Preserved ejection fraction and structural heart disease in 446 848 patients investigated with echocardiography
Abstract
Background
Sex-specific differences in left ventricular ejection fraction (LVEF) and responses to neurohormonal modulating therapies are relevant to clinical trials of treatment for heart failure with preserved ejection fraction (HFpEF).
Aims
This study aimed to identify the proportion and characteristics of patients presenting with possible or confirmed HFpEF within the National Echo Database of Australia.
Results
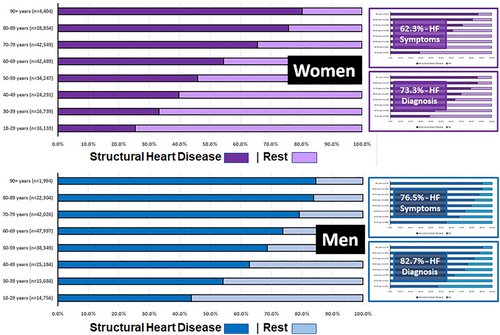
A total of 237 046 women (48.1%) and 256 019 men (aged 61.0 ± 18.3 vs. 60.6 ± 17.1 years, respectively) had sex-specific distributions of LVEF: 94.3% of women had LVEF ≥ 45% (mean LVEF 66.0 ± 8.6%), compared with 87.2% of men (mean LVEF 63.4 ± 8.7%). The presence of structural heart disease (SHD) according to the PARAGON-HF criteria could be calculated in 93.8% of women and 93.4% of men with an LVEF ≥ 45%. Of these, 64 502 (30.8%) women and 104 344 (50.0%) of men had left ventricular hypertrophy, and 78 948 (35.3%) and 95 846 (42.9%), respectively, had left atrial enlargement. As a result, the proportion of women vs. men fulfilling echocardiographic criteria for HFpEF was very different: 111 497 (53.2%) vs. 146 359 (70.1%). SHD markedly increased with age, associated with a greater increase in women than men. The same signal was observed in those referred for suspected or previously confirmed HFpEF.
Conclusions
Double the number of men than women had LVEF < 45%, and the distribution of SHD had was highly sex specific. Left ventricular hypertrophy and left atrial enlargement were more common in men and becoming more frequent in women with advancing age. The echocardiographic SHD distribution was similar in those referred with suspected or confirmed HFpEF. The findings are relevant to sex-specific recruitment criteria for future clinical trials.
Background
In contrast to clear benefits of applying neurohormonal modulating therapies demonstrated in those with heart failure (HF) with reduced ejection fraction, ideal treatment for those with HF with preserved ejection fraction (HFpEF) remains unclear.1 Because of sex-related differences in HF with reduced ejection fraction, this inherently means that more men than women have access to definitive, potentially life-saving treatment. Recently, composite findings from key trials, such as TOPCAT2 and PARAGON-HF,3 suggest that women with more ‘preserved’ left ventricular (LV) function respond better to such treatment.4 If confirmed, this observation will undoubtedly increase the pool of overall treatable cases with HFpEF. It might also redress the persistent issue of inequitable access to evidence-based HF therapies based on sex. However, to what extent is currently unknown.
Aims
Within the real-world patient cohort of the second iteration of the National Echocardiography Database of Australia (NEDA) Study,5 we sought to determine the proportion and characteristics of those who presented (on their first echocardiogram) with potential HFpEF based on an ejection fraction LVEF ≥ 45% and concurrent evidence of structural heart disease (SHD).
Methods
As described in greater detail previously,5 NEDA is a very large, ongoing observational registry that captures individual echocardiographic reporting data that are robustly linked to mortality outcomes via the National Death Index of Australia. It conforms to the highest standards of observational reporting, has received all relevant ethics approvals, and adheres to the Declaration of Helsinki. NEDA is also registered with the Australian New Zealand Clinical Trials Registry (ACTRN12617001387314). For the purpose of this report, profiling data on 493 155 individual cases with a first-reported echocardiogram conducted at 23 different centres Australia wide (https://www.neda.net.au/participating-sites/) during the period January 2000 to May 2019 were analysed.
All echocardiographic measurement and report data, including basic demographic profiling (biological sex and date of birth) and date of investigation, contained in the echocardiographic database of participating centres were collected and remotely transferred into a central database via a ‘vendor-agnostic’ automated data extraction process. Following a rigorous data cleaning and linkage process (including the application of text recognition software to capture free text reporting), the Master NEDA Database (v2.0) was finalized.
All individual LVEF values were initially recoded into five-unit groups, and a total of 446 848 cases with an LVEF ≥ 45% (90.6%) were identified. For the purpose of this report, PARAGON-HF Trial criteria3 were applied to determine the presence of SHD based on current evidence of (i) LV hypertrophy (LVH), defined as septal or posterior wall thickness >1.1 cm, and/or (ii) left atrial (LA) enlargement defined as any of the following: (a) LA width >3.8 cm, (b) LA length >5.0 cm, (c) LA area >20 cm2, (d) LA volume >55 mL, and/or (e) LA volume index >29 mL/m2. With no sex-specific adjustments, as originally applied, Criteria a–c and d/e were derived from four-chamber views and the biplane method, respectively. The overall distribution of cases fulfilling these criteria, with subgroup analyses of those referred with symptoms indicative of HF and those with a diagnosis of HF, is presented on an age and sex-specific basis with no imputation of missing data. Given the enormous size of the cohort, unless otherwise indicated, all statistical comparisons resulted in a P-value <0.001.
Results
The cohort comprised 237 046 women (48.1%) who were slightly older (61.0 ± 18.3 vs. 60.6 ± 17.1 years) than their 256 019 male counterparts. The distribution of cases with an LVEF above and below 45% was highly sex specific. Among women, there were 13 544 cases (5.7%) with an LVEF < 45% (mean 33.6 ± 8.6%); those with LVEF ≥ 45% (mean LVEF 66.0 ± 8.6%) were older (68.5 ± 16.4 vs. 60.5 ± 18.4 years), slightly heavier (body mass index 28.0 ± 7.0 vs. 27.7 ± 7.4 kg/m2), with lower estimated right ventricular systolic pressures (32.1 ± 10.7 vs. 37.6 ± 12.4 mmHg), and had less valvular disease (14.0% vs. 37.6%). Among men, there were more than double presenting with an LVEF < 45% (32 773–12.8%, mean 32.6 ± 8.9%). The remainder of men (LVEF 63.4 ± 8.7%) were also older (66.5 ± 14.9 vs. 59.8 ± 17.2 years), had equivalent body mass indices (28.1 ± 5.5 kg/m2), but with similarly lower estimated right ventricular systolic pressures (31.9 ± 10.2 vs. 37.1 ± 12.1 mmHg) and less valvular disease (13.2% vs. 31.8%).
Overall, 209 706 (93.8%) and 208 656 (93.4%) women and men with an LVEF ≥ 45%, respectively, had sufficient echocardiographic measurements to define the presence of SHD according to the PARAGON-HF criteria. Of these, 64 502 (30.8%) and 78 948 (35.3%) of women fulfilled the criteria for LVH and LA enlargement. The equivalent figures among men were much higher, being 104 344 (50.0%) for LVH and 95 846 (42.9%) for LA enlargement, respectively. Accordingly, the overall proportion of women (111 497–53.2%) vs. men (146 359–70.1%) fulfilling echocardiographic criteria for SHD and potential HFpEF was markedly different. As shown in Figure 1, there was a strong increase in the prevalence of SHD for those with an LVEF ≥ 45% in both sexes overall but even stronger in women than men (rising from 25.4% to 80.3% and from 43.7% to 84.6% in those aged 18–29 to 90+ years, respectively). Because NEDA does not (yet) capture clinical co-morbidity data or N-terminal pro-brain natriuretic peptide values, the later required for recruitment into PARAGON-HF, we also analysed those referred with suspected or known HF. As also shown in Figure 1, the proportion of both women (9842/15 215 and 8139/15 215) and men (7740/10 114 and 8064/9752) with SHD was progressively higher in patients referred for investigation with HF symptoms and a pre-confirmed diagnosis of HFpEF, respectively, noting the same age gradients being evident.
Conclusions
Using data from a very large echocardiographic repository, we found that double the number of men than women had LVEF < 45%. Applying PARAGON-HF criteria for SHD3 identified many more men than women fulfilling the criteria for LVH and LA enlargement, particularly with increasing age, and proportionally more women had a preserved LVEF. This finding was maintained in patients referred with suspected or confirmed HF. The SHD criteria resulted in significant sex differences in LVEF ≥ 45% and is likely to have influenced the broad pool of cases from which recent trials (such as PARAGON-HF3 and TOPCAT2) have recruited.4 Rather than the use of two-dimensional LV linear dimensions, guidelines recommend the use of indexed LV mass to identify LVH.6 Similarly, indexed LA volumes are preferred over linear measurements. The inclusive nature of the defined criteria for SHD in these trials, as well as the absence of sex-specific criteria, may possibly have allowed some patients without significant SHD to be recruited.6 Our finding of sex-specific differences in LVEF and SHD is clinically important given the need for specific echocardiographic criteria for future clinical trials, an increasing focus on finding effective HFpEF treatments, and evidence that women potentially benefit more than men from neurohormonal modulating therapy.4
Funding
This work has been funded by Novartis. S.S. is supported by the National Health and Medical Research Council of Australia (GNT1135894).




