Treatment-triggered onset and diagnosis of Sheehan syndrome in a multiple myeloma patient
Abstract
Background
Sheehan syndrome refers to a series of clinical symptoms resulting from avascular necrosis of anterior pituitary due to various reasons.
Case
We report a case of multiple myeloma patient after one cycle of chemotherapy consisting of bortezomib and dexamethasone diagnosis of Sheehan syndrome with obstinate diarrhea, low blood glucose, and coma symptom, especially, the fluorodeoxyglucose positron emission tomography (FDG-PET) and brain magnetic resonance imaging (MRI) revealed that the manifestations in the saddle area were in accordance with empty sella syndrome. A single administration with lenalidomide was given for both consolidative and maintenance treatment, and satisfactory efficacy was achieved. With the patient now remaining in satisfactory medical condition, the success of this therapy has been shown.
Conclusions
This is the first report showing a patient with combined multiple myeloma and rarely seen Sheehan syndrome, in which lenalidomide was given for treatment, and satisfactory efficacy was achieved.
List of abbreviations
-
- ISS
-
- International Staging System
-
- MRI
-
- Magnetic Resonance Imaging
-
- PET-CT
-
- Positron Emission Tomography Computer Tomography
1 INTRODUCTION
Sheehan syndrome (SS), which was first reported by Glinsini et al, refers to a series of clinical symptoms resulting from avascular necrosis of anterior pituitary due to various reasons, including from severe postpartum hemorrhage leading to anterior pituitary hypofunction.1 SS is an important cause of hypopituitarism, is common in developing countries. The most common presentation is the absence of lactation and amenorrhea, especially, after childbirth or after loss of large amounts of blood. A major outcome is insufficient production of anterior pituitary hormones. Generally, only when over one-half of the anterior pituitary is damaged, clinical syndromes will present. The genital gland is the first to be involved, followed by the thyroid gland, and adrenal cortex.2 With hypofunction of anterior pituitary, various stresses occur, including infection, diarrhea, dehydration, hunger, cold, acute myocardial infarction, which could lead to surgery for cerebrovascular accident, trauma, anesthesia, and the administration of sedatives, subsequently inducing a pituitary crisis.3 Pituitary crisis can be classified, according to its inducement and clinical manifestations, into high-fever type, low-temperature type, hypoglycemia type, water-intoxication type, and mixed type.4 Secondary empty sella syndrome can be indicated by image presentation. Magnetic resonance imaging (MRI) is significantly useful in the diagnosis of empty sella syndrome, in which increased size of sella, sunk bottom, and long-T1 and long-T2, indicating fullness of cerebrospinal fluid within the sella, are shown. The sella is linked with suprasellarcistern and subarachnoid cavity, and the pituitarium is compressed, with a height of less than 3 mm, which is closely connected with the sella bottom. The stalk hypophysial is extended to the sella bottom and located in the center or slightly backward. The optic nerve can be elevated, and the distance between pituitarium and optic nerve is extended.5 Neither plain nor enhanced MRI scanning can indicate an abnormal signal in the pituitarium. In this case study, we report a patient with multiple myeloma (MM) associated with SS.
2 CASE REPORT
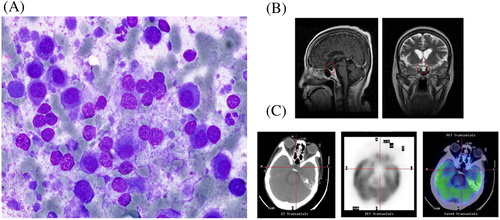
A 67-year-old woman, who had been experiencing intermittent left back pain for more than 2 years, was referred to Department of Hematology, Tianjin Medical University Cancer Institute and Hospital, Tianjin, China in October 2012. She presented with normal complete blood cell counts, normal liver and kidney function, normal blood glucose level, and normal electrolytes except for slightly decreased serum sodium level. The quantitative assessment of urine light chain for 24 hours was 3.2 g. A bone marrow aspiration showed approximate 10% immature plasma cells (Figure 1A). Positron Emission Tomography Computer Tomography (PET-CT) revealed osteolytic lesions on the eighth rib of the left side, with multiple low-density nodules found in many bones. The patient was thus diagnosed with MM, lambda-light chain type, classified by International Staging System as stage A.6 The patient was treated with one cycle of chemotherapy consisting of bortezomib (1.3 mg/m2 d1,4,8,11) and dexamethasone(40 mg d1-2,4-5,8-9,11-12). A therapeutic evaluation, including 24-hour light-chain urine monitoring and bone marrow biopsy, showed that the patient had a partial response (24-hour light-chain urine decrease more than 50%).
In December 2012, the patient presented with diarrhea, which had been occurring three to five times per day with watery stools. Supportive symptomatic therapy failed to resolve these symptoms. One day later, the patient suddenly went into a coma with no response to voice command. The medical examination revealed positive Babinski sign on the left side. A rapid blood glucose analysis was performed, which showed levels at 0.96 mmol/L (the normal range: 3.3-6.1 mmol/L).7 Intravenous injection with 50% glucose was immediately given, together with intravenous drip with hypertonic glucose and succinate hydrocortisone 100 mg. Rapid brain MRI indicated no obvious cerebral hemorrhage or infarction. After emergency treatment for 24 hours, the patient regained consciousness without sequela. However, obstinate diarrhea still presented, occurring six to eight times a day, but improved after live combined bifidobacterium (6 g/d) and lactobacillus tablets (3 g/d) and loperamide were administered orally.
Medical history showed that the patient had experienced childbirth twice, with severe postpartum hemorrhage after her second one in 1969. This subsequently led to gradual pubic and axillary trichomadesis, hypothyroidism, and sinus bradycardia, for which no special treatment was given, and no definitive diagnosis was rendered. SS is characterized by severe bleeding during childbirth due to certain complications. Hematogenous circulatory failure causes anterior pituitary blood transport disorder, thrombosis, and anterior lobe tissue. Ischemic necrosis, followed by fibrosis, leads to insufficient secretion of prohypophysial hormones, clinical syndrome of low gland, thyroid, and adrenal function. After recovery from coma, the work-up for the current case included an evening adrenocortical function test, which showed that adrenotrophic hormone was 5.90 pg/mL (0-46 pg/mL), corticosteroid was 2.10 μg/dL (5-25 μg/dL), and 24-hour urinary cortisol was 27.2 μg/24 h (30-110 μg/24 h), and no abnormality of adrenocortical function.8 A PET-CT and brain MRI revealed that the manifestations in the saddle area were in accordance with empty sella syndrome (Figure 1B and 1C). It was determined that, based on hypofunction of the anterior pituitary, the administration of large doses of steroids and obstinate diarrhea had induced a pituitary crisis, which presented as hypoglycemic coma and hyponatremia. The patient was diagnosed through retrospective analysis with SS and hypoglycemia type of pituitary crisis. Oral hydrocortisone (20 mg in the morning and 10 mg in the evening, with an interval of 12 hours) was administered as an alternative therapy. Since then, adrenocortical function of this patient remained normal, as indicated in several follow-up examinations. The patient signed the informed consent and agreed to publish it, which has been approved by the ethics committee of Tianjin Medical University Cancer Institute and Hospital.
3 DISCUSSION
Use of large doses of steroids is a first-line therapy in the treatment of MM. Therapy with bortezomib and had satisfactory efficacy in the induction treatment of this patient. On the basis of hypofunction of anterior pituitary, however, the administration of this therapy increased the risk of pituitary crisis. Therefore, instead, three cycles of lenalidomide (25 mg d1-28/cycle) alone were administered, which resulted in a complete response, as assessed by bone marrow aspiration and urine light-chain examination. Thereafter, lenalidomide alone was continued as maintenance treatment. The patient continued showing a complete response. Currently, she presents with good general condition and lives a normal life.
The patient in this study had a clear history of postpartum hemorrhage and had previously presented with pubic and axillary trichomadesis. In our patient, a medical examination revealed light areola papillaris and abnormal adrenocortical function, with manifestations in brain MRI and PET-CT in accordance with empty sella syndrome (Figure 1B and 1C). Thus, with a definitive diagnosis of SS, this patient could be treated with steroids as alternative therapy. Hydrocortisone is the first choice, but dexamethasone should be not administered for such patient due to its strong inhibition to hypothalamic-pituitary-target gland axis. SS was frequently seen in China in the 1950s and 1960s, but it is presently rarely seen because of economic progress and improved peripartum health care through the past decades. The treatment of patients with combined SS and MM is still challenging.9 Bortezomib plus dexamethasone therapy, with large doses of dexamethasone, was initially effective for our patient, but it increased the risk of pituitary crisis. Thus, lenalidomide, an immunomodulatory agent,10 was selected as consolidative treatment for this patient. After a complete response was achieved, single administration with lenalidomide was given for maintenance treatment. With the patient now remaining in satisfactory medical condition, the success of this therapy has been shown.
4 CONCLUSION
In conclusion, this is the first report showing a patient with combined MM and rarely seen SS, in which single administration with lenalidomide was given for both consolidative and maintenance treatment, and satisfactory efficacy was achieved.
AVAILABILITY OF DATA AND MATERIAL
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
ACKNOWLEDGEMENTS
This work was supported by grants from the National Natural Science Foundation of China (81600163).
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.
AUTHORS' CONTRIBUTION
All authors had full access to the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Conceptualization, B.X.; Investigation, B.X.; Formal analysis, B.X.; Resources, B.X.; Writing—original draft, B.X. and PF.L.; Writing—review and editing, B.X.; Visualization, B.X.; Supervision, B.X.; Funding acquisition, B.X.
FUNDING
This work was supported by grant from National Natural Science Foundation of China (81600163).