Resilience assessment methods for hospitals subjected to earthquakes: State of the art
Abstract
Hospitals play essential roles in modern communities in the lives of people. During and after earthquakes, they are supposed to be resilient and provide continued medical and social services. Resilience assessment methods are essential for determining hospitals' resilience levels, and the results will provide a direct basis and foundation for the design of new hospitals and retrofit optimization of existing hospitals. This paper reviews the resilience assessment methods and performance measures for hospitals subjected to earthquakes. Current assessment methods are divided into indicator- and functionality-based categories, and the performance measures for quantifying the functionality of hospitals are classified into availability, productivity, quality, and hybrid. This study will assist stakeholders and managers in understanding available assessment methods.
1 INTRODUCTION
The health sector, consisting of all businesses related to medical service provision and good manufacture, plays pivotal roles in modern communities, closely bound up with people's lives. As the primary provider of medical services, healthcare systems broadly include hospitals, emergency medical services, public health agencies, outpatient clinics, long-term care facilities, home health providers, and correctional health services.1, 2 Hospitals are the most critical infrastructures and are expected to meet user demands and reflect the needs and values of the communities in and around them.3 In emergencies, they should be resilient and able to maintain and scale up efficient and timely services, with attention to providing high-quality, compassionate, and equitable treatment for casualties and survivors.3, 4 Meanwhile, hospitals would provide leadership during the response phase of a disaster for the whole healthcare system,5 and become the centralized points of community support and assistance to provide shelter, water, food, and medication for the victims who surge into hospitals during and in the immediate aftermath of disasters.6
Earthquakes are one of the most severe disasters that hospitals have to face. Several regulations, plans, and retrofit projects have been proposed to improve hospitals' performance during and after earthquakes. Ordinance SB1953 enacted in California, USA, requires all acute care facilities by 2030 to be retrofitted to a level that can fully operate following an earthquake.7 Health Building Notes8 provided healthcare guidance under the UK Civil Contingency Act 2004 to determine appropriate levels of resilience for sites, buildings, and installations against hazards and threats. The 27th Pan American Sanitary Conference9 approved a regional initiative on disaster-resilient health facilities and encouraged assessment of the existing health facilities and the potential vulnerabilities to disasters to develop long-term plans to eliminate such vulnerabilities. The second World Conference for Disaster Reduction approved the Hyogo Framework for Action to ensure that hospitals function in disaster situations for newly built hospitals and existing health facilities through reinforcing efforts.10 The Sendai Framework for Disaster Risk Reduction 2015–2030 proposed four priorities (understanding disaster risk, strengthening disaster risk governance, investing in disaster risk reduction, and enhancing disaster preparedness) to promote disaster risk reduction in disaster preparedness, prevention, response, recovery, and rehabilitation.
These efforts are beneficial to the awareness of disaster preparedness among medical facilities and healthcare workers,11 although there are slight disparities from region to region depending on economic development.12 Medical managers and staff are willing to expand their knowledge on disaster management and serve in future disaster situations.13 A survey conducted during December 2003 in the Japanese Tohoku and Hokkaido areas demonstrated that 68% of the hospitals that responded had sound resilience strategies covering multiple disasters and were equipped with alternative sources for critical utilities.14 In Japanese, the functional preparedness, except for structural, nonstructural, and human resources, could be fulfilled for the majority of the respondent hospitals, which was helpful during the emergency period of a disaster according to the lessons drawn from the Great East Japan Earthquake.15 Nevertheless, these disaster plans focused on responding to disasters rather than improving the resilience of hospital facilities.16
The functionality of hospitals was highly dependent on physical and human factors after earthquakes, including building damages of structural and nonstructural components, damages of utilities in hospitals and infrastructures outside hospitals, malfunction of medical equipment, emergency management, and staff.17-20 Recent seismic events have caused serious effects on hospitals. In the 2010 Chile Earthquake, design requirements for nonstructural components were rarely enforced, and the buildings, including hospitals, predating modern codes had not been upgraded to current standards.21 The 2010 Haiti Earthquake directly caused more than 200,000 fatalities, and 10 months later, Haiti was stricken by epidemic cholera, which caused 7436 deaths.22 The national medical systems were destroyed to the point of nearly total reliance on foreign medical teams for trauma care.23, 24 In the 2011 Christchurch earthquake, Christchurch Hospital exposed difficulties in communication and managing staff reporting for duty and tracking patient movement; structural and nonstructural components were damaged, sustained by power lost due to the intermittent cutting out of generators.25 Imaging and reporting pathways were constrained due to the lack of energy and lift access.26 Patient transfers among intensive care units, operating theaters, medical imaging, and the mortuary were limited because of out-of-use elevators.27 Surgeons, as core units, found it difficult to continue operations during earthquakes because of tremors, power outages, and equipment malfunction.28 During the 2012 Varzaghan–Ahar twin earthquakes in Iran, severe damages to the columns and beams, ceilings, and walls were found in Heriss and Ahar hospitals and this forced the medical services to be performed at the temporary hospitals set up in tents.29 After the Kumamoto earthquake, approximately one-third of the hospitals in the affected area reported loss of functionality due to equipment inoperability and supply interruption, and 15% of the healthcare functionality in stricken regions was lost. Twenty-three hospitals (approximately 20%) reported evacuation of patients due to damage to buildings, critical systems, and equipment.30 Achour et al.31 proposed that vulnerability of infrastructure, the low performance of alternative sources, and lack of consideration of healthcare utility supplies in resilience codes and legislations were the three significant challenges in the face of natural hazards for hospitals. An investigation on the damage to 34 healthcare facilities in seven countries caused by nine earthquakes between 1994 and 2004 conducted by Achour et al.32 showed that the structural and architectural damages tended to be different. However, the damages of utility supplies and equipment showed similar trends.
The concept of resilience has recently received considerable attention in disaster prevention and mitigation. It addresses the complexity and interdependences of systems and focuses on the variability during disaster situations, which provides a new perspective and a viable implementation path for understanding hospital systems under earthquakes. The definition of seismic resilience, the selection of evaluation criteria, and the establishment of an assessment model are considered critical issues in this domain.33 Bruneau et al.34 defined resilience as the ability of a system to reduce the chances of a shock, to absorb a shock if it occurs (abrupt reduction of performance), and to recover quickly after a shock (re-establish normal performance). Resilience was expected to involve technical, organizational, social, and economic dimensions. Specifically, technical resilience refers to the performance of physical systems in disasters, and organizational resilience indicates the capacity of organizations to make appropriate decisions and take practical actions. The Multidisciplinary Center for Earthquake Engineering Research (MCEER)35 proposed a comprehensive definition of community resilience as the ability of social units to mitigate hazards, contain the effects of hazard-related disasters when they occur, and carry out recovery activities in ways that minimize social disruption and mitigate the effects of future hazards. The definition clarified that enhancing disaster resilience aims to minimize any reduction in quality of life through emergency response (including loss of life, injuries, and economic impacts) and enable communities to return to levels of predisaster functioning or acceptable levels rapidly as possible. These make the definition particularly applicable to infrastructure systems for assessing resilience.
Xie and Zhang36, 37 conducted in-depth research on disaster prevention and mitigation at the city scale and pioneered the concept of city capacity for earthquake disaster reduction in 2001. They proposed a framework for earthquake disaster risk evaluation using seismic casualty, economic loss during earthquakes, and the time required for recovery after an earthquake as the primary criteria. Six components that could affect the above elements and overall ability were considered as follows: seismic hazard analysis capacity; seismic monitoring and forecasting capacity; engineering performance; political, economic, and human resources (city administrative level, GDP per capita, population age distribution, etc.); nonengineering factors such as laws and regulations, emergency plan, and public awareness of disaster reduction, etc.); and the ability to provide emergency relief and assistance (command communication, medical treatment, firefighting, emergency water, and power supply and repairers, stuff storage, settlement, and accommodation, etc.). Recently, Fang et al.38 viewed a city as a system of systems in physical–societal–cyber spaces (named as trio spaces). The subsystems of a city (infrastructures, buildings, healthcare systems, transportation systems, government administration, and communication systems) and their interactions were the connotation and properties of urban resilience.
A growing body of literature has recognized the importance of hospitals for communities subjected to earthquakes. Moreover, the trends have led to a proliferation of reviews that focus on hospital resilience. Fallah-Aliabadi et al.45 reviewed publications related to hospital disaster reduction and identified the lack of studies substantially related to structural and nonstructural components of hospitals. Systematic efforts were made to identify and collect factors and indicators mentioned in different studies. Then, they were categorized into three domains (constructive, infrastructural, and administrative) and 27 subdomains. Ali et al.46 critically examined publications related to hospital resilience during disasters and found deficiencies in disaster-related plans for staff awareness, education, and training. The importance of infrastructure and organization for resilience was emphasized. Carrington et al.47 studied the impact of natural disasters on health resources within emergency departments from four priorities encompassed in the Sendai Framework for Disaster Risk Reduction 2015–2030. Although extensive research has been carried out on hospital disaster resilience, few reviews exist that focus on the assessment methods for hospitals, especially those subjected to earthquakes. There is little consensus regarding which measures should be selected and how to include these measures in a comprehensive framework for hospital resilience assessment.
An objective of this study was to contribute to this growing area of research by reviewing the assessment measures and methods and providing suggestions for further development. This paper has been divided into three parts. The first part begins by laying out the composition and organizational purpose of a hospital and summarizes the definitions of hospital resilience. The second part reviews the resilience assessment methods under earthquakes and classifies them into two general categories: indicator-based and functionality-based. The third part discusses the definition of hospital resilience and the current methods of seismic resilience assessment for hospitals in influencing factors, performance measures, and tools. It is hoped that this study will contribute to an in-depth understanding of the hospital resilience assessment methods subjected to earthquakes for disaster committees, hospital managers, and staff.
2 HOSPITAL RESILIENCE DEFINITION
Hospitals are defined as the medical institutions licensed by laws that provide continuous medical care for sick and injured persons. Multiple building functions are integrated into hospitals, such as hotels (inpatient department), office buildings (medical staff, logistics, and administration), laboratories (medical engineering), and warehouses.48 Figure 2 shows a schematic diagram of the composition of a hospital system. A hospital system usually consists of physical parts, patients and staff, and an organization. Structural systems, architectural and protective components, and supplies (e.g., electrical and water systems, heating, ventilation, air-conditioning [HVAC], medical gas systems) form the physical parts of the hospital. The entities in the system include patients, medical staff (such as doctors and nurses), and administrators. The disaster response and capacity surge would benefit from volunteers.49 Finally, designed organizations establish the connection between physical parts, patients, and staff. A hospital system would be able to have the functionality of treating patients. The severity-based treatment process is one of the most used hospital organizations for emergency and disaster response. Usually, a patient would be first graded and assigned a color code related to the severity to achieve efficient treatment. The red, yellow, and green colors represent emergency, urgency, and minor urgency. Patients with different color codes would be sent to various departments for examination or treatment according to their needs. In a hospital, departments are usually seen as the basic units, and according to their functions, they can be divided into four categories: medical, diagnostic, patient support, and overhead.50 Some studies selected critical departments (such as emergency departments51-53) to be analyzed as representatives of the multiple hospital functions. In addition to receiving new-arrival patients, as open systems, hospitals need to replenish materials, supplies, and medical resources (medical equipment, devices, and human resources47) from environments to maintain functional operations.
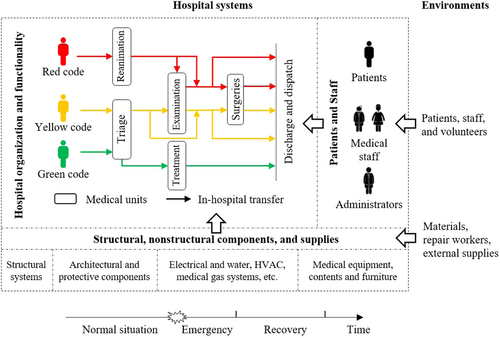
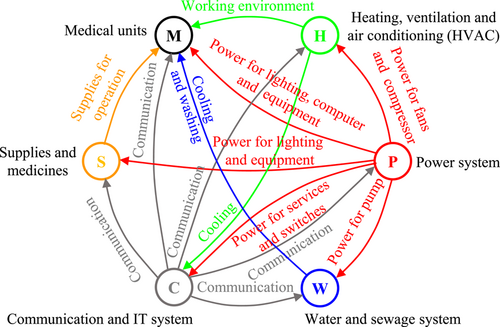
A high level of interconnections, dynamism, and technological innovation are the essential characteristics of hospital operations.54 In practice, patients and victims go through a sequence of hospital departments according to their treatment acquirements.55-58 The relationship and interconnections are brought to the fore between departments, external supplies and services, and internal processes, as shown in Figure 3. The arrows between different components represent dependencies. For example, electricity is required for switches in the communication system, fans, HVAC systems, lighting, and electronic equipment during hospital examinations and treatment. The interrelationships could improve hospital operational efficiency and save costs, but under external impacts (such as earthquakes), they are likely to lead to low redundancy and a high risk of a system crash. Deficiencies and losses in any functional aspect may make the entire hospital function at a reduced level or even lead to a crisis. The continued functioning of hospitals relies on safe structures that can resist exposures and forces from disasters, medical equipment in good working order, continued community infrastructure and critical services, and emergency and disaster management capacities.3 For the hospitals affected by earthquakes, they may need to undergo time-consuming and resource-intensive recovery processes to restore their functionality to a target level (equal to, above, or below the original state).59 The recovery plans and resources are expected to significantly affect the rapidity of recovery and, together with the robustness of systems, determine the resilience of hospitals.
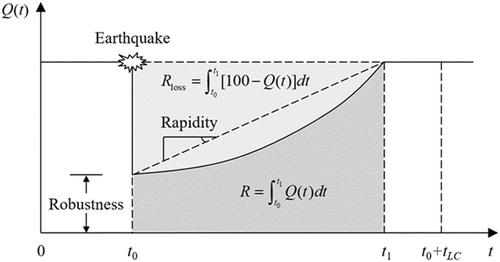
The definition of hospital resilience was widely debated in light of its importance for resilience assessment. Substantial efforts have been devoted to defining and describing hospital resilience from different perspectives. Bruneau et al.42 applied the concept of community seismic resilience in engineering to hospitals. Two quantification options for resilience were innovatively proposed: the quality of life after earthquakes and the ability of hospitals to provide an intended function for patients. The former is a significant measure for policymaking, while the latter involves multiple government agencies and individual hospital owners. Zhong et al.60 described hospital resilience as hospitals maintaining their prime functions to resist, absorb, and respond to the shock of a disaster and then restore to its original state or a new state. Vugrin et al.61 recognized hospital resilience as the capacity of a hospital to respond and its effectiveness during a disaster. Olu62 believed that a resilient system should prepare for, withstand the stress of, and respond to the public health consequences of disasters successfully from the health aspect. Barrera63 defined hospital resilience as inherent disaster resilience and adaptability to disasters, retaining essential functions. Wiig et al.64 focused on high-quality care, defining hospital seismic resilience as the primary function in response to sudden increases in demand and providing emergency medical services for patients. Shahverdi et al.65 proposed that resilient healthcare systems must provide their patients with services during disasters nearly similar to those provided in normal situations. The above diverse definitions of hospital resilience have been proposed for general disasters or earthquakes. In the main, they are consistent with the definition for a general system proposed by Bruneau et al.34 Unlike other studies, Bruneau et al.42 considered the demand of engineering practice and different assessment subjects, specified hospitals' functionality, and selected quantifiable measures, which would be one of the most important references for the resilience definition for hospitals subjected to earthquakes.
3 RESILIENCE ASSESSMENT METHODS
A more reasonable and reliable assessment of hospital resilience has long been a goal of tremendous interest in many fields, including earthquake engineering. The resilience assessment methods are at the heart of designing and achieving earthquake-resilient hospitals and communities. The assessment results could provide a critical reference for goal setting, emergency plan setting, facility design, and enhancement. A good summary and analysis of existing methods can be conducive to identifying existing research gaps and providing suggestions for future research.
Depending on whether or not functionality curves are adopted during assessments, the assessment methods for hospital resilience subjected to earthquakes can be divided into two main categories: indicator-based and functionality-based.56, 66 Indicator-based methods assess resilience by summarizing a rich set of indicators (understood as factors affecting resilience) from different dimensions or aspects of hospital disaster preparedness. Qualitative or quantitative values would be assigned to these indicators based on specific criteria, and then a total resilience indicator could be obtained through integration, though some of the measures adopted in functionality-based methods are similar to the indicators or domains in indicator-based methods. Functionality-based methods are characterized by using functionality curves in the assessment process to describe functionality changes in hospitals and summary metrics to quantify resilience.34
3.1 Indicator-based methods
Multifaceted impacts from technical, organizational, economic, and social aspects caused by earthquakes would be imposed on hospitals due to physical damages, confusion, disorder, supply and communication disruptions, and surge in casualty numbers.43, 67, 68 A straightforward and uncomplicated idea is to evaluate the dimensions or factors included in hospital resilience separately to achieve a comprehensive and detailed assessment. The indicators from different dimensions could also be aggregated to coordinate managers, directors, and stakeholders.
The most representative and widely used indicator-based method is the Hospital Safety Index (HSI),3 recommended by the Pan America Health Organization (PAHO) and the World Health Organization (WHO) for the assessment of hospital functional ability. It includes a safe hospital checklist with four sections or modules: (1) hazards affecting the safety of the hospital and the role of the hospital in emergency and disaster management; (2) structural safety, including previous events and hazards affecting structural safety, building integrity; (3) nonstructural safety, including architectural safety, infrastructural protection, access, and physical security, critical systems, and equipment and supplies; and (4) emergency and disaster management, including coordination of emergency and disaster management activities, hospital emergency and disaster management response, and recovery planning. Each item (total 151 items) in these modules has three levels of safety (high, average, and low) applied with different constant values, and a significant number of trained and experienced independent experts with different professional backgrounds are needed during the evaluation. The overall hospital safety index would be calculated from the module and safety index calculator, assigning weighted values to each item, section, submodule, and module. For example, the weighting of the modules has two models. One is 50%, 30%, and 20% for structural safety, the nonstructural module, and the nonstructural module, suitable for hospitals with a high risk of earthquakes; the other is that all modules are assigned equal weight. The calculator results (safety index) for each module and the overall hospital would then be assigned a classification of recommendations related to the intervention. Compared to detailed vulnerability studies, the HSI has the advantage of time and cost for a single evaluation and has been identified as an effective and authoritative tool to assess the safety of hospitals around the world.69-72 Expert reliance and time-consuming are the disadvantages to be overcome for future development.73 It should be pointed that the meaning of the term “safe hospital” in this approach, “a facility whose services remain accessible and functioning at maximum capacity, and with the same infrastructure, before, during and immediately after the impact of emergencies and disasters,” indeed contains high expectations and requirements of hospital performance under disasters from countries and other stakeholders. Furthermore, this can be interpreted as a goal for hospitals to design, build, and enhance resilience.
Zhong et al.5, 60, 74-76 conducted a comprehensive and in-depth series of studies on hospital disaster resilience evaluation, including the definition, conceptual resilience framework, measurement approaches, and surveys. Four domains were identified as follows, which were aggregated to incorporate all the hospitals' fundamental capacities to cope with disasters and influence the four dimensions (robustness, redundancy, resourcefulness, and rapidity)34: (1) hospital safety and vulnerability; (2) disaster preparedness and resources; (3) continuity of essential medical services; and (4) recovery and adaptation. The resilience evaluation was conducted top-down in the order of dimensions, domains, subdomains, and measures.60 The framework was then converted into a questionnaire using dichotomous indicators in a cross-sectional survey of tertiary hospitals for disaster resilience.5 The survey developed the framework through three rounds of modified-Delphi consultation and identified eight domains, 17 subdomains, and 43 indicators.74 The data relating to the eight domains of interest were collected and analyzed: (1) hospital internal safety; (2) emergency leadership and cooperation; (3) disaster plan; (4) disaster stockpile and logistics management; (5) emergency staff; (6) emergency critical care capability; (7) training and drills; and (8) disaster recovery mechanism. Each question in the questionnaire had two options (yes or no) and assigned scores (1 or 0). A total score representing the hospital resilience was calculated by summing the scores across all eight domains. Four key factors ([1] hospital disaster medical care capability; [2] hospital disaster management mechanism; [3] hospital disaster resources; and [4] hospital safety) were extracted from the eight domains through factor analysis to represent the overall level of disaster resilience capability to achieve the goal of reducing the number of variables included in the hospitals' resilience analysis. It is needed to sum the scores in each domain, determine the factors by a linear combination of the scores, and finally obtain the resilience indicator by a linear combination of the factors.5, 76 Cimellaro et al.77 conducted a similar survey to study the disaster resilience of tertiary hospitals in the San Francisco Bay area. In the survey questionnaire, thirty-three questions are listed and grouped into the same eight domains like those domains used in the literature.74
The number of factors was reduced to three. In the studies,76, 77 the quartile (25%–75%) was used to categorize the levels of the overall resilience score. Table 1 lists the data extraction, domains, and resilience-level categorization.
| Authors | Tool types (question number) | Scaling | Domains, modules, or dimensions | Resilience-level categorization |
|---|---|---|---|---|
| WHO3 | Checklist (151) | Low, average, and high | Hazards affecting the safety of the hospital and the role of the hospital in emergency and disaster management, structural safety, nonstructural safety, emergency, and disaster management. | 0.35–0.65 |
| Zhong et al.5, 74 | Questionnaire (56) | Yes or no | Hospital safety, disaster leadership and cooperation, disaster plans, disaster stockpiles and logistics management, emergency staff, emergency trainings and drills, emergency critical care capacity, recovery mechanism. | 0.25–0.75 |
| Cimellaro et al.77 | Questionnaire (33) | Yes or no | The same as Zhong et al.74 | |
3.2 Functionality-based methods
The usage of functionality curves in the resilience assessment is the identifying feature of functionality-based methods. In the functionality-based methods, according to the definition of functionality curves proposed by Bruneau et al.34 (Figure 1), the vertical axis should be a performance measure that reasonably represents the desired hospital functionality. A corresponding calculation method is needed, yielding the measured change during the emergency and recovery process. The resilience quantification needs summary metrics to map these curves as a single value. The functionality-based methods need to consider all the factors that influence the hospital performance.
Recently, Poulin et al.44 reviewed the publications that used resilience curves as tools in resilient infrastructure assessment and summarized a common vocabulary and taxonomy for resilience curve measures and summary metrics. The classification of performance measures was adopted in this study and, in order of increasing modeling complexity, the performance measures are classified into three detailed categories: (1) availability (capacity or aggregated function of the system); (2) productivity (quantity of service provided by the system); and (3) quality (nature of the service provided by the system). Table 2 lists the categories of performance measures48 and their adapted meaning for hospital resilience assessment. Each category is analyzed in terms of its description, analysis focus, modeling scope, nominal, and potential stakeholders.
| Availability | Productivity | Quality | |
|---|---|---|---|
| Description | Capacity or aggregated functionality of hospitals | Quantity of service provided by hospital systems | The nature of services provided by systems |
| Analyze focus | Hospital systems themselves | Provision of medical services | The utilization of medical services |
| Modeling scope | Primarily focused on hospital systems | Includes representation of service demand | Includes representation of service demand |
| Nominal | Full function | All service demands met | Typical or steady-state values may provide a reference, but not a bound |
| Potential stakeholders | Hospital operators, public healthcare departments | People, public health officials | Department heads, municipalities, peoples |
| Example | Emergency functionality availabity43 | Treatment capacity34 | Waiting time40 |
Besides the three categories, hybrid-type measures (such as quantity and quantity79) were found during this literature review. Hybrid measures are expected to overcome the limitations in the assessment dimension serviced stakeholders caused by a single measure. As a combination of availability, productivity, or quality, the hybrid measures are not included in Table 2. Meanwhile, some methods do not highlight the functionality of hospitals and use generic measures during resilience assessment, such as economic loss and repair cost,41, 80, 81 social loss,41 and usable space in buildings.82
3.2.1 Availability
After earthquakes, total or partial hospital functionality availability is a significant concern for hospital operators and public healthcare departments. It focuses on the macrostate of hospital systems themselves, but not the end-use of the service provided (e.g., earthquake-induced injuries), making it suitable for stakeholders indifferent to the medical demand and resource utilization. Physical damages in the engineering area are crucial for the assessment methods using availability measures. Fault tree (FT) analysis83 is a common used analysis tool. FTs can represent the combinations of primary failure and malfunction events that are not desirable in systems and for modeling the system interaction (Figure 3), and failure propagates from components to service through hospital systems. For example, in the seismic risk assessment of the Montréal hospital,84 FT analysis played a vital role in quantifying the consequences of component failures on the functionality of HVAC and life support systems. The analysis of the functionality-based methods for hospitals resilience assessment is listed in Table 3.
| Category | Authors | Measures | Tools | Summary metrics | Factors | Earthquake damages | Phases | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Physical | Staff | Organizational | Emergency | Recovery | ||||||
| Availability | Jacques et al.43 | Resilience metric | FT | - | √ | √ | × | √ | √ | √ |
| Yu et al.85 | Functionality levels | FT | Integral | √ | × | × | √ | √ | √ | |
| Shang et al.79 | Treatment path ratio | ST | Integral | √ | × | × | √ | √ | √ | |
| Productivity | Khanmohammadi et al.86 | Dimensionless waiting patients | SD | Integral | √ | √ | √ | √ | √ | √ |
| Li et al.66 | Treatment ratio | SD | Integral | √ | √ | √ | √ | √ | √ | |
| Quality | Cimellaro et al.40 | Normalized waiting time | DES & metamodel | Integral | √ | √ | √ | √ | √ | √ |
| Cimellaro et al.58 | Waiting time | DES & metamodel | - | √ | √ | √ | × | √ | × | |
| Niazi et al.51 | Waiting time | DES | Integral | √ | √ | √ | × | √ | × | |
| Hybrid | Cimellaro et al.87 | Product of quality and quantity | DES | - | √ | √ | √ | √ | √ | × |
| Hassan et al.87 | FT | - | √ | √ | √ | √ | √ | × | ||
| Hassan et al.87 | FT | Integral | √ | √ | √ | √ | √ | √ | ||
| Zhai et al.56 | Successful treatment ratio | FT & DES | - | √ | √ | √ | √ | √ | - | |
- Abbreviations: DES, discrete event simulation; FT, fault tree; SD, system dynamic.
3.2.2 Productivity
3.2.3 Quality
The presentation of quality measures reflects higher requirements on hospitals subjected to earthquakes beyond their availability and productivity. Quality measures are widely used in hospitals' daily performance appraisals, which department heads and municipalities are concerned about, and they correlate with people's treatment outcomes and satisfaction.93 Discrete event simulation (DES) was a critical technique to simulate treatment processes and calculate the measures to evaluate the hospital's performance after earthquakes. DES is skilled at modeling systems with typical queuing behavior (such as treatment processes) and is widely used in healthcare.94-97 It is called “discrete” because the state changes only co-occur as events occur, while the system states remain constant at other times.
In the study,58 WT was identified as the measure to evaluate the resilience indicator of an emergency department. The DES model of a hospital located in California87 was updated by a DES model of the emergency department in a hospital located in Italy, which was able to take into account the hospital resources, the emergency rooms, the circulation patterns, and the patient codes (red, yellow, and green). Furthermore, the number of parameters in the metamodel was reduced from three to two (the seismic input and the number of the available emergency rooms). Niazi et al.51 conducted a study that used DES to calculate the WT as the performance measure of resilience assessment for Imam-Khomeini hospital built in Tehran. In the studies,51, 58 the structural and nonstructural components were assumed to remain undamaged, or their influences on hospital functionality were ignored. The patient arrival rates collected by a Californian hospital during the 1994 Northridge Earthquake were scaled for the WT caculation in References [51, 58, 87]. Favier et al.99 developed an assessment framework for an emergency department from seismic risk, and the total waiting time during a period was adopted as the hospital performance measure. Novel efforts were made to integrate physical damages and caused loss of functionality. In detail, the impacts of damage were first reflected in the reduced number and downtime of hospital rooms and then in the functionality of the emergency department.
3.2.4 Hybrid
4 DISCUSSIONS
4.1 Resilience definition
The concept of the resilience of hospitals is accepted as being of increasing importance, as the severe impact of disasters is becoming more of a concern. The resilience definition of hospitals has developed from a single feature or dimension to multiple dimensions. According to domains or perspectives, the definition can be classified into social, organizational, and physical resilience.102-104 Organizational resilience uses administrative and operational procedures to implement interventions to reduce the adverse impact of seismic hazards and quickly respond to hazardous events.104 Physical resilience focuses on the performance of structural and nonstructural components.42 The TOSE dimensions of community resilience proposed by Bruneau et al.34 included technical, organizational, social, and economic dimensions. It also takes into consideration the economic dimension, which refers to the capacity to reduce both direct and indirect economic losses resulting from earthquakes.
Resistance, adaption, and restoration constitute the three phases of resilience in the time dimension. Resistance represents a phase in which hospitals withstand damages and disruptions when earthquakes occur. In the adaption phase, hospitals are expected to make optimal use of existing and alternate resources to maintain hospital functions and attempt to generate a booming treatment capacity for earthquake casualties. The first two phases are collectively referred to as the emergency phase. The recovery from a disruptive event is included in the restoration phase, and its purpose is to recover quickly at a reasonable cost. In the studies [101, 105], resilience was defined as the ability to resist unexpected challenges and the flexibility to restore to normality. The sudden increased demands for treatment were neglected, and emergency management was not included. Literature [106-108] regarded hospital resilience as the capability to withstand the event and cope with sudden increased patient influx with continuous provision of medical service, while the recovery phase was not emphasized. Understanding the definition of the seismic resilience of a hospital from the adaptive perspective helps improve the level of emergency medical services.109
4.2 Indicator- and functionality-based methods
As an open question, the resilience assessment of hospitals has attracted the attention of researchers and managers. A variety of studies on this topic provide a wide range of options and paths. As stated above, the seismic resilience of hospitals is influenced by many factors, and a reliable and accurate assessment method should take all factors into account and provide the values of resilience that are of interest to stakeholders. Moreover, the methods are also expected to be simple, quick, and low cost.
Though both indicator- and functionality-based methods can assess the seismic resilience of hospitals, there are several essential differences in the process and results. The numerous factors can be listed in the indicator-based methods and are usually categorized into several dimensions (physical, organizational, etc.) or domains. The complexity of hospitals and the multidimensional nature of the resilience concept can be fully reflected. Meanwhile, the trend of an increasing number of domains and indicators is observable (see Table 1), which represents an effort to capture and encompass as many factors as possible that can impact hospital resilience. Such methods cannot be implemented without a team of experts to score each question of questionnaires or checklists,73 thus inevitably introducing human bias and subjectivity. Based on the qualitatively assigned scores for the options of questions (yes or no,5 or high, average, and low3), the overall resilience index was obtained by summation and weighted summation. The mechanisms and mathematical modeling of the operation of hospitals subjected to earthquakes are not the point of interest for the indicator-based methods. Further studies with more focus on the values of scores, weighting of different domains, and the summation algorithm for the resilience index, and resilience-level categorization are suggested. For example, hospitals are complex systems, including multiple interactions between internal and external components. Using the summational algorithm to model the relationship between influencing factors and the resilience index would be an interesting topic that could be explored in further research. As for the assessment results, the resilience index from the indicator-based methods is a relative value that can provide a relative level of resilience,36, 37 which can compare hospitals or judge whether a hospital achieves an expected level.
In the functionality-based methods, the critical steps are to select or define functionality measures and plot resilience curves. Unlike the indicator-based methods, which require indicator lists and surveys, the functionality-based methods commonly select only one measure that attracts the interest of potential stakeholders. They could provide more details on the change of the performance measure over time after earthquakes. The formula-format definitions of performance measures and hospital resilience facilitate the adoption of system analysis and simulation tools. General recommendations for selecting appropriate measures are lacking in the literature in a broad context, including hospital resilience.44 A common problem with the functionality-based methods is that only a single measure (availability, productivity, or quality) is adopted in the resilience assessments, which ignores the richness of the resilience concept and interests of potential stakeholders. Bruneau et al. had focused attention on the fact that a single measure could not present the system functionality42 or capture all the characteristics of the functionality curve in the evaluation of system resilience.110 Hybrid measures, a product of quality and quantity87 and successful treatment ratio,56 may solve this problem.
FT and system simulation tools, including DES and SD, are commonly used in functionality-based methods. The simulated results of the DES model were used to calibrate the parameters of double-exponential functions, named metamodels in References [40] and [58]. Available interrelationships between components in hospitals and external utilities can be represented, and the impact of factors and their relative importance can be quantified and identified using the tools. Besides, there are high correlations between performance measures and tools. SD and DES were applied to calculate productivity and quality measures of hospitals, respectively. At the same time, FT (ST) was commonly used to judge the availability of hospital functionality and could be combined with DES to calculate the hybrid measures. However, compared to indicator-based methods, many factors cannot be considered in the functionality-based methods due to lack of data or essential research support. Assumptions and simplifications are inevitably required, such as that building components remain undamaged under earthquakes.58 Further studies, which take the factors that have been proposed in the indicator-based methods into account, will need to be undertaken.
A striking observation from the literature review (Table 3) is that almost all studies used the integral values as summary metrics to obtain the resilience from functionality curves. There are implicit assumptions that the hospital performances are valued equally at every point in time. Bruneau et al.42 gave two examples of resilience curves with same lack area (a total loss for 2 days and 10% loss for 20 days) to illustrate the nonlinearity of the resilience concept. Although the best case is that no degradation of functionality occurs, service providers and customers may choose different preferred cases based on their concerns. For example, the 10% loss for 20 days may be a preferred scenario compared to a total loss for 2 days that most customers are not adversely affected at the cost of loss of service to a small base. For the resilience assessment, it is essential but challenging to reflect the values and goals of stakeholders across all systems and achieve a balance. Use of multiple performance measures reflecting different stakeholders and assignment of linear or nonlinear weighting driven by spatial or temporal variations are promising solutions.111
Recovery is an indispensable part of the resilience definition. The approaches to how recovery is reflected in resilience assessment methods and results are different. In indicator-based methods, the recovery-related indicators would be integrated into a module (such as a recovery mechanism5, 74) to reflect the role of recovery in resilience. However, in functionality-based methods, recovery is usually regarded as one of the essential phases of resilience in the time dimension. Functionality curves, including recovery phases, are needed to obtain the summary metrics. The values of functionality measures must be evaluated as recovery processes are performed. During recovery phases, the states of components in hospitals could be obtained through surveyed data43 or the results of recovery path analysis.79 Besides, FEMA P-5888, 89 provided a method to estimate repair periods with parallel and serial repair strategies. It should be noted that, though partial studies listed in Table 3 do not include the recovery phases, they also have the potential to undertake the functionality assessment during recovery phases.
5 CONCLUSIONS
- 1.
There are four main perspectives of resilience definition: physical, organizational, social, and economic dimensions. Resistance, adaption, and restoration should be included in the time dimension of hospital resilience.
- 2.
The current assessment methods are divided into two main categories, indicator-based and functionality-based, depending on whether or not functionality curves are adopted. Performance measures for quantifying the functionality of hospitals are classified into four categories: availability, productivity, quality, and hybrid.
- 3.
The indicator-based methods can include numerous factors that affect hospital resilience. The complex components of hospitals and the multidimensional nature of the resilience concept can be fully reflected. However, further studies are urgently needed on the values of scores, the weighting of different domains, the summation algorithm for the resilience index, and resilience-level categorization.
- 4.
Functionality-based methods are limited in number and variety compared to indicator-based methods. The relationship between components can be mathematically represented, and an absolute value of resilience could be obtained. The assessment methods using hybrid measures could combine at least two kinds of performance characteristics, which become suggested choices to reflect different stakeholders' values and achieve a balance.
- 5.
There are high correlations between performance measures and tools. FT and system simulation tools, including DES and SD, are the most frequently used tools. Integration of functionality curve is the dominant method for calculating summary metric in current studies.
These findings have significant implications for interpreting similarities and differences between indicator- and functionality-based methods. It is hoped that researchers and managers can understand and learn more about both methods. The scope of this study is limited in terms of individual hospitals; future studies on hospital networks, healthcare systems, and community assessment are recommended. The issues not addressed in this study include the analysis of data requirements, assessment speed, and validation of the results.
ACKNOWLEDGMENTS
The contribution of Cheng Zhang of Harbin Institute of Technology to the preparation of this work is gratefully acknowledged. This investigation was supported by the National Natural Science Foundation of China (No. 51938004, 51825801, and U1939210), the Natural Science Foundation of Heilongjiang Province (No. LH2021E075), and Creative Research Groups of the National Natural Science Foundation of China (No. 51921006).
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
Data supporting the study findings are available upon request.




