Postconcussive symptom severity, risk factors for prolonged recovery, and mental health history: Pathways of influence in a diverse pediatric sample
Abstract
Introduction
The objective of this study was to confirm previous risk factors for concussion recovery in a diverse pediatric sample and to elucidate the pathways by which individual mental health factors influence postconcussive symptom reporting and time to clearance.
Methods
Subjects between 13 and 17 years of age (N = 642; mean age = 15.40; 45% female) were analyzed from a prospectively completed database associated with a multidisciplinary TBI/concussion clinic in the southwest United States. Fifty-four percent of participants identified as Hispanic, 41% received medical coverage through Medicaid, and 54% were injured during participation in an organized sports team. Mediation analysis using a structural equational framework was employed to examine the significance of both direct and indirect effects from preinjury factors (e.g., prior concussions, female gender, history of migraines, anxiety, depression, attention-deficit/hyperactivity disorder [ADHD], and learning disorders) on postinjury symptom reporting (at baseline and visit 1) and time to clearance.
Results
Higher symptom reporting at baseline was significantly associated with history of anxiety, depression, ADHD, headaches, and female gender. Higher symptom reporting at visit 1 was significantly associated with baseline symptoms, female gender, and history of anxiety. Symptom scores at baseline fully accounted for the relation between history of depression and symptom scores at visit 1 and only partially accounted for the relation between history of anxiety and symptom scores at visit 1. Only history of anxiety indirectly contributed to greater days to clearance through higher symptom scores at visit 1.
Discussion
This study supports the concept that heterogenous experience following injury is influenced by preinjury factors and extends the generalizability of risk factors to a diverse sample of youth in terms of ethnicity, insurance status/type, and mechanism of injury. Anxiety and depression represent important noninjury factors that warrant considerable attention during concussion treatment and management.
Introduction
Concussion* has been conceptualized as a complex multi-level system,1, 2 and neurobehavioral outcomes following concussion are posited to depend on numerous biopsychosocial factors.3, 4 Approximately 12% of youths 12–17 years of age have experienced symptoms of a concussion in their lifetime,5 and among youths who sustain a concussion, approximately one-third experience symptoms persisting longer than 4 weeks.6 Previous research highlights the role of preinjury factors (e.g., prior concussions, migraines, sex, age, mental health, and neurodevelopmental disorders) in experience with and reporting of concussion symptoms as well as the need to parse out baseline differences in reporting from clinical outcome.7 The overlap with concussion-like symptoms experienced in daily life, variable sample sizes, and diverse methodologies have led to mixed findings regarding predictors associated with recovery.7 Further, these predictors rarely occur in isolation; more often than not, adolescents present with more than one associated risk factor. The current study builds on this previous research by using structural equation modeling to examine the unique, additive effects of each predictor on both baseline and postinjury symptom reporting when evaluated in the context of other associated factors.
Both injury and noninjury factors contribute to symptom severity and recovery following a head injury, with growing attention to mental health (e.g., anxiety and depression) as a noninjury factor that may exacerbate or prolong self-reported concussion symptoms.8-10 As time progresses following a concussion, the contribution of injury characteristics lessens and the contribution of noninjury factors becomes increasingly important.10, 11 This pattern is evident in recovery from sports-related injuries12 as well as other mechanisms of injury (e.g., motor-vehicle collisions and falls13). For children and adolescents, in particular, restrictions from normal activities for a prolonged period, both in school and extracurricular, may lead to less social interactions, a reduced quality of life, and depressed mood.14 Recent reviews of existing literature examining preinjury mental health and postconcussive outcomes have identified a need to pay greater attention to this relation among diverse samples of middle school– and high school–age populations and to better understand the mechanisms underlying this increased risk for poor outcomes.15, 16
Among an ethnically diverse subspecialty clinic sample made of up athletes and nonathletes as well as individuals with prolonged symptoms and more typical recovery trajectories, this study used path analysis to quantify the relations among multiple variables potentially related to outcome from concussion. Both direct and indirect pathways were tested to better understand how these factors influence baseline and postinjury symptom reporting as well as time to clearance.
Methods
Design and setting
The interdisciplinary TBI/Concussion Clinic is an outpatient clinic at a children's hospital with a level I trauma center. The team manages mild to moderate TBI in accordance with active rehabilitation principles based on the Centers for Disease Control and Prevention (CDC) guidelines for the management of mild TBI in children.17 Referrals include sports-related concussion from school athletic trainers, posthospital or emergency department discharge, or injuries managed by primary care physicians if patients are not recovering as expected. Clinic goals include estimating preinjury baseline functioning to assess individual recovery and clear children to return to high-risk activities once appropriate. The team includes specialized medical providers, athletic trainers, and neuropsychologists. Initial visits are focused yet comprehensive (2 h) with rapid assessment of developmental/academic history, current performance, risk factors for prolonged recovery, a validated symptom scale called the Post-Concussive Symptom Inventory (PCSI), neurological examination including balance testing, and neurocognitive screening. For predominantly Spanish-speaking families, the intake paperwork and history forms are provided in Spanish and visits are conducted with the aid of a certified hospital interpreter or bilingual provider. The patient completes a neurological assessment with the medical provider, balance testing with the ahletic trainer, and neurocognitive screening (either computerized or with a neuropsychologist, when appropriate). Interdisciplinary interpretation of all assessments directs an individualized plan of care focusing on active rehabilitation (e.g., symptom management, academic accommodations, and safe, noncontact physical activity). Based on CDC guidelines, an Acute Concussion Education (ACE) care plan is developed and shared with the nurse at the child's school. Follow-up care, including repeat neurocognitive screening, is also individualized based on the stage of recovery and needs of the child and family.
The Institutional Review Board at The University of Texas at Austin approved the prospective database collection of clinical information and the research review of clinical records. Patient data were extracted into a secure, deidentified research database following completion of clinical care.
Participants
Participants (N = 642) were adolescents aged 13.00 to 17.99 years who presented to a multidisciplinary TBI/concussion clinic in the southwest United States between July 2017 and February 2024. Inclusion criteria included: (1) received a Glasgow Coma Scale score ≥13, (2) had normal brain imaging findings or imaging not obtained, (3) presented to the clinic within 8 weeks of injury, and (4) followed through clinical recovery (e.g., not lost to follow-up). Participants with a neurological diagnosis (e.g., epilepsy) or specific developmental disorders (e.g., autism spectrum disorder or intellectual disability) were excluded. Although an interpreter or bilingual provider was present in approximately 15% of visits to facilitate communication with caregivers and family members, 98% of the adolescents were considered English proficient (e.g., receiving English-only school instruction).
Measures
Child demographics
Information on child demographics (e.g., age, race, ethnicity, sex, gender) was obtained from the medical record, including a detailed health intake form filled out by a parent/guardian at the initial clinic visit. Race was identified from predetermined categories consistent with the US Census survey. Ethnicity categories included Hispanic and non-Hispanic. Child gender was identified as male, female, nonbinary, natal male identified female, natal female identified male, and other. Two natal females who identified as male were included with their identified gender in the analyses (0 = male; 1 = female). Removing these two-patients did not significantly impact the strength, direction, or significance of pathways in the model and, thus, these participants were included in the analyses.
Preinjury factors
Parents/guardians provided information on past medical history (e.g., migraines, previous concussion), preexisting psychiatric diagnoses (e.g., anxiety, depression), and preexisting neurodevelopmental diagnoses (e.g., attention-deficit/hyperactivity disorder [ADHD], learning disorder [LD]) on a health intake form completed upon arrival to the initial clinic appointment. Clarification of responses were collected via a brief clinical interview with the patient and parent/guardian performed by a qualified medical provider and/or neuropsychologist. All variables were binary with the exception of prior concussions (0 = none, 1 = 1 prior, 2 = 2 prior, 3 = 3 prior, 4 = 4 or more).
Injury characteristics
Primary injury characteristics included date of injury, initial Glasgow Coma Scale, loss of consciousness, mechanism of injury, and number of days since injury. Information about injury characteristics were provided by the referring provider (e.g., primary care physician, emergency department) prior to the clinic visit and uploaded into the child's medical record for review.
PCSI
The PCSI is a developmentally appropriate, psychometrically strong concussion symptom scale for use with pediatric populations.18 Three aged-based versions of the PCSI (5–7 years, 8–12 years, and 13–18 years) were created for pediatric use. The adolescent version (ages 13–18) was used in the current study and consists of 26 items answered using a 7-point Guttman scale (0 = not a problem; 6 = severe problem). Physical (e.g., headache, nausea), sleep (e.g., fatigue, drowsiness), emotional (e.g., irritability, sadness), and cognitive (e.g., difficulty concentrating and remembering) symptoms were included. Adolescents rated both their preinjury symptom levels (baseline) and current postinjury symptom levels (visit 1) corresponding to the day of their clinic visit (e.g., symptoms experienced that day or the day before). Retrospective recall of preinjury ratings using the PCSI has been shown to be stable in children and adolescents over the first 3 months postinjury.19 Scores were summed within time points (e.g., preinjury ratings, current ratings), with higher scores indicating greater endorsement of symptom severity.
Time to clearance from visit 1
Determination of clearance to return to high-risk activities was considered from a functional concussion standpoint. This was a clinical decision made by the medical provider based on a compilation of factors, including injury factors, symptom reporting, neurological assessment, balance testing, and neurocognitive testing (when available). This variable reflects when a patient was cleared from a functional concussion standpoint. It does not consider time required for neurosurgical clearance following skull fractures or intracranial hemorrhage.
Analytic strategy
Preliminary analyses were performed to examine frequency and descriptive information for all study variables using SPSS version 29. Correlational analyses were run to evaluate the relation between PCSI baseline scores, PCSI scores at visit 1, number of days from injury to visit 1, number of days from visit 1 to clearance, gender, and six variables related to preinjury history (e.g., history of depression, anxiety, ADHD, LD, migraines, and prior concussions).
Hypotheses were tested using mediational analysis in a structural equational framework (SEM), an approach that offers numerous conceptual and statistical advantages over standard regression methods.20 Analyses were conducted in Mplus (Mplus v.8.421), and missing data were handled using full information maximum likelihood estimation. Given the variability evident across previous research,7 the inclusion of predictors was based on results of correlational analyses within this sample. Mediation of the effects of preinjury anxiety and depression on PCSI visit 1 score (through PCSI baseline score) and on days from visit 1 to clearance (through PCSI visit 1 score) were tested using bootstrap confidence intervals (BOOTSTRAP = 5000) to examine the significance of the indirect effects.22
Results
Preliminary results
Demographic information, injury characteristics, and descriptive statistics for primary study variables are presented in Table 1. A total of 642 adolescents, ages 13.00 to 17.99, diagnosed with concussion were included in the SEM model. Of the 642 patients, 45% identified as female, 54% identified as Hispanic, and 41% received medical coverage through Medicaid. Approximately half of the sample (54%) sustained their injury during participation in organized team sports. A preinjury history of anxiety and depression was reported by 29% and 15%, respectively.
| Full sample (N = 734) | ||
|---|---|---|
| Mean (SD) | Range | |
| Age | 15.40 (1.37) | 13–17 |
| # Days from injury to first clinic visit | 17.32 (11.72) | 0–56 |
| # Days from first clinic visit to clearance | 17.25 (17.63) | 4–118 |
| PCSI baseline score | 9.73 (13.02) | 0–89 |
| PCSI visit 1 score | 28.99 (26.48) | 0–122 |
| Percentage | |
|---|---|
| Gender | 45% Female |
| Race | 84% White |
| 10% Black | |
| 2% Asian | |
| Ethnicity | 46% Non-Hispanic |
| 54% Hispanic | |
| Interpreter use | 16% Yes |
| Insurance status | 8% Uninsured |
| 41% Medicaid | |
| 51% Private | |
| Mechanism of injury | 54% Organized team sports |
| 16% Blunt object to the head | |
| 10% Motor vehicle collision | |
| 9% Falls | |
| Preinjury history | 29% Anxiety |
| 15% Depression | |
| 19% ADHD | |
| 18% LD | |
| 16% Headaches/migraines | |
| 75% No prior concussions | |
| 16% 1 prior concussion | |
| 5% 2 prior concussions |
- Abbreviations: ADHD, attention-deficit/hyperactivity disorder; LD, learning disorder; PCSI, postconcussive symptom inventory
Based on results of correlational analyses (Table 2), history of anxiety, depression, migraines, and gender were included as predictors of PCSI baseline score, PCSI visit 1 score, and days from visit 1 to clearance. History of an LD and ADHD were included as direct predictors of PCSI scores at baseline. Prior concussions, PCSI baseline score, and PCSI score at visit 1 were included as predictors of days from visit 1 to clearance. PCSI baseline score was also included as a predictor of PCSI score at visit 1.
| PCSI baseline | PCSI visit 1 | Days since injury | Days to clearance | Gender | Dep. | Anx. | ADHD | LD | Headaches | |
|---|---|---|---|---|---|---|---|---|---|---|
| PCSI visit 1 | 0.59** | - | ||||||||
| Days since injury | 0.05 | 0.02 | - | |||||||
| Days to clearance | 0.14** | 0.50** | 0.06 | - | ||||||
| Gender | 0.24** | 0.31** | 0.09 | 0.18** | - | |||||
| Dep. | 0.42** | 0.29** | 0.07 | 0.09 | 0.18** | - | ||||
| Anx. | 0.41** | 0.36** | 0.08 | 0.16** | 0.34** | 0.50** | - | |||
| ADHD | 0.21** | 0.08 | −0.04 | −0.01 | −0.06 | 0.27** | 0.20** | - | ||
| LD | 0.15** | 0.06 | −0.001 | −0.03 | 0.02 | 0.14** | 0.09 | 0.31** | - | |
| Headaches | 0.38** | 0.21** | 0.14* | 0.15** | 0.15** | 0.27** | 0.27** | 0.04 | 0.06 | - |
| Prior concussions | 0.05 | 0.03 | 0.06 | 0.08 | −0.04 | 0.10 | 0.08 | 0.04 | −0.004 | 0.07 |
- Note: underlined p < 0.05.
- Abbreviations: ADHD, attention-deficit/hyperactivity disorder; Anx., anxiety; Dep., depression; LD, learning disorder; PCSI, postconcussive symptom inventory.
- * p < 0.01.
- ** p < 0.001.
Primary results
The SEM fit the full sample data well, χ2 (N = 642; df = 6) = 2.97, p = 0.81, CFI = 1.00, SRMR = 0.01, RMSEA = 0.00 [90% CI: 0.00, 0.03]). Standardized model results are illustrated in Figure 1. Higher PCSI baseline scores were significantly associated with a history of anxiety (β = 0.18, SE = 0.05, p < 0.01), depression (β = 0.22, SE = 0.05, p < 0.01), ADHD (β = 0.09, SE = 0.04, p = 0.01), and headaches (β = 0.24, SE = 0.04, p < 0.01) as well as female gender (β = 0.11, SE = 0.04, p < 0.01). Higher PCSI scores at visit 1 were significantly associated with higher PCSI scores at baseline (β = 0.51, SE = 0.04, p < 0.01), female gender (β = 0.15, SE = 0.03, p < 0.01), and a history of anxiety (β = 0.12, SE = 0.04, p = 0.01). A greater number of days from visit 1 to clearance was associated with lower PCSI baseline scores (β = −0.30, SE = 0.06, p < 0.01), higher PCSI scores at visit 1 (β = 0.64, SE = 0.05, p < 0.01), and a history of migraines (β = 0.11, SE = 0.04, p = 0.02).
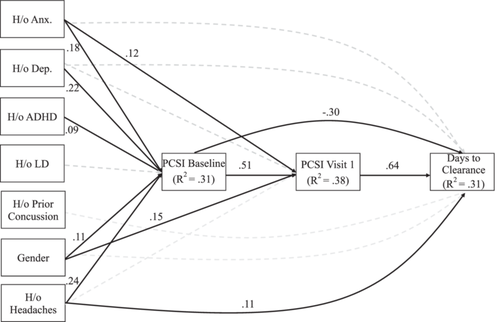
Based on results of the mediation analyses (Table 3), there was a significant indirect effect of history of anxiety and depression on PCSI score at visit 1 through PCSI baseline score. Meaning, PCSI scores at baseline fully accounted for the relation between history of depression and PCSI score at visit 1 and only partially accounted for the relation between history of anxiety and PCSI score at visit 1 (e.g., significant direct effect from anxiety to PCSI scores at visit 1). Only history of anxiety (b = 0.08) indirectly contributed to greater days to clearance by means of higher visit 1 PCSI scores.
| DV | Mediator | IV | Effect | Β (SE) | 95% CI | p |
|---|---|---|---|---|---|---|
| Days to clearance | PCSI visit 1 | H/o anxiety | ||||
| Direct | 0.01 (0.05) | [−0.08, 0.10] | 0.88 | |||
| Indirect | 0.08 (0.03) | [0.02, 0.013] | 0.01 | |||
| Total | 0.09 | |||||
| Days to clearance | PCSI visit 1 | H/o depression | ||||
| Direct | −0.01 (0.05) | [−0.10, 0.09] | 0.88 | |||
| Indirect | −0.01 (0.03) | [−0.06, 0.04] | 0.73 | |||
| Total | −0.02 | |||||
| PCSI visit 1 | PCSI baseline | H/o anxiety | ||||
| Direct | 0.12 (0.04) | [0.03, 0.20] | <0.01 | |||
| Indirect | 0.09 (0.02) | [0.04, 0.14] | <0.01 | |||
| Total | 0.21 | |||||
| PCSI visit 1 | PCSI baseline | H/o depression | ||||
| Direct | −0.02 (0.04) | [−0.10, 0.07] | 0.73 | |||
| Indirect | 0.11 (0.03) | [0.06, 0.16] | <0.01 | |||
| Total | 0.09 |
- Note: Standardized results are reported.
- Abbreviations: DV, dependent variable; H/o, history of; IV, independent variable; PCSI, postconcussive symptom inventory.
Post hoc analyses
Results of two-sided independent t-tests showed that adolescents with preinjury depression were seen in the specialty clinic during a similar time frame following injury (t(640) = −1.85, p = 0.07) and that it took approximately 4 additional days for this clinic to determine they were cleared to return to high-risk activities (t(640) = −2.40, p = 0.02) compared with their counterparts. Adolescents with preinjury anxiety were seen in the specialty clinic approximately 2 days later following injury (t(640) = −2.10, p = 0.04), and it took approximately 6 additional days for this clinic to determine they were cleared to return to high-risk activities (t(640) = −4.18, p < 0.01) compared with their counterparts.
Discussion
The objective of this study was to confirm previous risk factors for concussion recovery in a diverse pediatric sample and elucidate the pathways by which individual preinjury factors influence postconcussive symptom reporting (e.g., directly or indirectly). Through simultaneous examination of commonly associated risk factors, findings of the current study highlight unique, additive effects of preinjury factors on symptom reporting and concussion recovery. In particular, the unique contribution of mental health factors (i.e., history of anxiety or depression) remained meaningful when included among other known risk factors.
Factors associated with symptom reporting
Consistent with previous studies,23 a preinjury history of migraines, anxiety, depression, and female gender was associated with greater endorsement of postconcussive symptoms as well as longer time to clearance based on correlational and post hoc analyses. Given the diversity of this sample in terms of ethnicity, insurance status/type, and mechanism of injury, this study was able to provide a more socioeconomically balanced sample to answer questions posed about the generalizability of these preinjury factors across populations. The majority of the included risk factors for prolonged recovery were primarily associated with increased symptomatology at baseline (e.g., prior to injury). For clinicians, this emphasizes the importance of quantifying “baseline” (rather than “asymptomatic”) in order to determine when a patient has returned to their self-reported preinjury level of functioning. This estimation provides important context for interpreting the severity of postconcussive symptoms. For example, if the patient has a preinjury history of migraines and endorses headaches at baseline, similar endorsement of headaches postinjury would not be considered abnormal. A determination of “back to baseline” should be individually based and informed by injury factors and results of symptom reporting, neurological assessment, balance testing, and neurocognitive screening.
Evidence for the role of prior concussions on recovery from a subsequent concussion has been mixed, but more studies than not have been unable to substantiate the relation.7 Though associated with more days to clearance in isolation (e.g., correlational results), prior concussion was not significantly associated with days to clearance above and beyond the influence of other preinjury factors included in the model. In the context of influences from other preinjury factors, history of ADHD, but not an LD, was associated with increases in baseline symptom reporting. The lack of significant association between history of an LD or ADHD with time to clearance is consistent with the vast majority of previous empirical studies.7 These results speak to the importance of considering risk factors as a constellation rather than individually to better understand their relative importance for postinjury functioning and recovery.
The role of mental health factors
Rates of self-reported depression (15%) and anxiety (29%) among this sample of patients referred to a specialty clinic were higher than prevalence rates of diagnoses at the national level (6.1% and 10.5% for depression and anxiety, respectively; Ghandour et al.24). However, current study rates are consistent with reports of lifetime prevalence rates of depression (14%) and anxiety (32%) among adolescents ages 13–18 years.25 Previous studies have similarly reported elevated rates of preinjury mental health disorders among a specialty concussion population.26
In the present study, inclusion of mental health factors as primary predictors and simultaneous evaluation with other known risk factors (e.g., one statistical model) allowed for a better understanding of their relative strength as a unique predictor (e.g., above and beyond the influence of other factors). The benefit of the path analysis SEM model allowed for simultaneous consideration of all risk factors without a priori determinations of hierarchical processes. The association between history of anxiety and/or depression on baseline reporting of PCSI symptoms further emphasizes the overlap in symptomatology. For example, fatigue, sadness, feeling slowed down, and difficulty concentrating can all be associated with mental health status without the presence of a head injury.
The previous inclusion of mental health variables in relation to symptom recovery among pediatric populations has primarily been descriptive,15 which precludes the evaluation of shared variance and relative importance of anxiety and depression. Results of the current study show a direct relation between anxiety and PCSI score at visit 1, above and beyond the influence of anxiety on a higher baseline score. In contrast, depression was significantly and directly related to PCSI scores at baseline but not at visit 1. This difference highlights the unique influence of preinjury anxiety on postconcussive symptom experience above and beyond that of depression. Preinjury history of anxiety had larger total effects across the model than depression, which is consistent with prior work documenting significantly higher rates of preinjury anxiety, but not depression, in a mild TBI population compared with national norms.26 High levels of anxiety may lead to hypervigilance and subsequent overinterpretation and misattribution of benign bodily sensations following concussion (e.g., somatization), which, in turn, elevates report of symptoms and prolongs recovery.
Pathways of influence to clearance
A preinjury history of headaches/migraines demonstrated direct effects on baseline PCSI and was the only preinjury factor with a significant direct effect on days to clearance. Headaches, similar to symptoms of anxiety and depression, are another nonspecific symptom associated with concussion that can be maintained by multiple contributing factors (sleep, stress, predisposition/family history, etc.). These findings were consistent with previous literature describing that history of headaches is a common factor associated with prolonged symptoms.27 Higher PCSI scores at visit 1 were strongly associated with a longer time to clearance, which is also consistent with previous findings that higher acute symptom ratings are associated with longer recovery time.12 As expected, higher PCSI baseline scores predicted higher PCSI visit 1 scores, but baseline PCSI scores were inversely related to days to clearance. This secondary finding likely reflects that individuals who report few to no symptoms at baseline (e.g., no endorsement of headaches) may take longer to return to their preinjury level of functioning compared with individuals for whom aspects of the postconcussive experience, as captured on the PCSI, are a part of their normative daily experience. Additional investigation and replication of this finding is warranted.
History of both anxiety and depression indirectly contributed to a greater number of days to clearance, emphasizing the importance of considering noninjury factors as integral to concussion management and treatment. Practical implications include routine screening for past and current symptoms of anxiety and depression during clinic visits. If present, this information can influence treatment approach and management strategies, as treatment for depression and/or anxiety can differ from that for concussion alone (e.g., cognitive behavioral therapy for prolonged concussion symptoms28, 29). Neuropsychology involvement in concussion management can help differentiate cognitive symptoms postconcussion from broader symptomatology overlapping with mental health considerations. For patients whose psychological factors are more severe (i.e., new-onset post-traumatic stress following a motor vehicle collision), referral to outpatient mental health services is most likely appropriate. Explaining this association between symptomatology and noninjury factors to patients and their families can require a sensitive approach. Regardless of whether symptoms are thought to be neurological or psychological in origin, feedback should be delivered in a manner that focuses on healthy practices to reduce symptoms and improve overall functioning.
Limitations
In the context of study strengths, including a large, diverse sample in terms of ethnicity, insurance status/type, and mechanism of injury, several limitations must also be acknowledged. Though the current sample represents a strength for all the aforementioned reasons, the convenience sample derived from a specialty clinic may limit the generalizability of results to other populations. Diversity has many meanings, not all of which were well captured in this study's sample (e.g., race; predominantly White sample). Preinjury mental health history was collected as a dichotomous (yes/no) variable based on patient/family report, and further information regarding the age of onset, type, course, severity, and duration was not available. Given the consistently strong support for mental health impacts on concussion recovery in the recent literature,14 the field would benefit from a more nuanced approach that examines mental health history on a finer scale. A closer examination of the role of mental health intervention services prior to injury and during recovery on symptom reporting and recovery trajectory is also warranted. Further, data collection methods precluded evaluation of causal processes due to an inability to establish temporal precedence (e.g., retrospective report of baseline symptoms were reported in the same visit as current postconcussive symptoms).
Conclusion
Concussion recovery represents a complex biopsychosocial system with cascading effects of preinjury history on symptom experience and recovery course. This study provides additional support for the notion that heterogenous experience following injury is a function of preinjury factors and extends the generalizability of risk factors to a diverse sample of youth in terms of ethnicity, insurance status/type, and mechanism of injury. The influence of preinjury factors should be considered collectively rather than independently. Anxiety and depression represent important noninjury factors that warrant considerable attention during concussion treatment and management among pediatric populations. A preinjury history of anxiety, in particular, directly contributed to higher self-reported postconcussive symptomatology at baseline and indirectly contributed to prolonged time to clearance. Concussion providers are encouraged to incorporate psychoeducation about active rehabilitation principles and facilitate connections to additional mental health services when warranted.
Author Contributions
Laura Winstone-Weide: Conceptualization (lead), formal analysis (lead), methodology (lead), investigation (supporting), visualization (lead), writing—original draft presentation (lead), writing—review and editing (equal). Kelly Gettig: Data curation (equal), investigation (lead), writing—review and editing (equal). Cynthia Austin: Conceptualization (supporting), data curation (equal), investigation (supporting), visualization (supporting), methodology (supporting), writing—review and editing (equal).
Acknowledgments
The authors thank the clinical, nursing, and administration staff of the TBI/Concussion Clinic for their assistance with clinic operations, patient care, data collection, and data management. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- * Concussion, as defined by the American Congress of Rehabilitation Medicine (2023) and used throughout this article, refers to a mild traumatic brain injury with normal neuroimaging or in situations when neuroimaging was not clinically indicated.