Heart rate and its reduction in chronic heart failure and beyond
Abstract
Heart rate (HR) is associated with cardiovascular outcomes in all the stages of the cardiovascular continuum as well as in patients with pulmonary, cerebrovascular, and renal disease, sepsis, cancer, and erectile dysfunction. In patients with cardiovascular disease, but also in the general population, increased HR represents an important indicator of mortality with each acceleration of HR over 70 b.p.m. increasing the risk. In patients in sinus rhythm with chronic heart failure with reduced ejection fraction (HFrEF), a HR >70 b.p.m. increased the risk of hospitalization, and >75 b.p.m. the risk of cardiovascular death as shown in the Systolic Heart Failure Treatment with the If Inhibitor Ivabradine Trial (SHIFT). Reducing HR with ivabradine by 11 b.p.m. (placebo-controlled) reduced the primary composite endpoint (cardiovascular death and hospitalization for worsening heart failure). Ivabradine was well tolerated showing benefit irrespective of age or diabetes status, and also in the presence of low systolic blood pressure and severe heart failure (SHIFT trial). Therefore, HR qualifies as a modifiable risk factor in heart failure. In patients with stable coronary disease, HR is a risk marker but HR reduction with ivabradine does not improve outcomes. The role of selective HR lowering remains unclear in patients with pulmonary, renal, cerebrovascular, and other diseases, as the potential benefit of interventions on HR has not been explored in these conditions. Future studies should scrutinize if HR reduction improves outcomes, defining HR as a potential risk factor and therapeutic target in other conditions beyond heart failure.
Introduction
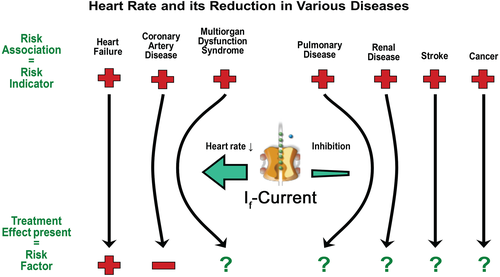
Heart rate (HR) is regulated by the autonomic nervous system and reflects the metabolic demands of the body.1, 2 In turn, coronary blood flow and myocardial oxygen consumption are also affected by high HR. Heart rate is associated with cardiovascular outcomes in all the stages of the cardiovascular continuum, starting with risk factors for cardiovascular events, hypertension, coronary heart disease, and heart failure (HF). To this point, it represents a risk marker. To prove value as a therapeutic target, randomized controlled studies must show improved outcomes by interventions causing HR reduction (Figure 1).3, 4 In patients with cardiovascular disease, especially in high risk patients after cardiovascular events but also in the general population, high HR represents an important indicator of mortality with each acceleration of HR over 70 b.p.m. increasing the risk.4 In patients with impaired left ventricular function after myocardial infarction, the morBidity-Mortality EvAlUaTion of the If inhibitor ivabradine in patients with coronary disease and left ventricULar dysfunction (BEAUTIFUL) trial showed a 34% increased risk for cardiovascular death and a 53% increase in hospitalization at a HR >70 b.p.m. compared with those with lower HR.5 In HF, cardiovascular death is increased from 75 b.p.m., while HF hospitalization risk is elevated from 70 b.p.m.6
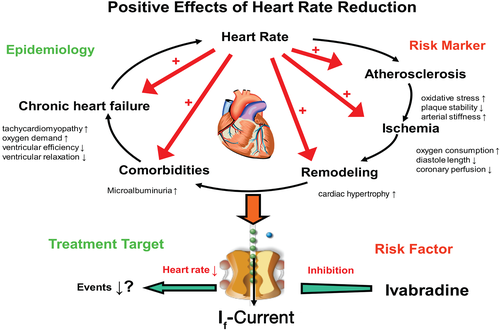
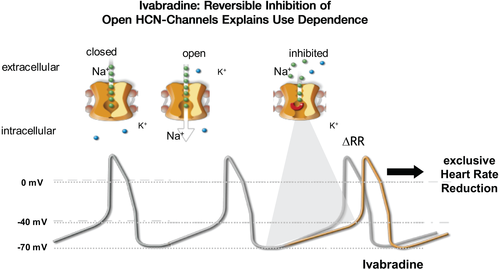
Beta-blockers are recommended in the treatment of chronic HF (CHF).7 Their clinical beneficial effects could be related to reversal of deleterious myocardial effects of catecholamines as well as their pharmacological properties such as a negative chronotropic and inotropic effect reducing myocardial oxygen consumption as well as antiarrhythmic effects. Ivabradine, as a first clinically available drug, reduces HR without other known effects on the cardiovascular system and is an important pharmacological tool to investigate HR affecting other cardiovascular diseases.8, 9 Ivabradine acts on the sinoatrial nodal pacemaker cells and binds to the inner side of the channel pore when it is in the open state and thereby inhibits the hyperpolarization-activated cyclic nucleotide-gated (HCN) channel (Figure 2). HCN is a non-selective cation channel and generates the f-current (f = funny or I(f)) modulating the slope of the spontaneous depolarization in sinoatrial cells that determines resting HR in HF and other chronic conditions, where less evidence has been generated.7-10 Herein, we review current evidence of HR as a risk marker or modifiable risk factor and the therapeutic potential of HR reduction.
Role of heart rate as a risk indicator
Outcome in healthy individuals and in patients with cardiovascular risk factors
The inverse association between HR and survival in the general population and in high risk cardiovascular patients has been demonstrated in epidemiological studies, which included over 100 000 individuals at follow-up of 5–36 years.11-15 The association of HR to outcomes appears to be independent of background risks; however, HR itself is also associated with incident cardiovascular risk factors, such as obesity and diabetes mellitus.16, 17 The association of cardiovascular mortality with transient hypertension and increased HR was observed first in mainly young men who were returning from the First World War.18 Secondary analyses from hypertension trials confirmed the association between high HR at baseline and increased mortality, and between decrease in HR over time and reduced cardiovascular mortality.19, 20 For apparently healthy subjects and stable coronary artery patients the threshold for increased risk is approximately 78–85 b.p.m.12-14
Heart rate and atherosclerosis
Elevated HR is associated with the progression of coronary atherosclerosis3 and an increased incidence of plaque rupture.21 The association of HR with endothelial dysfunction, oxidative stress, and plaque formation with vascular stiffness has been shown in animal models of atherosclerosis.22 In apolipoprotein E (Apo-E) knock-out mice, a reduction in HR with ivabradine has led to a reduction of atherosclerotic lesions and an improvement of endothelial function, providing evidence for a causal relationship.23-25 High resting HR in humans is associated with inflammatory markers for endothelial dysfunction,26, 27 and is related to carotid and aortic stiffness.28 An improvement of endothelial function has not been observed with atenolol in individuals with diabetes mellitus.29 The reason could be an enhanced pulse wave reflection independent of HR reduction and could point toward an adverse effect of beta-blockers on endothelial function.30
Coronary heart disease and myocardial infarction
Patients with coronary artery disease and left ventricular systolic dysfunction at a resting HR of >70 b.p.m. had an increased risk of cardiovascular mortality and coronary vascular events, as shown in the BEAUTIFUL study.5 However, cardiovascular death and vascular events were not significantly reduced by ivabradine.31 Nevertheless, a significant reduction in the need for revascularization and myocardial infarction after ivabradine in the specified subgroup of patients with a resting HR >70 b.p.m. and angina pectoris has been detected.32
The SIGNIFY trial has shown in 19 000 patients with pre-existing stable coronary artery disease that HR reduction with ivabradine did not reduce events and showed a small increase of cardiovascular death in patients treated with diltiazem or verapamil.33, 34 The difference between SIGNIFY33 and BEAUTIFUL31 was the preserved ejection fraction in the former and reduced ejection fraction in the latter population. In impaired ejection fraction with6 and without7 HF, as well as in coronary artery disease without events,12-14 HR is associated with outcomes. The lack of effect of HR reduction shows that HR in the absence of HF or even in normal ejection fraction is a marker of outcomes or a modifier of the long-term course of disease rather than a modifiable risk factor. Patients enrolled in BEAUTIFUL had impaired left ventricular ejection fraction (37% vs. 56% in SIGNIFY) but no HF.5, 31, 32 BEAUTIFUL has been studying an intermediate population.31 Thus, the interpretation is more complex.35
Supportive information comes from other registries and studies. In the REACH registry, treatment with beta-blockers associated with HR reduction in patients on current treatments with coronary artery disease did not show a benefit after low risk myocardial infarction.36 However, after infarction with presumably impaired left ventricular function, endpoints were reduced.36 Thus registry data point in the same direction as studies on HR reduction, although beta-blockers might provide effects beyond HR reduction. One secondary analysis from the ONTARGET study has explored that in patients after stroke or myocardial infarction or diabetes with proven peripheral vascular disease, high HR was connected with an increased risk of stroke and HF hospitalizations, as well as with cardiovascular death (Figure 3). However, the association with myocardial infarction was not significant.37 Therefore, in this analysis, in this specific type of high risk patient, the concept of HR being a risk indicator for myocardial infarctions has been challenged.37 This shows that in stable coronary artery disease, HR is only a risk marker, not a risk factor, because its reduction does not reduce events.

Treatment of angina pectoris through reduction of heart rate
Heart rate is an important determinant of myocardial oxygen demand and coronary blood flow.1 Heart rate acceleration can lead to diastolic dysfunction and to a dysbalance of supply and demand of oxygen and thereby to myocardial ischaemia and subsequent angina and is therefore a clear determinant of symptoms of coronary artery disease. An important target in treating patients with stable angina pectoris is a reduction of HR and, thereby, correcting the imbalance between oxygen supply and demand by influencing both sides of the equation.1 Ivabradine prolongs diastolic time, thereby increasing myocardial perfusion resulting in a reduction of anginal attacks.38 The efficacy of ivabradine on angina symptoms has been shown in beta-blocker-naive patients,39 as well as in patients already treated with atenolol,40 or amlodipine.41 Reduction of HR with ivabradine improved exercise tolerance as measured by time to ST-depression40, 41 and onset of angina pectoris symptoms39-41 leading to its recommendation in the European guidelines for the management of stable coronary artery disease.42 It is interesting to note that despite the convincing antianginal effects HR reduction failed to reduce clinical outcomes in patients with proven coronary artery disease showing that symptom improvement is not related to a reduction of clinical complications. Thus, symptom control and ischaemia reduction reflected by improved angina do not translate into improved outcomes. This conceptually important finding was brought about by the neutral SIGNIFY trial on outcomes. Positive studies are related to symptom control indicating that HR reduction should be used for angina relief and outcome reduction cannot be expected.34, 43
Systolic heart failure
Beta-blocker trials with bisoprolol (CIBIS II44), metoprolol (MERIT-HF45) and carvedilol (COPERNICUS46 and the Carvedilol US programme) demonstrated clinical efficacy by including almost 10 000 patients with stable systolic HF (NYHA class II–IV). Beyond prolonging survival, they reduced hospitalization for worsening of HF, but in the era before intracardiac cardioverter defibrillators were used. The effect of beta-blockers could be due to HR reduction itself,47, 48 but also to other effects derived from interrupting maladaptive beta-signalling pathways. The Systolic Heart failure treatment with the If-inhibitor ivabradine Trial (SHIFT) evaluated the effect of HR reduction by ivabradine in addition to guideline-based treatment on cardiovascular outcomes, symptoms, and quality of life in patients with HF with reduced ejection fraction (HFrEF).49 Ivabradine significantly reduced HR by a placebo-corrected average of 10.9 b.p.m. at 28 days, 9.1 b.p.m. at 1 year, and 8.1 b.p.m. at the end of the study.6 Ivabradine was associated with a lower incidence of the primary endpoint, the composite of cardiovascular death or hospital admission for worsening CHF compared with placebo (Figure 4).49, 50 This result was primarily driven by reduction of hospital admissions for worsening CHF (Figure 5).6, 49 SHIFT has shown that HR is a modifiable risk factor, because through the modification of HR without any other known cardiovascular effects risk was reduced (Figure 6).6, 9 There was a direct association between baseline HR and outcomes.50 After 1 month of treatment, patients with the lowest HR (i.e. 60 b.p.m.) achieved the lowest subsequent event rates at follow-up.50 In the SHIFT subpopulation with HR ≥75 b.p.m., patients had a higher risk of cardiovascular death and hospital admission for worsening HF compared with those with HR <75 b.p.m.50 Ivabradine at HR ≥75 b.p.m. significantly reduced all primary and secondary endpoints including total death and cardiovascular death, in particularly when HR was reduced ≥15 b.p.m.50 More symptomatic bradycardia (5% vs. 1%) and more phosphenes (5% vs. 1%) were observed. There was an increase of 1% in incident atrial fibrillation (AF)49 as it was also observed in SIGNIFY33 and BEAUTIFUL.31
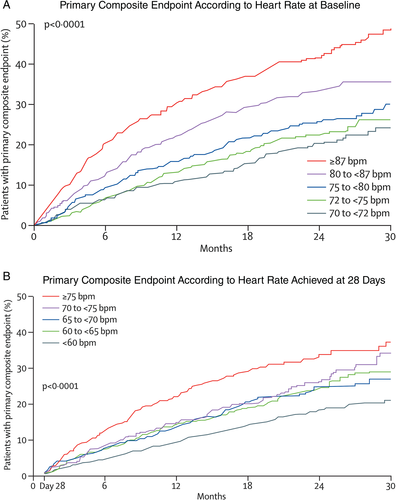
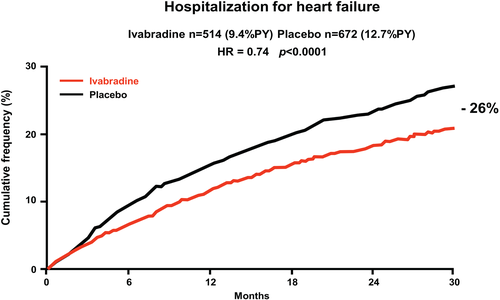
Every hospitalization due to worsening of HF leads to substantially increased mortality of patients with CHF,7 and imposes an enormous burden on health care systems setting the prevention of in-hospital readmissions to high priority in treatment strategies. Patients with HF are particularly at risk for death or rehospitalization in the first weeks after discharge,51, 52 defining this early period as a so-called ‘vulnerable phase’.53 Ivabradine reduced readmissions in this vulnerable phase in patients with CHF after they were hospitalized due to worsening HF.54 Recent data pointed out that a HR >70 b.p.m. is an independent predictor of 1 year risk for readmission in outpatient settings,55 stressing once more the importance of routine evaluation of this easily assessable and low-cost parameter.
Ivabradine in patients with severe HF, often not included or underrepresented in trials, was associated with nominally, non-significant risk reductions for the primary composite endpoint (16%), all-cause death (22%), cardiovascular death (22%), HF death (37%), and hospitalizations for worsening HF (17%).56 This post hoc analysis underscores that HR reduction is beneficial irrespective of disease severity without safety concerns in severe HF and can improve outcomes in patients with severe HF extending to those with sinus tachycardia after heart transplantation57 and ongoing angina.58 In agreement, the beneficial effect of beta-blockers appears to largely depend on their HR risk of properties rather than their dose59, 60 or the blood pressure achieved on treatment.60
Heart rate in heart failure with preserved ejection fraction
It is estimated that the proportion of patients with HF with preserved ejection fraction (HFpEF) ranges from 22 to 73%.7 The association between HR and clinical outcomes in HFpEF patients is less known compared with patients with HFrEF. In a post hoc analysis from the Irbesartan in patients with heart failure and preserved ejection fraction (I-Preserve) trial on 3271 patients, aged >60 years and ejection fraction >45% in sinus rhythm, it has been shown that HR is an independent predictor of adverse clinical outcomes, but there was no relationship between HR and outcomes in 696 patients in AF.61 Similar findings have been observed in a post hoc analysis from the CHART-2 study, where elevated HR at baseline in patients with HFpEF (ejection fraction >50%) and sinus rhythm was associated with increased all-cause mortality and also cardiovascular mortality,62 as well as in a recent meta-analysis.63 Interestingly, the use of beta-blocker therapy was not associated with reduced HF mortality in this subgroup of patients with preserved ejection fraction.61 Whether HR reduction by ivabradine is a potential therapeutic target in HFpEF or not is currently under investigation (Effect of Ivabradine versus placebo on cardiac function, exercise tolerance, and neuroendocrine activation in patients with chronic Heart Failure with Preserved Ejection Fraction, EDIFY, EUDRA-CT No 2012 002742-20).
Heart rate in patients with heart failure and atrial fibrillation
Atrial fibrillation represents the most common arrhythmia in HF patients and is related to increasing the risk of thromboembolic complications, impairing cardiac function and worsening of HF.7 The role of AF to predict outcome is mixed. Some studies found no independent association with mortality64, 65 but with rehospitalization.65 In outpatients, the association with mortality was not robust to adjustment for confounders. According to current evidence, HR in patients with HF and AF does not predict prognosis in terms of survival, as it has been shown that higher HR in these patients was not associated with higher mortality,61-63, 66, 67 irrespective of ejection fraction63 or treatment with beta-blockers,61, 63 except for a HR >120 b.p.m.59 This finding was supported by results of a meta-analysis where use of up-titrated beta-blocker therapy in patients with HFrEF and AF failed to reduce adverse outcomes.67
Heart rate co-morbidities in heart failure
Low blood pressure
Systolic blood pressure (SBP) is an important prognostic factor in patients with CHF. Low SBP (<120 mmHg), which is observed in 15–25% of HF patients, is associated with greater risk for in-hospital and post-discharge mortality, as well as hospitalization for cardiovascular reasons, primarily for worsening HF.68, 69 Low blood pressure may be caused by severely impaired left ventricular function with low cardiac output but may also be due to the use of HF medications, such as beta-blockers, angiotensin II receptor blockers, or angiotensin-converting enzyme (ACE) inhibitors.70 Use of ivabradine in HF patients, as a blood pressure-neutral drug,49 is shown to be beneficial irrespective of SBP values with a good safety profile.70 Furthermore, it has been shown that ivabradine does not influence SBP in the entire SHIFT population49 and in patients with particularly low SBP at baseline.70 Therefore, isolated HR reduction is suitable in the treatment of patients with CHF with low blood pressure and high resting HR.70
Diabetes mellitus
Diabetes mellitus is an important risk factor for the development of HF and increases the risk of all-cause mortality and morbidity, as well as hospitalization in HF patients.7, 71-74 Diabetes mellitus is present in about 30% of patients with HF and is associated with poor outcomes, worsening the prognosis of systolic HF,7, 72 in particular when insulin-treated.74 In a post hoc analysis of the SHIFT trial, it has been shown that ivabradine reduced the primary composite endpoint predominantly by reducing hospitalizations irrespective of diabetes status or use of insulin in diabetes patients.75 Whether improvement of HF outcomes with a potential reduction of neuroendocrine activation is associated with reduced incidence of diabetes or less use of antidiabetics has not been explored yet.
Age
The prevalence of HF increases with age. Ageing influences response to drug treatment in HF patients in many ways. Drugs such as beta-blockers, ACE inhibitors, and mineralocorticoid receptor antagonists76, 77 are less prescribed in eligible patients >75 years, which may be caused by poor tolerance or due to decreased renal function. Furthermore, polypharmacy is common in older HF patients, which in turn can result in more drug-related adverse effects.78 It has been shown that in elderly HF patients, HR after up-titration with beta-blocker therapy, but not the dose of beta-blocker, predicted all-cause mortality risk.79 Elderly patients with HR in the range of 55–64 b.p.m. had lowest mortality.79 The efficacy and safety of ivabradine across the age spectrum by dividing all patients into four groups (<53, <60, 60–69, and >69 years) have been evaluated recently.80 Ivabradine use was associated with a relative risk reduction of the primary endpoint in all age groups, ranging from 38% in the group <53 years to 16% in the group ≥69 years, with no statistical difference by treatment effect of ivabradine in the elderly.80
Heart rate variability, left bundle branch block, and arrhythmias
There was no observed difference in the occurrence of bradycardia and phosphenes across the analysed groups.81 In the Holter substudy of SHIFT (n = 602), there were no severe bradycardias and no clinically relevant pauses on ivabradine in 24 h Holter monitoring documented in any age group.81 Heart rate variability (HRV) measurement provides non-invasive evaluation of autonomic function and can also predict cardiovascular events in patients after a myocardial infarction and in patients with HF.82 In order to investigate if ivabradine affects HRV, and in which way, and to detect rhythm disorders with ivabradine treatment, a substudy of SHIFT with 24 h Holter ECG (every 30 min ECG recordings) was conducted.81 It showed that ivabradine improves HRV in patients with systolic HF, without inducing significant bradycardia, ventricular arrhythmias, or supraventricular arrhythmias.81 In the subgroup of patients with pre-existing left bundle branch block, ivabradine did not produce more bradycardias but a similar efficacy compared with patients without left bundle branch block.83 Nevertheless, in SIGNIFY33, BEAUTIFUL,31 and SHIFT49 there was a small, but significant increase of incident AF.
Septic shock
Myocardial function is commonly impaired in patients with severe septic shock, and multiorgan dysfunction syndrome is associated with poor prognosis.84 Owing to excessive sympathetic activation and depressed parasympathetic control, patients with multiple organ dysfunction syndrome have typically elevated HR.85 It has been reported that in patients in shock the short-acting beta-blocker esmolol resulted in an improvement of haemodynamic parameters and in clinical outcomes associated with its bradycardic effects.86 A longstanding sympathetic activation in concert with therapeutically applied catecholamine-mediated cardiac stimulation has been suggested to be responsible for cardiac depression in sepsis.87 Prospective, randomized trials are needed to properly estimate the applicability of therapeutic HR reduction in patients with critical diseases such as septic or cardiogenic shock.88
Cerebrovascular disease
In mice exposed to chronic stress such as tail suspension, exposure to rats, and intermittent compression, an increase in HR, but not blood pressure, sensitive to ivabradine treatment has been shown to increase the size of experimental stroke89 after experimental occlusion of the middle cerebral artery. Improved endothelial dysfunction, increased capillary density, and reduced oxidative stress have been associated with reduction in stroke size.89 In the PROFESS trial, which included patients after stroke, it has been shown that HR was connected with an increase in cardiovascular death and with an enhancement of cognitive decline after a second stroke.90 Higher HR at baseline in patients with acute ischaemic stroke without AF is associated with increased in-hospital mortality and poor outcome at discharge (modified Rankin Score ≤5), especially in those patients with HR ≥83 b.p.m.91 High mean HR on Holter monitoring after acute ischaemic stroke has been shown to be associated with poorer neurological outcomes (modified Rankin Score ≤5) after 3 months.92 Increased admission HR in acute ischaemic stroke provides additional prediction of early mortality over known predictors such as age and stroke severity.91 A meta-analysis of 5606 patients on stroke units showed that a threshold HR of >86 b.p.m. predicted poor functional and morphological outcome.93 Similar results were recently obtained in patients with intracranial bleeding94 providing a plea for controlled trials95 that should answer the question of whether HR reduction would be beneficial in stroke. Trials exploring effects of HR reduction on outcomes in stroke are needed.
Renal disease
The influence of HR on renal outcome is less known, but it is considered that HR might influence renal risk. It is reported that elevated HR is associated with the prevalence of microalbuminuria in sinus rhythm,96 and AF.97 In the ONTARGET and TRANSCEND trials, elevated resting HR was associated with an increase of renal outcomes like incident microalbuminuria, new onset microalbuminuria, doubling of creatinine, and end-stage renal disease.98 In a post hoc analysis from the SHIFT study, it was demonstrated that increments of 5 b.p.m. of baseline HR were an independent predictor of developing worsening renal function (WRF).99 Ivabradine reduced the primary composite endpoint in patients with and without WRF and treatment with ivabradine itself was not associated with WRF.99 There were no differences in renal function between ivabradine and placebo-treated patients, and, thus, a protective effect of ivabradine on renal function by slowing HR was not observed. The discrepant finding of preventing the progression of HF, which is per se associated with deterioration of renal function, and no protective effect on renal function might be explained by the inclusion criteria with well-preserved renal function in the overall population and in part by a strict definition for WRF used in this study.98, 99
Erectile dysfunction
Erectile dysfunction is a dominant health problem in elderly male and especially in cardiovascular high risk patients.100 It is associated with endothelial dysfunction101 and new onset symptomatic coronary artery disease.102 Erectile function can be experimentally judged from the relaxation of corpora cavernosa. In ivabradine-treated Apo-E knock-out mice, the blunted endothelium-dependent relaxation of corpora cavernosa was improved after HR reduction with ivabradine, which was related to reduction of oxidative stress and an improvement of endothelial function.23 In patients with cardiovascular risk enrolled in the ONTARGET/TRANSCEND trial programme, there was an association of resting HR with erectile function, which was more pronounced than the association with high blood pressure.103
Pulmonary disease
Elevated HR predicts mortality in patients with chronic obstructive pulmonary disease (COPD),104 and is sensitive to cardiopulmonary rehabilitation and endurance training.105 Data from several reports have demonstrated a frequent coexistence of CHF and COPD in a range from 11 to 25%.106, 107 Although COPD patients should be treated with beta-blocker,7 and particularly in those with CHF, physicians often hesitate to use beta-blocker due to concern for deterioration of COPD, which could in part explain poorer outcome in patients with CHF and COPD compared with CHF and non-COPD patients in the SHIFT trial.106
In a post hoc SHIFT analysis, patients were studied according to COPD status. Patients with COPD had higher HR and also worse outcome compared with non-COPD patients.106 Use of ivabradine in COPD patients showed reduction of HR compared with placebo with a good safety profile.106 All endpoints were less frequent with ivabradine compared with placebo in COPD patients.106 One important message of this report is that ivabradine slows HR and can be safely used together with beta-blockers in this high risk population. Heart rate influences prognosis in patients with pulmonary hypertension and, according to case reports, HR reduction with ivabradine delayed the need for parenteral prostanoid therapy.108 Decreasing HR with ivabradine in patients with pulmonary hypertension caused by systemic sclerosis has been shown to be well tolerated and safe.109
Non-adherence effects in patients with chronic heart failure
Non-adherence to evidence-based medications in patients with HF apparently occurred in up to 40% and is related to poor outcome.110 It is associated with increased age,111 polypharmacy,112 depression and cognitive dysfunction in those patients.113 The relationship between clinical outcomes and adherence vs. non-adherence to ivabradine and placebo patients was investigated in a post hoc SHIFT analysis.114 Non-adherence was denoted as premature and permanent stopping of either study drug (ivabradine or placebo), which was observed in 20% of patients.114 Non-adherence was related to the primary composite endpoint with similar results regarding other outcomes. Interestingly, the effect of ivabradine was maintained independently of adherence status in both groups.114 Furthermore, previous HF hospitalizations were associated with developing non-adherence. Thus, non-adherence and worsening of HF are closely connected by showing that one leads to another, creating a vicious circle for HF patients, resulting in poor outcome.
Cancer and heart rate
Associations between cancer mortality and HR in middle-aged men had already been documented in two of three epidemiological studies 35 years ago.115 In 125 513 men (20–95 years) with follow-up of 8 years, a positive relationship between increased HR and cancer mortality has been established regardless of the known risks, in particular cigarette smoking and physical activity.116 After exclusion of the first 2 years of follow-up, increased HR was still associated with cancer mortality, excluding the possibility that increased HR was a reflection of the underlying disease.117 A HR >80 b.p.m. at baseline was associated with 4-fold increased broncho-pulmonary cancer mortality and 2.5-fold increased digestive cancer mortality compared with HR <60 b.p.m.118 The relationship of different HR parameters (resting HR, HR increase during exercise, HR decrease during recovery, and change over 5 years) and cancer mortality was analysed in 6101 asymptomatic men aged 42–53 years with 25 years of follow-up.116 Increased HR was associated with increased cancer mortality, even after exclusion of deaths that occurred during the first 5 years of follow-up.117 A recent report on patients on contemporary cancer therapies118 showed that HR was associated with mortality in patients with colorectal, pancreatic, and non-small cell lung cancer irrespective of other co-morbidities, in particular infections and anaemia, showing that HR ≥75 b.p.m. is an independent predictor of mortality in these patients.118 Heart rate reduction could be useful to ameliorate the toxic effects of cancer drugs and to improve quality of life. The latter effect has been shown in patients with CHF.119 The potential of this approach has been emphasized in a retrospective analysis on renin–angiotensin blockers providing protective effects in cancer patients.120, 121 Furthermore, beta-blockers appear to prolong life in cancer patients,122 which could be related to protective cardiovascular effects, or effects on cancer recurrence123 or secondary cancer formation.124
This finding represents a valid basis for consideration that cardiovascular intervention as a HR reduction might have a beneficial effect on survival, thus determining HR as potential modifiable risk factor in cancer patients and the role of its reduction as a supportive care concept.125 The role of cardioprotective treatment has to be scrutinized in future trials.
Summary and future perspectives
With ivabradine as the first approved HR-lowering drug with no other known cardiovascular effects, SHIFT provided support for the concept that in HF, HR is a modifiable risk factor independent of the use or dose of beta-blockers.126 In coronary artery disease with normal ejection fraction, there is no role for ivabradine to improve outcomes. Presently, resting HR remains only a risk marker also in many other conditions (Figure 6). Nevertheless, the HR–risk association suggests to test the concept of HR reduction in other conditions like acute illness, including cardiogenic shock, or chronic conditions such as pulmonary disease, erectile dysfunction, provided that patients are stable enough to tolerate HR reduction. Since the latter conditions are frequent co-morbidities in CHF, it is interesting to note that HR reduction reduces outcomes in patients with different co-morbidity loads.127 Therefore, it is important to generate trials to study HR reduction in conditions beyond HF.
Conflict of interest: A.N.V. and D.V. have no conflicts of interest to declare. J.B., M.K., M.C., and M.B. received honoraria for scientific advice and lecture fees from Servier. J.B., M.K., K.S., and M.B. were members of the Executive Board of the SHIFT trial. M.L. received honoraria and lecture fee from Servier.