Reply to: More data about cardiac and neurologic findings would be useful
We thank Stöllberger et al. for their interest in our study,1 and we gladly report additional information.
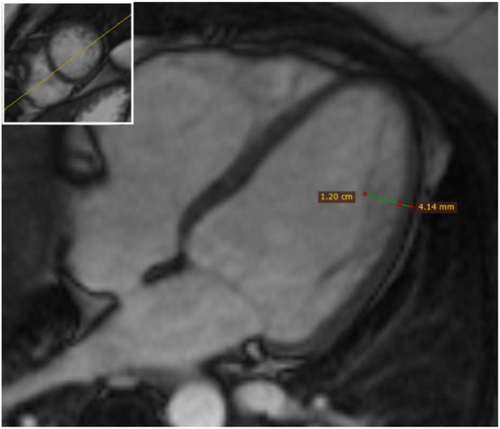
Cardiac magnetic resonance (cMR) images were reviewed in patients with myotonic dystrophies (available in 26/29 patients) focussing on left ventricular (LV) non-compaction. We found a mean diastolic ratio of non-compacted/compacted myocardium (NC/C) of 1.41 ± 0.57. One patient (myotonic dystrophy type 1) complied with cMR-criteria (NC/C > 2.3)2 exhibiting a mild phenotype with a maximum NC/C ratio of 2.9 apicolateral (AHA segment 16) (Figure 1).
The rationale to exclude patients with concomitant cardiac disease has been laid out in our paper. We sought to exclude acquired cardiac disease that may bias towards over-reporting cardiac involvement due to skeletal myopathies. Inclusion of patients with significant coronary artery disease (CAD), history of myocardial infarction, or status post myocarditis might lead to wrong interpretation as cardiac involvement. Naturally, individual subjects may suffer from a combination of both; however, confidently distinguishing phenotypes may be difficult. Here, we thus sought to define a true negative background population in terms of acquired disease.
Computed tomography coronary angiography (CTA) was performed in 36 patients at increased risk for CAD. From eight patients with suspected significant CAD on CTA, six additionally underwent invasive coronary angiography, which confirmed significant CAD in five.
In our entire cohort (n = 73), 16% were treated with ACE inhibitors or AT1-receptor antagonists, 6% with beta-blockers, 4% with calcium antagonists, and 6% with thiazide diuretics. Only five patients in the whole cohort had reduced LV ejection fraction <50% (cMR), of those one (Becker muscular dystrophy) took an AT1-receptor antagonist and beta-blocker and one (Duchenne muscular dystrophy) an ACE inhibitor. Thus, cardiologic screening identified patients with potential for improving heart failure therapy.
While all patients underwent 24 h ECG, no patient had received an event recorder at the time of data acquisition.
Other requested data such as family history of cardiac disease, neuromuscular impairment, genotype, and comprehensive follow up examinations were out of the scope of this study, which focused on cardiac involvement in a cross-sectional design.
Overall, cardiac involvement was absent or mild in the majority of patients in our cohort, especially in myotonic dystrophies.




