Decongestion in acute heart failure
Abstract
Congestion is a major reason for hospitalization in acute heart failure (HF). Therapeutic strategies to manage congestion include diuretics, vasodilators, ultrafiltration, vasopressin antagonists, mineralocorticoid receptor antagonists, and potentially also novel therapies such as gut sequesterants and serelaxin. Uncertainty exists with respect to the appropriate decongestion strategy for an individual patient. In this review, we summarize the benefit and risk profiles for these decongestion strategies and provide guidance on selecting an appropriate approach for different patients. An evidence-based initial approach to congestion management involves high-dose i.v. diuretics with addition of vasodilators for dyspnoea relief if blood pressure allows. To enhance diuresis or overcome diuretic resistance, options include dual nephron blockade with thiazide diuretics or natriuretic doses of mineralocorticoid receptor antagonists. Vasopressin antagonists may improve aquaresis and relieve dyspnoea. If diuretic strategies are unsuccessful, then ultrafiltration may be considered. Ultrafiltration should be used with caution in the setting of worsening renal function. This review is based on discussions among scientists, clinical trialists, and regulatory representatives at the 9th Global Cardio Vascular Clinical Trialists Forum in Paris, France, from 30 November to 1 December 2012.
Introduction
Heart failure (HF) is a major and increasing public health problem worldwide.1-3 The primary reason for acute HF (AHF) hospitalization is congestion manifested by dyspnoea, oedema, and fatigue due to elevated filling pressures.4-6 Despite inpatient treatment targeting decongestion with diuretics, many patients are discharged without weight loss and with persistent signs of congestion.7, 8 For instance, in an international AHF trial, persistent congestion was present at discharge in more than a quarter of patients.9 Baseline congestion and residual congestion at discharge are associated with increased rehospitalization and mortality, and successful decongestion is a major goal of AHF management.9-11
Uncertainty exists with respect to the pathogenesis of congestion and how best to treat congestion prior to discharge.12, 13 In addition to diuretics, strategies to treat congestion include vasodilators, ultrafiltration (UF), vasopressin antagonists, and mineralocorticoid receptor antagonists (MRAs). Serelaxin and gut sequesterants may also be used for decongestion in the future. Here, we summarize the benefit and risk profiles for these therapies and provide guidance on selecting an appropriate approach for different patients. This review is based on discussions among scientists, clinical trialists, and regulatory representatives at the 9th Global CardioVascular Clinical Trialists Forum in Paris, France, from 30 November to 1 December 2012.
Pathophysiology of congestion in acute heart failure
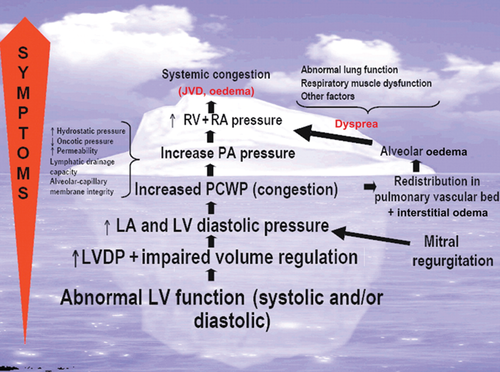
Congestion is defined as a high LV end-diastolic pressure associated with signs and symptoms such as dyspnoea, rales, and oedema (Figure 1).13 Recent data also demonstrate the importance of elevation in right-sided pressures as characterized by inferior vena cava dilation,14 which result in the characteristic signs and symptoms of hepatic and renal congestion.
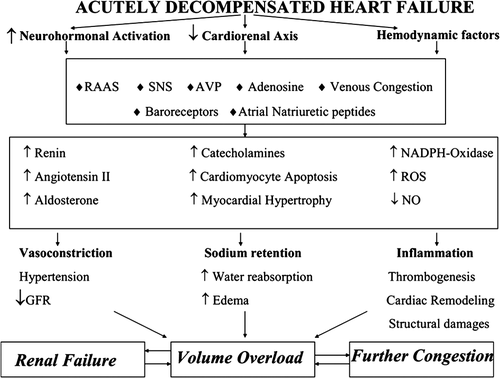
At present, the underlying mechanisms of congestion in AHF are poorly understood. The traditional paradigm assumes that haemodynamic abnormalities related to reduced cardiac output and activation of the renin–angiotensin–aldosterone system (RAAS) are the primary pathophysiological drivers in AHF. Underlying cardiac dysfunction is exacerbated by coronary ischaemia, hypertension, arrhythmia, infection, or medical/dietary non-adherence, with increased fluid retention. However, in many patients, a specific precipitating factor cannot be identified, and early symptoms of congestion occur without significant weight gain.15 Thus, there is increasing recognition that fluid redistribution may contribute to AHF. For instance, extracellular fluid volume can shift from the splanchnic veins into the effective circulating blood volume during AHF via autonomic mechanisms.16 Contemporary data also support a role for inflammation, endothelial cell activation, prothrombotic changes, and abnormalities in arginine vasopressin (AVP) and adenosine signalling (Figure 2).17 For instance, Colombo and colleagues recently demonstrated that peripheral venous congestion caused the release of inflammatory mediators and changes in endothelial cell response in an experimental model.18 The contribution of these mechanisms in different AHF patients varies.19 For instance, elderly females with preserved EF tend to present more often with rapidly progressive pulmonary oedema in the setting of hypertension related to mechanisms of reduced arterial compliance and venous capacitance.20-22 Other patients present with a distinct phenotype characterized by the insidious onset of dyspnoea, and peripheral oedema with evidence of hepatic and renal dysfunction due, in part, to RAAS activation, inflammation, and progressive cardiorenal syndrome.17, 23-25 Regardless of the specific underlying mechanisms for an individual patient, congestion contributes to HF progression through further neurohormonal activation, LV geometric changes, pulmonary hypertension, right ventricular (RV) dysfunction, and adverse cardiorenal changes.26-28
Assessment of congestion and decongestion
The pattern of congestion in AHF varies, but data suggest that 89% of patients present with dyspnoea; rales and peripheral oedema are present in 68% and 66%, respectively.4 While there is not currently a standardized definition of adequate decongestion, clinical trials have used the following criteria: jugular venous distension (JVD) <8 cm of water, no more than trace peripheral oedema, and the absence of orthopnoea.29 These criteria have been simplified into an ‘orthoedema’ congestion score based on the presence of orthopnoea (≥2 pillow = 2, <2 pillows = 0) and peripheral oedema (trace = 0, moderate = 1, severe = 2) with the components added to classify congestion as mild (score 0–1), moderate (2), and severe (3–4).30 A post-hoc analysis of the DOSE-HF and CARRESS-HF trials of AHF patients with congestion (and cardiorenal syndrome in the case of CARRESS-HF) found that baseline orthoedema was moderate in 22% of patients and severe in 62%.31 Following aggressive inpatient therapy targeting decongestion, more than one-third of patients (35%) had persistent moderate to severe congestion at discharge. Higher orthoedema scores at admission and discharge were both associated with increased risk for 60-day death or HF hospitalization.
These recent studies in combination with other data in AHF patients demonstrate that even with severe haemodynamic congestion, physical signs including rales, oedema, and JVD may have limited sensitivity and specificity.32 Moreover, markers of decongestion such as weight and fluid loss have a poor correlation with dyspnoea relief.33 Given the difficulty in accurately assessing congestion by exam, biomarkers and other novel approaches may help clinicians to quantify congestion. For example, recent data highlight a role for the use of bioimpedance techniques in evaluating volume status.34 Natriuretic peptides are the most commonly used biomarker of volume status. Rather than using absolute thresholds of natriuretic peptides to signify congestion, the value of using ‘wet’ and ‘optivolaemic’ values for individual patients has been demonstrated.35 In other words, clinicians may consider obtaining serial values (e.g. on admission for AHF with congestion, prior to discharge from AHF following decongestion, and during a period of euvolaemia as an outpatient) in order to inform future clinical evaluation of an individual patient's congestion status. Haemoconcentration during hospitalization, as characterized by increases in haemoglobin or haematocrit, albumin, and total protein, represents another marker of decongestion. Haemoconcentration during AHF hospitalization has been associated with improved 180-day survival36 despite an association with worsening renal function (WRF).37 Recent evidence has also highlighted the importance of the timing of haemoconcentration.38 Only haemoconcentration that occurs later during hospitalization is associated with improved outcomes, which suggests the importance of sustained decongestion. Altogether, the assessment of volume status is of paramount importance in order to tailor therapies to an individual patient's needs. In contemporary clinical practice, the assessment of volume status is largely based on data from clinical examination and laboratory biomarker profiles. Future work will better define the role of novel techniques to monitor volume status such as bioimpedence and implantable monitors.
Decongestion strategies
Loop diuretics
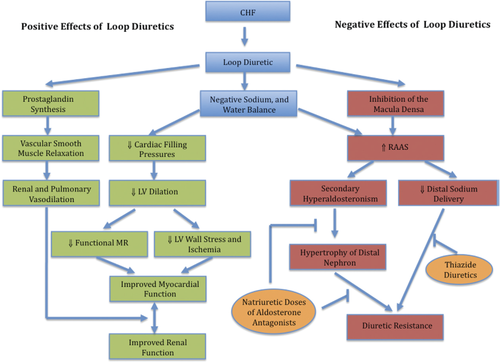
Historically, loop diuretics (e.g. furosemide and torsemide) have been the cornerstone of decongestive therapy.39 Loop diuretics inhibit the renal Na+/2Cl–/K+ co-transporter, resulting in natriuresis and diuresis. In HF patients, the diuretic dose–response curve shifts downward and to the right, such that a higher dose is required to achieve the effect. Loop diuretics generally improve dyspnoea and decrease ventricular filling pressures in AHF (Figure 3). Several small studies of torsemide vs. furosemide40-42 and a recent meta-analysis43 suggest a decrease in HF morbidity with torsemide compared with furosemide. However, a prospective large-scale trial is needed to support these findings.
The DOSE trial (Diuretic Optimization Strategies Evaluation) is the largest randomized AHF trial to evaluate diuretic strategies.44 DOSE randomized 308 AHF patients to i.v. furosemide given as boluses or continuous infusion and to either a low-dose (i.v. dose numerically equivalent to the patient's oral dose) or a high-dose (2.5 times the oral dose given intravenously) strategy. There was no significant difference in the co-primary endpoints of global assessment of symptoms or change in serum creatinine over 72 h with any of these strategies. However, patients randomized to the higher dose strategy had more favourable outcomes for the secondary measures of dyspnoea relief, change in weight, and fluid loss. However, as noted above, more than one-third of patients in a combined analysis of the DOSE and CARRESS trials had persistent congestion at discharge despite therapy targeting decongestion in the clinical trial setting.31 Thus, despite the efficacy of loop diuretics for dyspnoea relief, data suggest limitations related to successful decongestion.
Loop diuretic use is also balanced by limitations of diuretic resistance, neurohormonal activation, and WRF.39 Diuretic resistance occurs when these agents fail to control volume status adequately despite appropriate dose escalation. Mechanisms of diuretic resistance include the ‘braking phenomenon’, ‘rebound’ effect, and hyperaldosteronism. The ‘braking phenomenon’ occurs when long-term diuretic use results in a reduced natriuretic response due, in part, to nephron adaptations.45 The ‘rebound’ effect involves post-diuretic sodium retention typically in the setting of inadequate dosing frequency and insufficient sodium restriction.46 Sequential nephron blockade with thiazide-type diuretics may be used in combination with loop diuretics to augment diuresis.47 However, their use has been associated with increased arrhythmia risk due to hypokalaemia.48
Observational studies have shown associations between high-dose loop diuretics and adverse outcomes.49-51 However, these studies are confounded, since patients receiving higher doses of diuretics tend to have greater disease severity and/or co-morbidity. Nonetheless, animal studies have shown that treatment with furosemide results in progression of LV systolic dysfunction.52 Potential mechanisms for worse outcomes with loop diuretics include RAAS activation, electrolyte disturbances, and WRF.
Loop diuretics may cause RAAS activation. Studies supporting this concept, however, generally pre-date contemporary HF pharmacotherapy. A retrospective study of the SOLVD trial demonstrated that plasma renin activity (PRA) was significantly elevated in HF patients receiving diuretics compared with those not receiving diuretics.53 In another study, acute dosing of i.v. furosemide resulted in rapid PRA elevation in HF patients treated chronically with digoxin, and this was associated with systemic vasoconstriction.54
The association between higher diuretic dosing and WRF has been of particular interest given that WRF is associated with worse outcome.49, 55 However, recent data have suggested that transient WRF during AHF therapy may not affect post-discharge outcomes.37, 56 For instance, in the DOSE trial, higher dose diuretics were superior to lower dose diuretics for dyspnoea relief and fluid loss at the cost of transient WRF that did not appear to have long-term consequences.44 Given that persistent congestion is associated with WRF57 and adverse events, transient WRF may be a reasonable trade-off for decongestion. For instance, a recent analysis by Metra et al. demonstrated that WRF was not associated with worse outcomes, but that WRF in the context of persistent congestion was an independent predictor of post-discharge morbidity and mortality.58
Vasodilators
Current guidelines indicate that if symptomatic hypotension is absent during hospitalization for AHF, i.v. vasodilators may be considered as an adjuvant to diuretic therapy for dyspnoea relief.1, 3 There are currently no data to support improved outcomes in AHF patients treated with vasodilators. Overall, the data support modest beneficial effects on dyspnoea relief and haemodynamics (e.g. central venous pressure and pulmonary capillary wedge pressure), but further details related to effects on peripheral oedema, net fluid loss, and weight loss are limited. Thus, further characterization of the utility of these agents to decongest patients adequately based on the metrics above is not possible.
Intravenous nitroglycerin is primarily a venodilator that lowers preload and may help reduce pulmonary congestion.59 However, tachyphylaxis to nitroglycerin may develop within hours despite dose escalation.60 Nitroprusside is a balanced venodilator and arteriodilator with effects on the pulmonary vasculature.61 Efficacy data with nitroprusside in AHF patients are limited and largely confined to post-myocardial infarction LV dysfunction.62, 63 Nitroprusside use is typically confined to an intensive care setting with invasive haemodynamic monitoring due to the potential for marked hypotension.1
Nesiritide reduces ventricular filling pressures, yet studies demonstrated variable effects on dyspnoea relief. A randomized trial of nesiritide vs. placebo in 127 AHF patients demonstrated that nesiritide more rapidly reduced dyspnoea compared with diuretics alone.64 The VMAC study investigated the use of nesiritide vs. nitroglycerin vs. placebo in 489 AHF patients.65 Nesiritide resulted in significant improvements in wedge pressure compared with nitroglycerin and placebo. However, there was no difference between nesiritide and nitroglycerin with respect to dyspnoea benefits. ASCEND-HF demonstrated that nesiritide compared with placebo had a modest non-significant impact on dyspnoea at the cost of more hypotension.66 Nesiritide did not affect post-discharge outcomes. A recent subgroup analysis also showed that nesiritide did not increase urine output compared with standard therapy.67 Thus, routine use of nesiritide has not been recommended in the broad AHF population.
Novel natriuretic peptides with vasodilatory effects, such as ularitide, are being investigated in acute HF patients. Two double-blind placebo-controlled proof-of-concept studies demonstrated haemodynamic and symptom benefits with ularitide.68 An ongoing phase III trial of ularitide is investigating a potential role for ularitide added to standard therapy in acute HF (NCT01661634).
Ultrafiltration
Ultrafiltration involves removal of plasma water across a semi-permeable membrane in response to a transmembrane pressure gradient.39 If fluid removal does not exceed the interstitial fluid mobilization rate, then intravascular volume can be preserved, potentially avoiding RAAS activation and WRF.39 However, most studies investigating RAAS activation with UF pre-dated routine use of beta-blockers and ACE inhibitors.
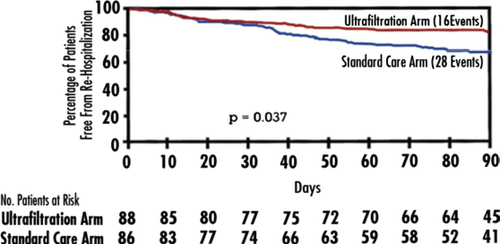
The UNLOAD trial was the first large-scale trial of UF in AHF.69 This unblinded trial randomized 200 patients with AHF to either UF or loop diuretics as the primary decongestive therapy within 24 h of hospitalization. The duration and rate of UF were decided by the treating physicians. The co-primary endpoints were weight loss and dyspnoea relief at 48 h. The UF group had greater weight loss (mean of 5.0 kg vs. 3.1 kg, P = 0.001), but there was no difference in dyspnoea relief. There was significantly less hypokalaemia with UF, and other safety parameters (including serum creatinine change) were similar in the two study arms. Net fluid loss at 48 h (a secondary endpoint) was also greater in the UF arm (mean of 4.6 L vs. 3.3 L, P = 0.001). However, BNP improvements were similar with UF and usual care. There was a significant decrease in the secondary endpoint of rehospitalization for HF at 90 days with UF compared with diuretic therapy (Figure 4). These findings are hypothesis-generating given the small number of events, short follow-up, and unblinded study design.
CARRESS-HF was a randomized trial of UF vs. stepped pharmacological therapy in 188 AHF patients with WRF and persistent volume overload.29 UF was performed at a fluid removal rate of 200 mL/h. Stepped pharmacological therapy involved adjustments in loop diuretic doses as well as i.v. vasodilators and inotropic agents as a function of the signs and symptoms of congestion, urine output, blood pressure, EF, and the presence or absence of RV failure at 48 h. CARRESS-HF tested UF in a different patient population (i.e. cardiorenal syndrome type 1) compared with UNLOAD (i.e. routine AHF). UF was inferior for the primary endpoint of the bivariate change in the serum creatinine and body weight at 96 h due to an increase in creatinine. Whether such a rise in serum creatinine represents desired effects of haemoconcentration or undesired WRF with subsequent outcome consequences is unknown. There was no significant between-group difference in weight loss or natriuretic peptides, and a higher percentage of patients in the UF group had a serious adverse event. Overall, successful decongestion (JVD <8 cm of water, ≤peripheral oedema, no orthopnoea) occurred in only ∼10% of patients at 96 h in both treatment arms. These data further demonstrate that substantial weight and fluid loss are not adequate surrogates of decongestion. UF use must also be balanced by limitations related to the technology. UF involves a disposable, single-use extracorporeal blood circuit. A cost–consequences analysis found that despite a potential reduction in rehospitalization with UF, it was unlikely to result in cost savings from a societal level.70 Despite the current ability to perform UF through peripheral i.v. access, the lumens must provide 10–40 mL/min of blood flow such that patients are exposed to increased risk related to vascular access complications. Full anticoagulation is required. In CARRESS-HF, patients receiving UF had a high adverse event rate due to catheter- or anticoagulation-related complications (e.g. 2% catheter site haemorrhage, 9% sepsis, bacteraemia, or cellulitis, and 7% gastrointestinal haemorrhage). Provider experience and nursing support are additional concerns with the routine use of UF.
Current guidelines indicate that if diuretic strategies are unsuccessful, UF may be considered.1, 3 The results of the ongoing Study of Heart Failure Hospitalizations After Aquapheresis Therapy Compared to Intravenous Diuretic Treatment (AVOID-HF, ClinicalTrials.gov Identifier: NCT01474200) are eagerly awaited. This trial is to enrol 810 patients admitted with AHF, and randomized to either UF or i.v. loop diuretics. The primary outcome is time to first HF event within 90 days after discharge from the index hospitalization.
Vasopressin antagonists
Inappropriate elevation of AVP in HF results in water retention with resultant congestive symptoms and electrolyte abnormalities.71 Vasopressin antagonists such as tolvaptan have been developed to block the action of AVP at the V2 receptor in renal tubules to promote aquaresis. V2-specific antagonists have the potential to increase AVP levels with consequent stimulation of V1 receptors involved in peripheral vasoconstriction.
EVEREST was a large trial comparing tolvaptan and placebo, which tested the hypothesis that adding an aquaretic agent to conventional diuretics in HF patients would improve symptoms and outcomes.72, 73 EVEREST enrolled 4133 patients admitted with AHF with EF <40% and ≥2 signs/symptoms of fluid overload. The primary short-term endpoint was a composite of patient-assessed global clinical status and weight at day 7 or discharge. The long-term co-primary endpoints were mortality and cardiovascular mortality/HF hospitalization. Tolvaptan showed greater improvement compared with placebo for weight change, but long-term outcomes were similar.
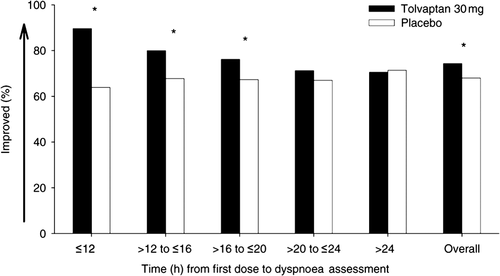
In EVEREST, tolvaptan in addition to standard diuretic therapy improved many, but not all, signs and symptoms related to congestion. Tolvaptan improved dyspnoea, body weight, rales, JVD, and orthopnoea over the first several days of hospitalization despite less use of diuretics. However, global clinical status, a component of the primary outcome, was not improved. The dyspnoea benefits were greatest within 12 h after the initial dose, and persisted up to 20 h74 (Figure 5). Tolvaptan's benefits on dyspnoea relief and weight reduction were more marked in those patients with hyponatraemia.75 In the small cohort of patients with severe hyponatraemia (sodium <130 mEq/L), tolvaptan was associated with reduced cardiovascular morbidity and mortality. Overall, serious adverse events including renal dysfunction, hypotension, and electrolyte abnormalities were similar with tolvaptan. These data have suggested that tolvaptan may be a useful adjunct to treating congestion early during hospitalization in patients with AHF. Tolvaptan is not specifically approved for treating congestion but rather is approved for the treatment of severe hyponatraemia such as that seen in heart failure. At present, at least two placebo-controlled trials are exploring decongestion benefits with tolvaptan in AHF (NCT01644331 and NCT01584557).
The Food and Drug Administration (FDA) recently announced label changes for tolvaptan, which indicate that it should not be used for longer than 30 days and should not be used in patients with underlying liver disease. These changes were made after three cases of suspected liver injury with higher doses and prolonged use of tolvaptan were identified in the TEMPO study of patients with Polycystic Kidney Disease.76
Natriuretic doses of mineralocorticoid receptor antagonists
Chronic therapy with an MRA, either spironolactone 25 mg daily or eplerenone 50 mg daily, is recommended in patients with NYHA class II–IV symptoms and an LVEF ≤35%.1 A post-hoc analysis of the EPHESUS study data suggested that eplerenone produced a mild short-term diuretic effect associated with better outcomes.77 However, the benefits at these doses seem to be due largely to cardioprotective effects rather than sodium handling.78 The current evidence-based MRA doses in HF are much lower than the natriuretic doses of up to 400 mg/day used in cirrhotic patients.79 It has been suggested that natriuretic doses could provide additional decongestion benefits beyond loop diuretics in AHF.79
In both cirrhosis and HF, hyperaldosteronism plays a major role in the development of congestive symptoms and contributes to diuretic resistance.39 The pathophysiology involves a failure to escape from the sodium-retaining effect of aldosterone. Hyperaldosteronism increases the major aldosterone-sensitive renal tubule channels.80 Therefore, sodium that is not reabsorbed in the loop of Henle due to the effects of loop diuretics may be reabsorbed in the distal nephron via aldosterone-related mechanisms. Natriuretic MRA doses in addition to loop diuretics may cause significant natriuresis even in the context of presumed diuretic resistance. To date, natriuretic MRA doses have not been empirically evaluated in an adequately powered HF study. However, several small studies have suggested potential benefits.81-84
The use of natriuretic MRA doses must be balanced with concerns of hyperkalaemia. A recent retrospective study examined the safety of natriuretic doses of spironolactone in HF patients.85 During a total of 738 patient-weeks, there was no significant increase in mean serum potassium or creatinine with natriuretic MRA doses. In contrast, a post-hoc analysis of the EPHESUS data suggested that eplerenone produced a mild short-term potassium-sparing effect, which was associated with better outcomes.77 Prospective, controlled studies are needed to explore the benefits related to decongestion.
Gut sequesterants
Since many patients with AHF have chronic kidney disease (CKD) or WRF, it has been suggested that alternative, non-invasive strategies to remove fluid should be explored.86 In particular, agents are needed that assist with fluid removal without RAAS activation and hyperkalaemia.
An acrylic polymer called cross-linked polyelectrolyte (CLP) removes sodium, potassium, and fluid from the gastrointestinal tract with elimination in the faeces. A double-blind randomized trial of CLP vs. placebo for 8 weeks was performed in 113 HF patients with CKD.87 There was no between-group difference in the primary endpoint of serum potassium over time, but the CLP-treated patients had greater weight loss early in the study as well as improved symptoms and quality of life. There was a trend toward less dyspnoea and lower natriuretic peptide levels with CLP. The primary concern was that four deaths occurred in the CLP arm. While this was a small study and investigators did not feel the deaths were attributable to study drug, these findings highlight the need for caution in subsequent studies. Future studies will need to explore whether these potential benefits in weight loss, dyspnoea relief, and natriuretic peptide levels translate into improved decongestion in the setting of larger, controlled clinical trials.
Serelaxin
Serelaxin is recombinant human relaxin-2 peptide, which regulates maternal adaptations in pregnancy.88 Serelaxin has potential benefits for decongestion given effects on arterial compliance, cardiac output, and renal blood flow.
The RELAX-AHF trial was a phase III placebo-controlled trial of serelaxin in 1161 AHF patients with co-primary endpoints of dyspnoea improvement.89 A 48-h infusion of serelaxin resulted in an improvement in the visual analogue scale area under the curve from baseline to 5 days, but not dyspnoea improvement by Likert scale. There were no between-group differences for secondary composite endpoints including death or hospitalization. However, all-cause mortality and cardiovascular mortality at 180 days were significantly lower with serelaxin [hazard ratio (HR) 0.63, 95% confidence interval (CI) 0.43–0.93; and HR 0.63, 95% CI, 0.41–0.96, respectively]. Benefits with serelaxin were also observed for rates of worsening HF, length of stay, and prognostic biomarkers.90 Serelaxin may offer benefits on congestion as evidence by effects on dyspnoea relief and natriuretic peptides as well as the prevention of worsening HF, but further study is required. The ongoing RELAX-2 study is powered (target n = 6375) for the primary endpoint of cardiovascular mortality through 180 days (ClinicalTrials.gov identifier: NCT01870778). A recent randomized study investigated the renal haemodynamic effects of a 24-h infusion of serelaxin vs. placebo in 65 patients with chronic HF.91 Serelaxin-treated patients demonstrated a rise in renal plasma flow during the infusion, but there was no between-group difference in glomerular filtration rate. There were also no significant differences for changes in systolic blood pressure (SBP) or sodium excretion. Thus, ongoing study is required to investigate the mechanisms by which serelaxin may improve symptoms and outcomes in AHF.
| Strategy | Strengths | Limitations | Key references |
|---|---|---|---|
| Strategies routinely used for decongestion | |||
| Loop diuretics | •Ease of clinical use | •Diuretic resistance | DOSE-AHF44 |
| •Non-invasive strategy | •Possible neurohormonal activation | ||
| •Operator experience is robust | •Side effects including electrolyte disturbances | Felker and Mentz39 | |
| •Benefits on dyspnoea relief | •Association with worsening renal function | ||
| •Potential limitations to reaching successful decongestion | Hasselblad et al.51 | ||
| Metra et al.58 | |||
| Intravenous vasodilators | •Dyspnoea benefits (modest) | •Potential for hypotension | VMAC65 |
| •Haemodynamic benefits (CVP, PCWP) | •Require close monitoring ± ICU | ||
| •Blood pressure reduction may be beneficial in certain circumstances | •Tachyphylaxis (nitroglycerin) | ASCEND66 | |
| •Uncertain decongestion benefits | |||
| Ultrafiltration | •Fluid removal possible in the setting of diuretic resistance and renal insufficiency | •Potential for worsening renal function in the setting of cardiorenal syndrome (e.g. CARRESS Trial) | UNLOAD69 |
| •Potential for reduced RAAS activation | •Vascular access complications | ||
| •Potential benefits on weight loss (variable effects in different trials) | •Anticoagulation is required | CARRESS29 | |
| •Potential for reduced electrolyte disturbances | •Provider experience may be less | ||
| •Nursing support/training required | |||
| •Potential limitations to reaching successful decongestion | |||
| •Potential cost considerations | |||
| Strategies in development or under investigation for decongestion | |||
| Vasopressin antagonists | •Dyspnoea relief (particularly early during AHF) | •Benefit appears to be greatest in those with hyponatraemia | Konstam et al.72 |
| •Benefits for body weight, rales, JVD, and orthopnoea | •Adverse effect profile includes neurological changes and hepatotoxicity (in the context of prolonged use) | ||
| •May allow less loop diuretic use | •Cost considerations | Pang et al.74 | |
| Mineralocorticoid receptor antagonists (natriuretic doses) | •Potential additive benefits to loop diuretic on natriuresis | •Hyperkalaemia | Bansal et al.79 |
| •Potential strategy to overcome diuretic resistance | •Empiric data regarding decongestion benefits are limited | ||
| •Provider experience with high dose may be limited | |||
| Gut sequesterants | •Potential benefits on weight loss | •Current empiric evidence on these agents is limited | Costanzo et al.87 |
| •Possible benefits on dyspnoea relief and natriuretic peptide levels | •Concerns related to mortality in early phase studies | ||
| •May allow fluid removal without RAAS activation and potassium abnormalities | •Cost considerations | ||
| Serelaxin | •Dyspnoea relief | •Empiric data regarding decongestion benefits are limited | Teerlink et al.89 |
| •Benefits on natriuretic peptide levels | •Provider experience is less | ||
| •Reduced incidence of worsening HF | •Potential cost considerations | Metra et al.90 | |
| •Potential mortality benefit | |||
- AHF, acute heart failure; CVP, central venous pressure; HF, heart failure; ICU, intensive care unit; JVD, jugular venous distension; RAAS, renin–angiotensin–aldosterone system.
Other novel agents under investigation
In addition to gut sequesterants, serelaxin, and novel natriuretic peptides such as ularitide, there are a number of additional AHF therapeutic agents with potential decongestion benefits that are currently under investigation. For instance, these agents include luso-inotropic agents (istraoxime), cardiac myosin activators (omecamtiv mecarbil), and oral soluble guanylate cyclase stimulators, which have recently been reviewed.17, 68 Further studies will be needed to clarify the utility of these and other agents with regard to decongestion.
Selecting an appropriate decongestion approach for different patients
Figure 6 outlines an approach to managing congestion in AHF patients. An evidence-based initial approach to congestion management involves high-dose i.v. diuretics by either i.v. bolus or continuous infusion.44 Current guidelines indicate that the optimal dose of i.v. furosemide is uncertain,3 but, based on DOSE-AHF, an initial i.v. furosemide dose of 2.5 times the patient's home oral diuretic dose generally results in substantial diuresis and dyspnoea relief. Diuretic dosing can be repeated as needed. Baseline electrolyte abnormalities or renal dysfunction should lead to consideration of other therapies including haemodiafiltration. In the subgroup of AHF patients with elevation in SBP, the use of vasodilators may be added for dyspnoea relief. In order to augment diuresis or to overcome issues related to diuretic resistance, natriuretic MRA doses may be used as long as the patient does not have significant renal dysfunction or hyperkalaemia. Alternative strategies to augment decongestion include the use of thiazide-type diuretics39 or potentially also vasopressin antagonists (particularly in the setting of hyponatraemia).
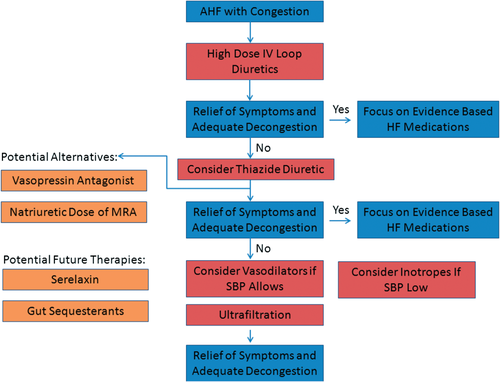
In the setting of WRF, the CARRESS trial provided hypothesis-generating evidence to support stepped pharmacological therapy to treat congestion.29 For the first 2 days, i.v. diuretics were adjusted (± a thiazide diuretic) to manage congestion and maintain a urine output of 3–5 L/day. If after 48 h, urine output was inadequate, the use of i.v. vasodilators or inotropic agents was considered. The specific protocols29 were dependent upon a patient's SBP, LVEF, and the presence or absence of RV failure. For instance, if SBP was <110 mmHg and the patient had a reduced LVEF or RV failure, then dopamine or dobutamine could be considered. If the patient's SBP was >120 mmHg and he/she had severe symptoms, then nitroglycerin or nesiritide was considered. If urine output was still inadequate after 72 h, then there was consideration for haemodynamic-guided i.v. therapy, or crossover to UF or dialysis. Importantly, this stepped pharmacological care algorithm has only been compared with UF, and potential advantages over usual care have not been empirically demonstrated.
If all diuretic strategies including consideration of stepped pharmacological therapy are unsuccessful, then UF may be considered. However, the results of CARRESS indicate that UF should be used with caution in the setting of WRF. Alternatively, in AHF due to AF and when i.v. inotropes are not feasible, digoxin may be considered. In the future, options for decongestion therapy might also include serelaxin and/or gut sequesterants.
Conclusion
Diuretics have been the mainstay of decongestion therapy. However, the approach to decongestion can be individualized based on a patient's initial diuretic response, co-morbidity burden, electrolyte abnormalities, and haemodynamic profile. Different options may include natriuretic MRA doses, vasodilators, and/or a stepped pharmacological approach of diuretic up-titration and inotropes. At the present time, the use of UF should be confined to patients that fail to respond to diuretic-based strategies. In the future, gut sequesterants and serelaxin may serve as additional or alternative therapies. Although many unanswered questions remain about the best approach for using these therapies, ongoing trials will inform the future treatment of congestion.
Funding
The National Institute of General Medical Sciences [grant no. T32GM086330 R.J.M.]; the European Commission [grant FP7-242209-BIOSTAT-CHF to A.A.V.].
Conflict of interest: A.A.V. received consultancy fees and/or research grants from: Alere, Amgen, Anexon, Bayer, Boehringer Ingelheim, Cardio3Biosciences, Celladon, Merck, Novartis, Servier, Torrent, and Vifor Pharma. G.F.C. served on advisory boards for MSD and Bayer. S.D.A is a consultant for Vifor International, Amgen, Bayer, Bosch GmbH, PsiOxus Therapeutics, Professional Dietetics, and Novartis; and received research support from Vifor International and PsiOxus Therapeutics. M.G. is a consultant for Abbott Labs, Astellas, AstraZeneca, Bayer Schering PharmaAG, CorThera Inc., Cytokinetics Inc., DebioPharm S.A., Errekappa Terapeutici (Milan, Italy), Glaxo Smith Kline, JNJ, Medtronic, Novartis Pharma AG, Otsuka, Sigma Tau, Solvay Pharmaceuticals, and Pericor Therapeutics. P.R has received honoraria from AstraZeneca, Baxter-Gambro, Daiichi-Sankyo, Fresenius Medical Care, Novartis Pharmaceuticals, Relypsa, and Servier, and is a shareholder of CardioRenal diagnostics. F.Z. has received grants from Roche Diagnostics; has served on steering committees for Bayer, Boston Scientific, Gambro, Janssen, Novartis, Pfizer, Resmed, and Takeda, and on an event committee for Biotronik; and is a consultant/scientific advisory board member for Novartis, Servier, and St Jude. B.P. is a consultant to Pfizer, Merck, Novartis, Takeda, Astra Zeneca, Bayer, Lilly, BMS, Cytopherx, Amorcyte, Relypsa, BG-Medicine, Aurasense, and GE Healthcare; holds stocks options in Relypsa, BG-Medicine, and Aurasense; and has received grants from Novartis, Forrest Laboratories, and Medtronic. C.M.O. is a consultant to Merck and Amgen. The other authors have no conflict of interest to declare.




