Dynamic electro-clinical changes corresponding to immediate recovery after glucose administration from insulinoma-induced hypoglycemia: Report of two cases
Insulinoma is an endocrine tumor causing hypoglycemia,1 which manifests as various nonspecific symptoms, such as sweating, confusion, tremors, and palpitations, with paroxysmal occurrences.2 Electroencephalography (EEG) during hypoglycemia is characterized by slowing in background activity, and diffuse high amplitude slow activity intermixed with spikes.3-6 However, the electro-clinical process of recovery from insulinoma-induced hypoglycemia with glucose administration is unknown. We treated two insulinoma patients, a 39-year-old man (Case 1) and a 53-year-old woman (Case 2), in whom long-term video EEG monitoring (LTVEM) clarified that their spells were non-epileptic due to hypoglycemia, and characterized the electro-clinical profile. Both patients, without past and family history, had recurrent spells of behavioral abnormalities with impaired awareness. The spells tended to appear either at night (Case 1) or before meals (Case 2) and lasted hours at longest. Soon after spells with alert state, unremarkable physical and neurological examination as well as normal blood sugar, 83 mg/dL (Case 1), were confirmed, and brain MRI showed no cortical lesion. Epilepsy was initially considered, but short-term EEG showed no epileptiform discharges. Antiseizure medications were not effective. LTVEM showed interictal bilateral frontal spikes in Case 1 (Figure 1A). LTVEM also recorded spells as high voltage generalized slowing without electrical evolution (Figures 1B Case 1, and 1E Case 2). During the event, hypoglycemia was confirmed (29 mg/dL Case 1, 30 mg/dL Case 2). Intravenous administration of glucose 10 g resulted in both clinical (improved level of awareness) and electrical improvements (increased frequency, decreased amplitude, and alpha rhythm activity appearance) within a couple of minutes (Figure 1C,D Case 1, and 1F Case 2). Unsuppressed serum insulin (34.1 μU/mL Case 1, 22.4 μU/mL Case 2; normal 1.84–12.2 μU/mL) and C-peptide (6.43 ng/mL Case 1, 3.3 μU/mL Case 2; normal 0.61–2.09 ng/mL) were identified despite the low glucose level (40 mg/dL Case 1, 44 mg/dL Case 2). Abdominal MRI demonstrated tumors in the pancreas of both patients, and histopathological examination identified benign pancreatic insulinoma. Following resection, the patients were released from their spells.
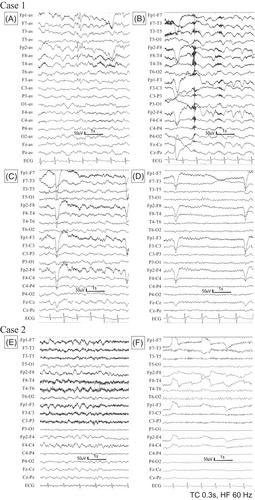
EEG showed bilateral frontotemporal spikes in Case 1. The current definition of interictal epileptiform discharges proposed by International Federation of Clinical Neurophysiology is based on six morphological criteria.7, 8 Case 1 met four of the six criteria as follows: (1) di- or tri-phasic waves with sharp or spiky morphology; (2) different wave duration than the ongoing background activity; (3) asymmetry of the waveform; and (4) distribution of the negative and positive potentials on the scalp suggesting the signal source located in the brain. Previously, patients with insulinoma were found to have spikes and sharp waves,3-6, 9 although the precise mechanism remains unknown.
The EEG changes corresponding to the hypoglycemic event started with irregular high-voltage delta activities, which gradually increased and became continuous without evolution.3, 6, 9 Based on our cases, we stress the utility of LTVEM to both diagnose epilepsy and to reveal the periods of hypoglycemia. EEG findings during insulinoma-induced hypoglycemic attacks can be distinguished from those during focal seizures because of the poorly defined beginning and end of the EEG changes and the absence of evolution. We believe that understanding the typical features of epileptic seizures (i.e., automatism as repetition of nonobjective behavior) is important to exclude epilepsy-mimicking events (i.e., syncope and symptom of increased intracranial pressure) by considering these features as “scripts” of epileptic seizures.10 Based on such knowledge, the utility of LTVEM will be extended. LTVEM also revealed dynamic changes in both semiological and EEG findings corresponding to the immediate recovery from insulinoma-induced hypoglycemia with glucose administration in our two patients. The neurological symptoms disappeared dramatically within 90 s after glucose administration in both our patients, and the generalized high amplitude delta activities on EEG improved within couple of minutes.
Long-term video EEG monitoring can reveal electro-clinical associations of hypoglycemia with high temporal resolution. We hope that this report illustrates the usefulness of LTVEM to clarify the dynamic functional changes within the brain caused by hypoglycemia.
CONFLICT OF INTEREST STATEMENT
None.
REFERENCES
Test yourself
-
How long did it take for the symptoms to improve after intravenous glucose administration?
- Within 3 min
- Within 30 min
- Within 2 h
-
Which EEG finding was characteristic during hypoglycemia in this study?
- Normal EEG
- High voltage generalized slowing without evolution
- High voltage generalized slowing with evolution
-
Which factors made the diagnosis of insulinoma difficult in this study?
- Recurrent neuropsychiatric paroxysmal events
- Normal fasting blood glucose level
- Interictal EEG abnormalities
- All of the above
Answers may be found in the supporting information.