The ‘peptide for life’ initiative in the emergency department study
Abstract
Aims
Natriuretic peptide (NP) uptake varies in Emergency Departments (EDs) across Europe. The ‘Peptide for Life’ (P4L) initiative, led by Heart Failure Association, aims to enhance NP utilization for early diagnosis of heart failure (HF). We tested the hypothesis that implementing an educational campaign in Western Balkan countries would significantly increase NP adoption rates in the ED.
Methods and results
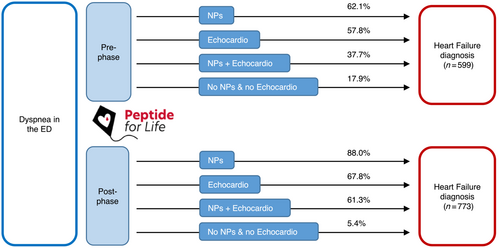
This registry examined NP adoption before and after implementing the P4L-ED study across 10 centres in five countries: Bosnia and Herzegovina, Croatia, Montenegro, North Macedonia, and Serbia. A train-the-trainer programme was implemented to enhance awareness of NP testing in the ED, and centres without access received point-of-care instruments. Differences in NP testing between the pre-P4L-ED and post-P4L-ED phases were evaluated. A total of 2519 patients were enrolled in the study: 1224 (48.6%) in the pre-P4L-ED phase and 1295 (51.4%) in the post-P4L-ED phase. NP testing was performed in the ED on 684 patients (55.9%) during the pre-P4L-ED phase and on 1039 patients (80.3%) during the post-P4L-ED phase, indicating a significant absolute difference of 24.4% (95% CI: 20.8% to 27.9%, P < 0.001). The use of both NPs and echocardiography significantly increased from 37.7% in the pre-P4L-ED phase to 61.3% in the post-P4L-ED phase. There was an increased prescription of diuretics and SGLT2 inhibitors during the post-P4L-ED phase.
Conclusions
By increasing awareness and providing resources, the utilization of NPs increased in the ED, leading to improved diagnostic accuracy and enhanced patient care.
Introduction
Natriuretic peptides (NPs) are recommended for the diagnosis of heart failure (HF) according to international guidelines and the universal definition of HF.1-3 However, despite two decades of scientific evidence supporting their use, the adoption of NPs, including B-type NP (BNP) and N-terminal BNP (NT-proBNP), in real-life clinical practice remains low and inconsistent. Indeed, the Heart Failure Association (HFA) Atlas has highlighted the significant disparities in NP utilization in the emergency departments (EDs) across Europe.4 Adoption rates are highest in Germany, central Europe, and Scandinavia, where there is greater acceptance and integration of NPs for the diagnosis of HF in the ED. On the other hand, the western Balkans, ex-Soviet republics, and Russia exhibit remarkably low adoption rates of NPs for HF diagnosis in the ED.4
‘Peptide for Life’ is a strategic initiative led by the HFA with the primary objective of promoting early diagnosis of HF through improved utilization of NPs. This multifaceted initiative encompasses several key objectives, including increasing awareness about the benefits of NPs, advocating for improved access and reimbursement, and ultimately driving wider adoption of NPs.5, 6
Based on the insights gained from the HFA Atlas and the objectives outlined in the Peptide for Life initiative, the Peptide for Life-Emergency Department (P4L-ED) study has been strategically designed to encompass six counties within the Western Balkans. The primary objective of this study was to test the hypothesis that by implementing an educational and awareness campaign targeting the healthcare team responsible for evaluating breathless patients in the ED in conjunction with improving access to NPs will result in a significant rise in the adoption rates of NPs.
Methods
This observational study investigated the adoption of NPs before and after the implementation of the P4L-ED initiative on 10 centres in 5 countries: Bosnia and Herzegovina, Croatia, Montenegro, North Macedonia, and Serbia. The P4L-ED aimed to increase awareness of NP testing in the ED and improve access to instruments capable of measuring NPs when needed. To achieve this, a train-the-trainer programme was developed to widely enhance awareness on NP testing in the ED. As part of the training process, trainers were equipped with a standardized virtual programme that incorporated three essential components. The first component involved a description of the Peptide for Life initiative. The second component focused on explaining the clinical significance of NP testing in the context of acute heart failure, emphasizing international recommendations related to NP testing. Finally, the training programme actively engaged participants through interactive case studies, enabling them to apply their knowledge and actively participate in discussions. As part of the training process, trainers were equipped with a standardized 2-h virtual programme that incorporated three essential components. Before implementation of the P4L-ED, it was identified that two centres lacked access to NP testing. As part of the initiative, these centres were provided with a point-of-care instrument (cobas h 232, Roche Diagnostics, Rotkreuz, Switzerland), and the required reagents for NT-proBNP testing.
Patients
Consecutive adult patients presenting to the ED with dyspnea as their main complaint were included in the study, with the following exceptions: patients in cardiogenic shock, those with a life expectancy of less than 6 h from ED arrival, and those who refused to provide consent. The management of patients adhered to the principles outlined in the Declaration of Helsinki. The protocol received approval from the local ethics committees and patients provided either written or oral general consent in accordance with applicable local regulations.
Measures and outcomes
At the time of inclusion, baseline characteristics, including demographic information, comorbidities data, vital parameters, and symptoms, were documented. Additionally, the utilization of diagnostic exams, such as ECG, lung ultrasound, and chest X-ray, was recorded. Results of blood exams (haemoglobin, sodium, potassium creatinine, and urea concentrations) were gathered when available. The presence or absence of NP testing upon admission and at discharge was documented, along with the corresponding NP concentrations. Final diagnosis and treatments at discharge as well as patient status (dead or alive) were documented.
The primary outcome was to compare the rate of patients presenting to the ED with dyspnea and undergoing NP testing, pre and post implementation of the P4L-ED initiative. Secondary outcomes included the comparison of diagnostic pathways, final diagnosis and treatments, pre and post P4L-EdD.
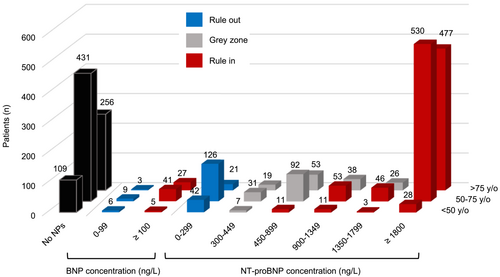
Natriuretic peptide cut-points
The cut-points utilized to classify patients as ‘rule-in’ or ‘rule-out’ for acute heart failure were based on the 2021 ESC-HFA clinical guidelines.1 For NT-proBNP, a single rule-out cut-point of 300 pg/mL was employed. Additionally, age-adjusted rule-in cut-points were applied as follows: <50 years: 450 pg/mL, 50–75 years: 900 pg/mL, and >75 years: 1800 pg/mL. The range between the rule-in and rule-out cut-points was designated as the grey zone category, indicating results that were inconclusive based on accepted cut-off points. Regarding BNP measurements, a single cut-point of 100 pg/mL was utilized to determine both the rule-in and rule-out status for heart failure.
Statistical analysis
Based on the EURODEM study,7 it was anticipated that the utilization of NP in the ED during the pre-P4L-ED phase would be 35%. A clinically significant increase of 20% was deemed meaningful, leading to a target of 42% NP testing in the post-P4L-ED phase. To achieve a statistical power of 90% and a significance level of 5%, a minimum of 1253 patients would need to be included during each phase of the study.
Descriptive statistics were computed to analyse the characteristics of the study groups. Continuous variables were presented as median values accompanied by interquartile range (IQR), while categorical variables were reported as absolute numbers and percentages. To assess the differences between pre-P4L-ED phase and post-P4L-ED phase, the Mann–Whitney U test was employed for continuous variables, and the chi-square (𝜒2) or Fisher's exact test was used for dichotomous variables. The primary endpoint, NP testing upon admission, was compared between the groups using the chi-square (𝜒2) test with Yates correction for continuity. A P-value of <0.05 was considered statistically significant. IBM SPSS Statistics version 20 (New York, NY) was utilized for all statistical analyses.
Results
A total of 2519 patients were included in the study. The pre-P4L-ED phase began on 14 September 2022, and spanned 72 days, during which 1224 (48.6%) patients were included. The post-P4L-ED phase started on 10 March 2023, and lasted 78 days, with 1295 (51.4%) patients included. The period between these two phases (from 25 November 2022 to 30 January 2023) was dedicated to conducting the P4L-ED training and installing point-of-care NP measuring devices in the two designated centres, ensuring that all necessary preparations were completed before the subsequent phase of the study. Totally, 81 healthcare professionals were trained (38 cardiologists, 26 emergency physicians, and 17 others).
Table 1 displays the baseline characteristics of the patients. In the pre-P4L-ED group, a significantly higher proportion of patients had pulmonary comorbidities and experienced rest dyspnoea upon admission. However, no significant differences were found between the pre and post groups regarding oxygen saturation levels and the need for oxygen supply upon admission.
| All (n = 2519) | Before (n = 1224) | After (n = 1295) | P-value | |
|---|---|---|---|---|
| Age (years) | 72 [63;80] | 71 [62;80] | 72 [63;80] | 0.14 |
| Male sex | 1397 (55.6) | 677 (55.3) | 720 (55.6) | 0.92 |
| Body mass index (kg/m2) | 26.9 [24.6;29.7] | 27.4 [24.7;30.3] | 26.8 [24.4;29.4] | 0.10 |
| Co-morbidities | ||||
| Hypertension | 2023 (80.5) | 965 (79.0) | 1058 (82.0) | 0.06 |
| Diabetes | 871 (34.7) | 423 (34.7) | 448 (34.7) | 1.00 |
| Dyslipidaemia | 958 (38.9) | 448 (37.2) | 510 (40.6) | 0.09 |
| Myocardial infarction | 500 (20.0) | 251 (20.6) | 249 (19.4) | 0.48 |
| Valvular disease (history) | 411 (16.4) | 175 (14.4) | 236 (18.4) | 0.01 |
| Atrial fibrillation (history) | 786 (31.3) | 356 (29.1) | 430 (33.4) | 0.02 |
| Chronic kidney disease | 530 (21.2) | 243 (20.0) | 287 (22.3) | 0.16 |
| Chronic pulmonary disease | 573 (22.7) | 338 (27.6) | 235 (18.1) | <0.001 |
| Non smoker | 1521 (72.0) | 733 (73.7) | 788 (70.5) | 0.11 |
| Signs and symptoms | ||||
| Effort dyspnoea | 2319 (92.5) | 1094 (89.6) | 1225 (95.2) | <0.001 |
| Rest dyspnoea | 1720 (68.7) | 911 (74.6) | 809 (63.0) | <0.001 |
| Nocturnal dyspnoea | 738 (31.1) | 382 (31.9) | 356 (30.3) | 0.45 |
| Asthenia | 601 (24.8) | 273 (23.0) | 328 (26.5) | 0.05 |
| Leg oedema | 964 (38.4) | 469 (38.4) | 495 (38.4) | 1 |
| Jugular vein distention | 123 (5.2) | 52 (4.4) | 71 (6.1) | 0.07 |
| Hepatojugular reflux | 64 (2.7) | 32 (2.7) | 32 (2.8) | 1 |
| Hepatomegaly | 104 (4.4) | 45 (3.7) | 59 (5.0) | 0.15 |
| 3rd heart sound | 79 (3.2) | 35 (2.9) | 44 (3.4) | 0.53 |
| Cardiac murmur | 637(25.3) | 290 (23.7) | 347 (26.8) | 0.08 |
| Lung rales | 1308 (52.0) | 620 (50.7) | 688 (53.2) | 0.24 |
| Pleural effusion | 824 (33.0) | 392 (32.2) | 432 (33.7) | 0.47 |
| Vital parameters at admission | ||||
| SBP (mmHg) | 130 [118;150] | 130 [115;150] | 130 [120;150] | 0.24 |
| DBP (mmHg) | 80 [70;80] | 80 [70;90] | 80 [70;90] | 0.48 |
| Heart rate (/min) | 90 [75;109] | 90 [75;110] | 90 [75;106] | 0.27 |
| Respiratory rate (/min) | 17 [15;20] | 16 [15;20] | 18 [15;20] | 0.38 |
| Temperature (°C) | 36.3 [36.0;36.6] | 36.2 [36.0;36.6] | 36.3 [36.0;36.6] | 0.48 |
| Oxygen saturation (%) | 94 [90;97] | 94 [90;97] | 95 [90;97] | 0.09 |
| Oxygen supply | 759 (30.9) | 355 (29.2) | 404 (32.6) | 0.08 |
| Blood exams at admission | ||||
| Haemoglobin (g/L) | 130 [114;144] | 130 [114;144] | 131 [114;145] | 0.61 |
| Sodium (mmol/L) | 139 [136;141] | 139 [136;141] | 139 [136;141] | 0.16 |
| Potassium (mmol/L) | 4.3 [4.0;4.7] | 4.3 [4.0;4.7] | 4.3 [4.0;4.7] | 0.29 |
| Creatinine (umol/L) | 97 [76;134] | 97 [75;131] | 98 [76;136] | 0.32 |
| Urea (mmol/L) | 8.1 [6.0;11.8] | 8.0 [5.7;11.6] | 8.3 [5.9;12.0] | 0.14 |
- DBP, diastolic blood pressure; SBP, systolic blood pressure.
Eight hundred seventy-eight patients, out of the initial 1372 (1372–1494 = 878), who had a known history of heart failure were ultimately diagnosed with heart failure. Among the patients with a known history of heart failure, 35 received a final diagnosis other than acute heart failure. Four hundred ninety-four patients received a de novo diagnosis of heart failure, and 1112 patients without a prior history of heart failure received a final diagnosis other than acute heart failure.
Natriuretic peptide testing
During the pre-P4L-ED phase, 684 patients (55.9% of the total) underwent NP testing, whereas in the post-P4L-ED phase, 1039 patients (80.3% of the total) were tested. This represents an absolute difference of 24.4% (95% confidence interval: 20.8% to 27.9%, P < 0.001) between the two phases. In the two centres where NP testing was unavailable during the pre-P4L phase (n = 79 inclusions, 0% NP testing), all patients (n = 106 inclusions) were tested in the post-P4L-ED phase after the introduction of point-of-care NP testing. Consequently, the increased accessibility to NP testing accounted for 33.5% of the total absolute difference observed between the pre-P4L-ED and post-P4L-ED phases. The detailed analysis of NP testing is presented in Table 2.
| All (n = 2519) | Before (n = 1224) | After (n = 1295) | P-value | |
|---|---|---|---|---|
| NPs measured at admission | 1723 (68.4) | 684 (55.9) | 1039 (80.3) | <0.001 |
| NT-proBNP | 1632 (64.8) | 658 (53.8) | 974 (75.3) | |
| BNP | 91 (3.6) | 26 (2.1) | 65 (5.0) | |
| NPs concentrations at admission | ||||
| NT-proBNP (ng/L) | 3430 [907;9000] | 3200 [877;10 147] | 3590 [960;9000] | 0.74 |
| BNP (ng/L) | 374 [128;1072] | 727 [289;2605] | 352 [101;830] | 0.01 |
| NT-proBNP cut offs | 0.72 | |||
| Rule out | 189 (11.7) | 74 (11.3) | 115 (12.0) | |
| Grey zone | 266 (16.5) | 117 (17.9) | 149 (15.5) | |
| Rule in | 1159 (71.8) | 464 (70.8) | 695 (72.5) | |
| <50 years olda | 53 (51.9) | 21 (50.0) | 32 (53.3) | |
| 50–75 years olda | 629 (71.6) | 261 (73.3) | 368 (70.5) | |
| >75 years olda | 477 (75.2) | 182 (70.8) | 295 (78.2) | |
| BNP | ||||
| Rule out | 18 (19.8) | 2 (7.7) | 16 (24.6) | 0.12 |
| Rule in | 73 (80.2) | 24 (92.3) | 49 (75.4) | 0.12 |
| NPs measured at discharge | 288 (11.8) | 94 (7.9) | 194 (15.6) | <0.001 |
| NT-proBNP | 267 (11.0) | 82 (6.9) | 185 (14.9) | |
| BNP | 21 (0.9) | 12 (1.0) | 9 (0.7) | |
| NPs concentrations at discharge | ||||
| NT-proBNP (ng/L) | 1901 [929;4900] | 1894 [872;4393] | 1931 [986;4987] | 0.89 |
| NT-proBNP > 1500 ng/L | ||||
| BNP (ng/L) | 355 [154;2216] | 570 [172;2471] | 209 [12;537] | 0.35 |
| NPs measured at admission and discharge | 251 (14.5) | 75 (11.0) | 176 (16.9) | <0.001 |
| [NPs] decrease by 30% | 153 (61.0) | 45 (60.0) | 108 (61.4) | 1 |
- BNP, B-type natriuretic peptide; NPs, natriuretic peptides; [NPs], concentration of natriuretic peptides; NT-proBNP, N-terminal pro-B-type natriuretic peptide.
- a Values are reported as n (% of the total number of patients in the same age cut-off).
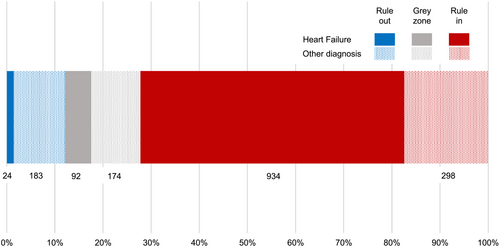
NT-proBNP was measured in 1632 individuals, accounting for 64.8% of the study population, while BNP was measured in 91 patients, representing 3.6% of the population. In general, a greater number of patients were identified as ‘rule-in’ rather than ‘rule-out’ based on NP testing upon admission. Among the NT-proBNP patients, 16.5% fell into the grey zone category (Table 2 and Figure 1).
Although not the primary objective of this study, it was also of interest to document the utilization of NPs before discharge. Interestingly, there was a significant increase in the rate of NP testing at both admission and discharge from the pre-P4L-ED phase to the post-P4L-ED phase. Specifically, the rate of NP testing doubled, rising from 7.9% in the pre-P4L-ED phase to 15.6% in the post-P4L-ED phase (P < 0.001) (Table 2).
Patient management and follow-up
In the post-P4L-ED phase, a higher number of patients underwent echocardiography compared with the pre-P4L-ED phase [656 patients (52.2%) vs. 471 patients (38.5%), P < 0.001]. However, there were no significant differences observed in the left ventricular ejection fraction (LVEF) between the two groups (pre-P4L-ED: 40% [30;50] vs. post-P4L-ED: 43% [30;50], P = 0.26). HF categories according to LVEF was also not different between groups [pre-P4L-ED: reduced 178 patients (50.4%); mildly reduced 98 patients (28.6%); preserved 67 patients (19.5%) vs. post-P4L-ED: reduced 255 patients (48.9%); mildly reduced 132 patients (25.4%); preserved 134 patients (25.7%), P = 0.82].
The diagnostic pathways for diagnosing acute heart failure (HF) utilizing both natriuretic peptides (NPs) and echocardiography exhibited notable differences between the pre-P4L-ED and post-P4L-ED phases. Specifically, the proportion of patients following diagnostic pathways that incorporated both NPs and echocardiography increased significantly from 37.7% in the pre-P4L-ED phase to 61.3% in the post-P4L-ED phase (Figure 2).
There were no significant differences observed in the use of electrocardiogram (ECG) between the pre-P4L-ED phase (1207 patients, 98.6%) and the post-P4L-ED phase (1274 patients, 98.4%) (P = 0.75). Similarly, there were no significant differences in the use of lung ultrasound between the pre-P4L-ED phase (47 patients, 3.8%) and the post-P4L-ED phase (66 patients, 5.1%) (P = 0.15). However, a lower number of patients received chest X-ray in the post-P4L-ED phase (829 patients, 64.0%) compared with the pre-P4L-ED phase (914 patients, 74.7%) (P < 0.001).
Table 3 and Figure 3 present the final diagnosis and outcomes of the patients. Among those who were identified as ‘rule-in’ based on the diagnostic criteria, the majority received a final diagnosis of heart failure. This trend was particularly notable in the post-P4L-ED phase, indicating an improved accuracy in diagnosing HF after the implementation of the P4L-ED initiative (Figure S1).
| All (n = 2519) | Before (n = 1224) | After (n = 1295) | P-value | |
|---|---|---|---|---|
| Final diagnosis | <0.001 | |||
| Heart failure | 1372 (57.9) | 599 (51.3) | 773 (64.4) | |
| de novo heart failure | 494 (36.0) | 199 (33.2) | 295 (38.2) | 0.05 |
| Pulmonary infection | 180 (7.6) | 98 (8.4) | 82 (6.8) | |
| COPD exacerbation | 174 (7.3) | 113 (9.7) | 61 (5.1) | |
| Pulmonary embolism | 68 (2.9) | 29 (2.5) | 39 (3.2) | |
| Asthma | 54 (2.3) | 28 (2.4) | 26 (2.2) | |
| Pneumothorax | 5 (0.2) | 4 (0.3) | 1 (0.1) | |
| Other | 515 (21.8) | 297 (25.4) | 218 (18.2) | |
| Trigger of this acute episode | <0.001 | |||
| Acute Coronary síndrome | 153 (11.8) | 73 (12.7) | 80 (11.1) | |
| Hypertension emergency | 78 (6.0) | 31 (5.4) | 47 (6.5) | |
| Arrhythmia | 229 (17.6) | 86 (14.9) | 143 (19.8) | |
| Mechanical cause | 3 (0.1) | 1 (0.1) | 2 (0.1) | |
| Pulmonary embolism | 16 (1.2) | 4 (0.7) | 12 (1.7) | |
| Infection | 178 (13.8) | 85 (14.8) | 93 (12.9) | |
| Tamponade | 0 (0) | 0 (0) | 0 (0) | |
| Anaemia | 49 (3.8) | 26 (4.4) | 23 (3.2) | |
| Lack of treatment adherence | 114 (8.8) | 49 (8.5) | 65 (9.0) | |
| None evident | 303 (23.3) | 172 (29.8) | 131 (18.2) | |
| Other | 175 (13.6) | 50 (8.7) | 125 (17.5) | |
| Hospitalization after ED | 1448 (57.5) | 669 (54.7) | 779 (60.1) | 0.006 |
| For heart failure | 976 (67.4) | 409 (61.1) | 567 (72.8) | <0.001 |
| Inhospital death | 205 (8.1) | 112 (9.1) | 93 (7.2) | 0.08 |
- COPD, chronic obstructive pulmonary disease; ED, emergency department.
During the post-P4L-ED phase, more patients were hospitalized for heart failure. At discharge, the prescription rates of diuretics (69.4% vs. 64.0%, P = 0.005) and sodium/glucose cotransporter 2 inhibitors (SGLT2i) (24.9% vs. 16.5%, P < 0.001) were significantly different between the pre-P4L-ED and post-P4L-ED groups. However, there were no significant differences in the prescription rates of RAS inhibitors (ACE inhibitors, ARBs, ARNI) (pre-P4L-ED: 59.3% vs. post-P4L-ED: 60.1%, P = 0.48), beta-blockers (pre-P4L-ED: 64.7% vs. post-P4L-ED: 65.6%, P = 0.67), and mineralocorticoid receptor antagonists (pre-P4L-ED: 37.5% vs. post-P4L-ED: 38.6%, P = 0.60) between the two groups.
Discussion
Despite the well-established recognition of NPs for diagnosing acute HF in patients presenting to the ED with breathlessness, their adoption in clinical practice remains low and varies widely between countries.4 This multicountry study conducted in the western Balkans aimed to address this issue by raising awareness among healthcare physicians responsible for evaluating dyspneic patients in the ED and improving access to NPs. The results of the study provide compelling evidence that these interventions had a significant impact on the adoption of NPs. The study observed a remarkable increase in the use of NPs, with utilization rates rising from 55.9% in the pre-P4L-ED phase to 80.3% in the post-P4L-ED phase. This finding aligns with the primary objective of the P4L-ED study, demonstrating the effectiveness of the educational campaign and improved access to natriuretic peptides in promoting their adoption among healthcare professionals.
The impact of the P4L-ED initiative goes beyond the mere increase in the adoption of NP testing. It has the potential to transform the entire diagnostic pathway for acute heart failure patients, particularly by facilitating the detection of more patients with HF through the ‘rule-in’ approach. This is evident from the increased utilization of echocardiography, which is recommended in the guidelines for diagnosing acute HF in the presence of a positive NP test.1 The higher frequency of echocardiography in the post-P4L-ED phase suggests an improved patient management approach. By incorporating both NP testing and echocardiography, clinicians can achieve a more comprehensive and accurate diagnosis, leading to appropriate treatment decisions and better patient outcomes. Another notable finding is the reduced use of chest X-rays in the diagnostic process during the post-P4L-ED phase, despite the undeniable importance of chest X-ray in the diagnosis of AHF, where it is extremely important to quickly identify important comorbidities.8 The decreased reliance on chest X-ray further supports the shift towards a more evidence-based and effective diagnostic approach by emphasizing the use of NPs.
Despite the availability of multiple NPs for the diagnostic evaluation of HF as recommended by the most recent ESC guidelines,1 the use of NT-proBNP is predominant in clinical practice. This trend is consistent with findings from the ESC Heart Failure Long-Term Registry, which identified NT-proBNP as the most utilized peptide for diagnosing and managing HF in Europe.9 This study further confirms these observations in the western Balkans, where NT-proBNP was used in 95% of cases, while BNP was used in only 5% of cases. Notably, MR-proANP was not used in any case. The preference for NT-proBNP over other natriuretic peptides can be attributed to several factors. First, NT-proBNP concentrations are higher compared with BNP, which is the biologically active component of the pro-peptide, which enhances the reliability and sensitivity of the assay in detecting HF. In addition, NT-proBNP demonstrates greater stability in vitro after blood sample collection, reducing concerns related to transportation delays between the clinic and the laboratory.10, 11
The utilization of NPs for early diagnosis not only aids in the detection of acute heart failure but also has an impact on patient treatments.12 In this study, we observed an increased use of diuretics. This suggests that the timely and accurate diagnosis facilitated by NP testing allows for more targeted and effective treatment strategies, such as the appropriate administration of diuretics to manage fluid overload. Furthermore, the study also revealed an increase in the use of SGLT2 inhibitors (SGLT2i). While part of this increase may be attributed to the improved diagnosis of heart failure, it is important to consider the potential influence of time bias. SGLT2i have been gaining recognition for their positive effects on HF outcomes, as demonstrated in pivotal trials.13
In the current study, there was a significant increase in the use of NPs at discharge from 7.9% to 15% between the pre- and post-P4L-ED phases. However, this level of utilization is still insufficient to promote the proper adoption of guideline-directed medical treatment (GDMT) as demonstrated by the STRONG-HF trial.14 The STRONG-HF trial employed a threshold of 1500 pg/mL of NT-proBNP prior to discharge to randomize patients into high-intensity care or usual care groups. The high-intensity care group received intensive management including the initiation of RASi, beta-blockers, and mineralocorticoid receptor antagonists (MRAs) before discharge. The medication doses were gradually uptitrated during sequential visits in the first weeks after discharge.14 In the current study, there were no identified improvements in the utilization of RASi, beta-blockers, or MRAs between the pre- and post-P4L-ED phases. This lack of improvement may be attributed to the relatively low adoption of NPs at the pre-discharge stage or to inertia in initiating GDMT after hospitalization. The data from the STRONG-HF trial serve as an important stimulus to initiate GDMT before discharge, relying on NT-proBNP measurements prior to discharge and in the early post-discharge period.
This study has several limitations that need to be acknowledged. First, the pre-P4L-ED phase was conducted retrospectively, while the post-P4L-ED phase was prospective. This difference in study design may introduce some degree of bias and potential confounding factors. However, it is important to note that both phases included consecutive patients, and the number of patients recruited in a similar timeframe was comparable. Second, the number of participating centres from each country is limited and may not fully represent the entire country's healthcare system. This could introduce some regional variations and potential selection bias. Nonetheless, these centres provide a real-life snapshot of the implementation of the P4L-ED initiative in the western Balkans. Last, like any educational and awareness programme, the degree of adherence to the trained content among healthcare professionals may vary. The effectiveness of the P4L-ED training programme may depend on the individual motivation and engagement of the participants, which could introduce variability in the implementation of NP testing and subsequent management practices.
Conclusions
The P4L-ED study successfully demonstrated that by raising awareness among healthcare professionals and providing them with the necessary tools and resources, there was an increase in the utilization of NPs, thereby enhancing the diagnostic accuracy and improving patient care. The results of this study have broader implications for healthcare systems aiming to optimize the management of acute heart failure. By implementing similar educational initiatives and ensuring adequate access to NPs, healthcare professionals can make more informed decisions in diagnosing and managing patients with heart failure.15
Acknowledgements
Appendix (young physicians): Milenko Tomić, Stefan Stanković, Marija Klarić, Mihajlo Viduljević, Nemanja Djordjević, Jovana Klac, Danka Civrić, Teodora Pejović, Blagoje Babić, Tanja Nenezić, Zoran Radovanović, Bogdana Jungić, Aleksandra Milovančev, Jelena Tripunović, Nikola Denda, Isidora Milosavljević, Milica Janković, Božana Diković, Zan Zimbakov, Irena Mitevska, Lazar Kostovski, Višeslav Popadić, Aleksandra Radojević, Andrea Manojlović, Dušan Radovanović, Tatjana Ivanković, Uroš Gajić, Maša Stojanović, Djordje Marinković, Jovana Stojković, Bojan Stojčić, Valentina Savić, Mina Bogdanović, Marija Sredojević, Nikola Blagojević, Mihailo Radovanović, Ljiljana Tabaković, Josip Andelo Borovac, Mijo Meter, Mate Parčina, Ante Šošić, Marina Ivanišević Džaja, Josip Katić, Vedran Pašara, Sara Hoteit, Zrinka Planinić. [Correction added on 29 December 2023, after first online publication: Josip Andelo Borovac's name has been corrected in this version.]
Conflict of interest
AB-G has lectured and/or participated in advisory boards for Abbott, AstraZeneca, Bayer, Boehringer Ingelheim, Novartis, Roche Diagnostics, and Vifor.
Funding
Roche Diagnostics provided funding to support the organization of the study, including point-of-care instruments and reagents where needed. Roche Diagnostics was not involved in any aspect of study conception or result interpretation.
Conflict of interest
AB-G reports personal fees or advisory boards from Abbott, AstraZeneca, Boehringer Ingelheim, Bayer, Novartis, NovoNordisk, Roche Diagnostics and Vifor Pharma. The rest ofthe authors declare no conflict of interest.




