% | 25% | 23.2% | 11.6% | 7.90% | 6.50% | 7.50% |
- Abbreviations: LA, Latin America; PNs, pediatric neurologists; SUDEP, sudden unexpected death in epilepsy.
- a Total number of PNs who participated in two surveys at different times, 84 of whom answered both surveys.
- b Communicate the risk of SUDEP to more than 50% of patients.
Specific features in the pediatric population have been reported to be related to an increased risk of SUDEP, including genetic etiology-channelopathies, such as Dravet syndrome or SCN8A-DEE,5, 24, 25 presence of nocturnal generalized tonic–clonic seizures, high frequency of seizures (3 or more per month), absence of seizure freedom periods, and not escalating treatments in patients who progress to refractory epilepsy and seizures during sleep.26 Male sex, onset of epilepsy before the age of 16, duration of the disease greater than 15 years, patients younger than 16 years with intellectual disability, structural brain injury, abnormal neurological examination, adults who consume alcohol, psychiatric comorbidities, particularly in female patients with epilepsy, and use of anxiolytic medication are other factors that currently have weak or insufficient evidence of increasing the risk of SUDEP.6, 22, 27 Modifiable risk factors, such as medication adherence and avoidance of excessive alcohol consumption, could be modified through education to patients and caregivers.28 Achieving seizure control with combined pharmacological therapy would not result in a higher risk of SUDEP.29, 30 Some studies have proposed that nocturnal supervision may be useful in controlling the risk of SUDEP. Nevertheless, the latest Cochrane systematic review concluded that it found limited and very low-certainty evidence that supervision at night reduces the incidence of SUDEP, and further research is required to identify the effectiveness of other current recommendations.31
Known risk factors, such as refractoriness, compel almost 80% of PNs to communicate about SUDEP. Our study showed that there was a consensus about the necessity of talking about the risk of SUDEP to adolescents with poor adherence or self-care difficulties. However, obtaining information about SUDEP will not, on its own, increase medication adherence in most patients.25 Other strategies to motivate patients to improve their medication adherence must be studied. The majority of PNs in LA prefer not to speak about SUDEP in cases with very low risk. The American Academy of Neurology and the American Epilepsy Society created a guideline stating that patients should receive information about SUDEP in some clinical scenarios: frequent clonic–tonic seizures, epileptic syndromes with high frequency of SUDEP, epileptic seizures during sleep, low adherence to pharmacological treatment, patients who express questions regarding the increase in mortality associated with the diagnosis of epilepsy, and a recent diagnosis.26 Conversely, PNs in LA thought that a personalized approach to the SUDEP discussion should be recommended, considering the personal characteristics of the patient, their caregivers, and the specific diagnosis, emphasizing the negligible risk in most cases. A small observational study in Uganda reported that most adult patients with epilepsy obtained information about SUDEP outside of the healthcare system, but most of them would prefer to receive information regarding the risk of SUDEP from a reliable source such as a physician, early after their diagnosis.32 The same features were found in another United States-based study. Despite most patients with epilepsy and their caregivers reporting fear, anxiety, and sadness after first hearing about the risk of SUDEP, they wanted to discuss it with their doctor. Furthermore, in the same study, over two thirds of respondents wanted to know about SUDEP regardless of its risk, and 37% wanted to talk about it early on in the epilepsy diagnosis.33 Our study did not explore other sources of information available to the patients.
The most relevant motivation to communicate the risk of SUDEP was “Responding to questions of the patient and/or caregiver,” “Patient's education,” and “Strategy to improve patient adherence.” However, the reasons for not communicating SUDEP are related to the desire to not frighten patients and their caregivers with an unusual situation. In an analysis of this survey and the literature, this concept is related to the sensitive nature of the information, the lack of clear knowledge about its pathophysiology, the absence of measures that reduce its risk, and the low incidence of this pathology. However, in the analysis of the open question, the relationship between not scaring patients and the lack of personal skills for delivering bad news stands out. Two cross-sectional surveys of PNs reported concern that discussing SUDEP could provoke excessive anxiety or worry for caregivers; however, when PNs feel they know enough about SUDEP and/or feel ethically obligated, they discuss SUDEP with a greater proportion of their patients. Of the 88 PNs who reported changing their practice after an educational program, 82% changed because they declared they learned more about SUDEP with this educational intervention.23
Pediatric neurologists are undecided on when to first address this topic, because the first consultation with a patient with epilepsy requires delivering information and education on several topics, such as the diagnosis per se, use of medications, and side effects, so it may be difficult to communicate SUDEP due to the limited time of consultation. In addition, physicians recognize that not personally knowing patients and families makes them hesitant to provide this information on the first visit. They think this could create anguish or denial in patients and caregivers, preferring to get a feel for them before broaching the subject. Perceived cultural differences have a strong value in their attitudes toward communicating the risks of SUDEP. Other PNs wait to see the evolution of the epilepsy, therapy response, and etiology so that they are able to assess the real risk before communicating.
Among the reasons reported about why some physicians decide to communicate the risk of SUDEP to their patients include empowering the patient in managing their pathology, the right to knowledge of up-to-date information, and legal concerns.34 The reasons given for not communicating this risk are related to the low probability of occurrence, and the lack of strategies to prevent it and to reduce unnecessary stress in patients and their caregivers.19-21 It is noteworthy that a majority of surveyed participants in one study reported that standardization in the management of the information about SUDEP would be beneficial for patients.34 This relationship highlights the importance of establishing training programs for delivering bad news as part of medical education.
Most of the reasons PNs do not inform the relevant parties about SUDEP are probably to “protect” the patient and their caregivers from bad news, reflected in the answers “not to scare,” “not to inform about an infrequent situation,” and “no effective preventive treatment.” An evaluation of the informal sources of information should be conducted. The belief that healthcare professionals are the sole source of information is unrealistic nowadays. Studies that have explored the perception of caregivers of children with epilepsy about SUDEP highlight the lack of knowledge on the subject, and the lack of opportunity to talk about it.26 The vast majority of studies indicate that communication about the risk of SUDEP is a duty and should be communicated soon after diagnosis.35, 36 However, there is no consensus on a standardized method to deliver this information.6, 31 It is evident that there is a gap between the family and caregivers' expectations with the information they receive, which implies a problem in medical care.
4.1 Limitations and challenges
For the analysis of self-report surveys, the confounding impact of social desirability biases has been frequently documented. It has been observed that respondents can guide their answers according to what they consider to be a correct answer rather than their usual practices. Thus, not considering the social desirability bias in this survey could be a limitation.37 Furthermore, we do not know what patients and caregivers really want to know in LA. We do not know how multicultural beliefs and values influence community expectations for medical attention. New scenarios are open with continuous changes and development of countries and their citizens. Further research is necessary to understand the needs of Latin Americans. Moreover, communication skills are particular to individual physicians, and the effectiveness of their messages to people is very difficult to evaluate. It seems useful to have local guidelines that consider the characteristics of their own population and that incorporate cultural contexts. Likewise, a training program for delivering bad news, such as the risk of SUDEP, could help PNs broach this topic better. Future research should be conducted to evaluate the impact of the different strategies mentioned to reduce the risk of SUDEP and fulfill the informational needs of patients and caregivers.
The distribution of PNs in LA is not uniform, with Chile being one of the countries with higher numbers of PNs per capita. Although scientific societies and PNs from all Latin American countries were invited to participate in the survey, there is an overrepresentation of Chilean PNs in our study. This bias in the sample may be due to the fact that all the authors work in Chile.
5 CONCLUSIONS
Latin America is a diverse region; it is a melting pot, a mix of native, Spanish, Portuguese, European, and African peoples. Moreover, the economic disparity is sizable. Thus, cultural differences emerge powerfully in the characteristics and attitudes of PNs and their communication with SUDEP. This is an important consideration, making it difficult to have a unique guideline or recommendation to approach this topic in different contexts. The discrepancy among the high relevance reported in the communication of the risk of SUDEP and the low frequency they actually communicate is common in the majority of the studies. The level of complexity of patients attended and personal experience with SUDEP encouraged PNs to communicate the risk of SUDEP more frequently. Known risk factors are a strong reason for talking about SUDEP. Most physicians believe that adolescents should be included in the conversation. Professional experience with SUDEP in this study was a reason for leaving patients out of the conversation. It seems necessary to train PNs in this topic. Personal difficulties in delivering bad news were also a limitation in communicating this risk. A standard of care should be provided to all patients and caregivers. A better understanding of communication expectations, education of health professionals in the pathology, and communication techniques have a strong relevance in diminishing the gap between guidelines and practice.
ACKNOWLEDGMENTS
We are grateful to all the PNs of LA that participated in our study. Special thanks to the Chilean Society of Psychiatry and Neurology of Childhood and Adolescence (SOPNIA), the Society of Epileptology of Chile (SOCEPCHI), and Pediatric Neurology Societies of LA for their support. We are thankful for the generous advice provided by Dr. Elaine Wirrell.
CONFLICT OF INTEREST
None of the authors has any conflicts of interest to disclose. We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.