The pathological differential diagnosis of portal hypertension
Potential conflict of interest: Nothing to report.
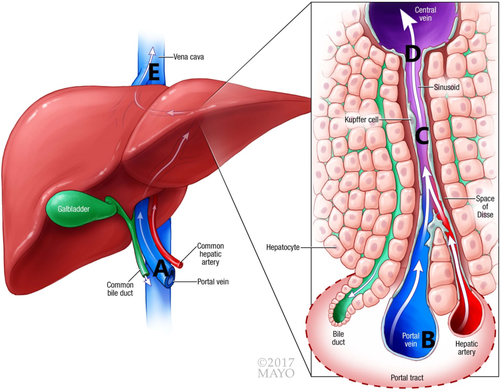
The most common cause of portal hypertension is cirrhosis of the liver. Increasingly, however, liver biopsies are being done for unexplained portal hypertension. This condition is often clinically referred to as idiopathic noncirrhotic portal hypertension.1 The physiology of portal hypertension can be explained in a simplistic manner in that there is obstruction or impairment of blood flow through the portal vein. This results in increased pressure in the portal vein. When this occurs chronically, serious consequences can ensue, including the formation of esophageal varices with subsequent hemorrhage that may lead to significant morbidity and mortality. Portal hypertension is frequently determined using pressure measurements in the hepatic vein and the sinusoidal wedge pressure, which often mimics the portal pressure.2 The difference between the two is referred to as pressure gradient. The existence of a gradient, as well as the actual pressure measurement, can help in determining the level of obstruction. This is shown in Table 1.
| Location of Lesion in Fig. 1 | Level of Obstruction | Condition | Elevated Hepatic Vein Pressure/Gradient Present |
|---|---|---|---|
| A | Prehepatic |
Portal vein thrombosis Congenital venous abnormalities |
No/No |
| B | Hepatic (presinusoidal) |
Hepatoportal sclerosis Schistosomiasis Granulomatous disease |
No/No |
| C | Hepatic (sinusoidal) |
Cirrhosis Congenital hepatic fibrosis Steatohepatitis Nodular regenerative hyperplasia Amyloidosis |
No/Yes |
| D | Hepatic (postsinusoidal) | Veno-occlusive disease (sinusoidal obstructive syndrome) | No/Yes |
| E | Posthepatic |
Budd-Chiari syndrome Cardiac failure |
NA Yes/No |
- The level of obstruction, the specific condition, whether the hepatic venous pressure measurement is elevated, and whether a pressure gradient exists are listed.
The causes of portal hypertension can be categorized as prehepatic, hepatic, and posthepatic. This is entirely based on the level of obstruction of the portal circulation (Table 1). The hepatic causes can also be subcategorized as presinusoidal, sinusoidal, and postsinusoidal (Fig. 1).
Prehepatic Causes
Portal Vein Thrombosis
The most common condition leading to portal hypertension is portal vein thrombosis. This can occur because of a variety of conditions. Portal vein thrombosis is seen frequently (up to 50%) in cirrhotic native livers examined at transplantation. Portal vein thrombosis may also be seen in patients with inherited or acquired prothrombotic states. In about 25% of patients, the reason for thrombosis is not identified. Thrombosis in cirrhotic patients is likely due to abnormal hemodynamics with slowing of the portal vein flow. Inherited conditions associated with thrombosis include factor V Leiden, antithrombin, protein C, and protein S deficiencies and increased factor VII levels. The pathology of portal vein thrombosis usually manifests itself as deposition of fibrin with entrapment of red cells. With time, organization occurs with vascularization of the blood clot and deposition of collagen.
Congenital Venous Abnormalities
Congenital venous abnormalities of the portal vein system may also lead to portal hypertension. These abnormalities include partial or complete agenesis of the portal vein, abnormal branching of the portal vein, venous malposition, arteriovenous malformations, and the persistence of fetal valves.
Presinusoidal Causes
Hepatoportal Sclerosis
Hepatoportal sclerosis is a condition with multiple names. The essence of the lesion is that intrahepatic veins become sclerotic with fibrous obliteration of the lumen (Fig. 2). As shunting occurs, additional findings may include abnormally dilated portal venous branches with extension into the hepatic lobules. The cause of this lesion is not known. Multiple causes have been implicated in its development, most commonly toxicity caused by exogenous elements.
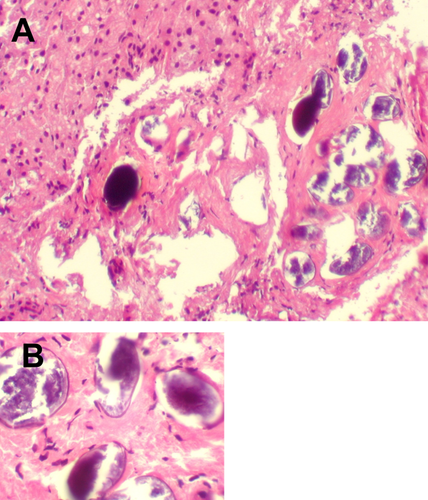
Schistosomiasis
Schistosomiasis is a well-documented cause of portal hypertension. The Schistosoma eggs embed in the portal veins and lead to obstruction of the portal vein system (Fig. 3).
Granulomatous Inflammation
Multiple etiologies result in granulomatous inflammation. Most will not result in portal hypertension. When granulomatous inflammation occurs primarily in the portal tracts and widely involves the liver, then portal hypertension may occur. Granulomas occur when there is a coalescence of histiocytes, often forming giant cells. Granulomas may be necrotizing or nonnecrotizing. Necrotizing granulomas typically occur with infectious causes. Other notable granulomatous conditions include sarcoidosis and primary biliary cholangitis (Fig. 4).

Sinusoidal Causes
Common to the sinusoidal causes is the disruption of the functional sinusoidal microanatomy resulting in impaired blood flow. The disruption may occur within the sinusoidal lumen or in the space of Disse.
Cirrhosis
As stated earlier, cirrhosis is often associated with portal vein thrombosis, contributing to the portal hypertension. However, even in the absence of portal vein thrombosis, cirrhotic livers invariably cause portal hypertension as a result of altered microanatomy, resulting in significant disruption and alteration of blood flow through the liver.
Congenital Hepatic Fibrosis
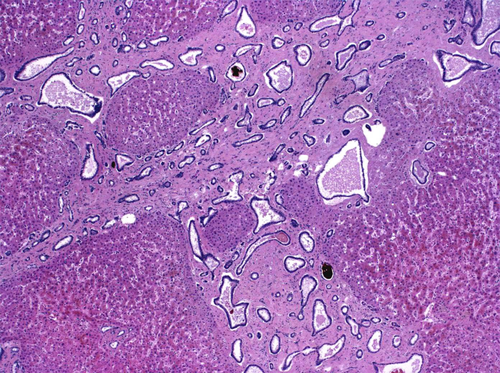
Congenital hepatic fibrosis is one of a group of fibrocystic diseases of the liver that result from abnormal development of the ductal system during intrauterine development. The full-blown syndrome shows broad fibrous septae with numerous cystic abnormal ductal structures (Fig. 5). Von Meyenburg complexes are commonly seen in congenital hepatic fibrosis.
Steatohepatitis
Advanced stage steatohepatitis can result in portal hypertension because the disease results in deposition of collagen within the perisinusoidal space, resulting in impaired blood flow through the sinusoids. The classic features of steatohepatitis include fatty change, ballooning degeneration with the formation of Mallory's hyaline, and acute inflammatory cells.
Amyloidosis
Multiple forms of amyloidosis can occur. When amyloid deposition is limited to the periarterial location, it is unlikely to cause portal hypertension. When amyloid deposits within the sinusoids, it will result in portal hypertension. This could also occur if masses develop in the liver. The pathophysiology is that of obstruction and altered blood flow. Amyloidosis deposits as material that does not stain well with the usual hematoxylin and eosin stains (Fig. 6). Congo red stain shows amyloid as an orange color that polarizes well and produces apple-green birefringence.

Nodular Regenerative Hyperplasia
Nodular regenerative hyperplasia is a condition that is often seen in patients with collagen vascular diseases. It is thought to be due to chronic use of steroids or other anti-inflammatory treatments. Other drugs have also been implicated. The condition results in a diffusely nodular liver that does not exhibit fibrosis. Morphologically, regenerative nodules of hepatocytes are present surrounded by collapsed or atrophied hepatic plates. This is best highlighted with a reticulin stain (Fig. 7).
Sinusoidal Tumor Infiltrates
There have been rare reported cases of tumor infiltrating through the sinusoids to the degree of causing portal hypertension. Examples of such occurrences include leukemia and lymphomas involving the liver.
Postsinusoidal Causes
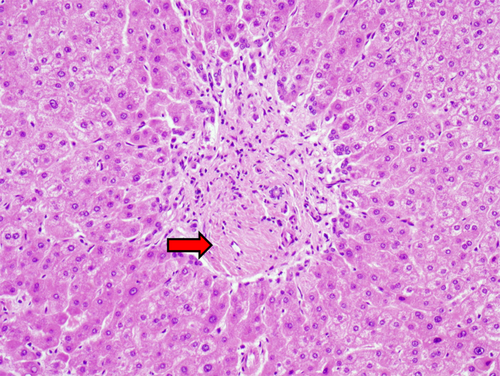
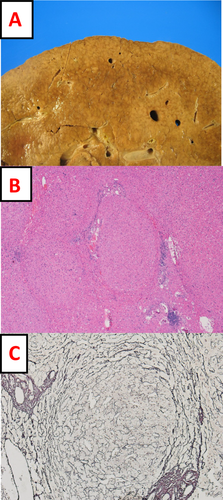
Sinusoidal Obstructive Syndrome (Veno-occlusive Disease)
Sinusoidal obstructive syndrome typically occurs in patients with hematological malignancies after stem cell or bone marrow transplantation. It is thought to develop from prolonged conditioning chemotherapeutic agents. The lesion is an injury of the zone 3 sinusoidal lining cells at the point where the sinusoids communicate with central veins. This results in collapse of the walls of the central vein narrowing the lumen, leading to obstruction of blood flow through the sinusoids and the central veins. Over time, this lesion scars (Fig. 8).
Post-Hepatic Causes
Budd-Chiari Syndrome
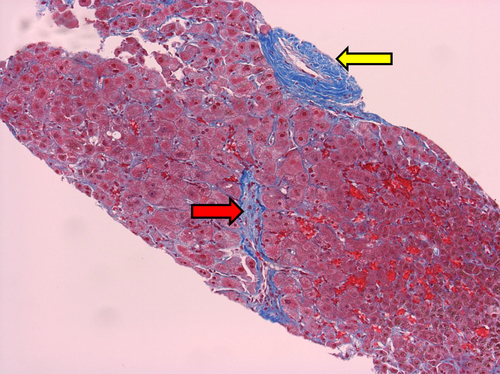
Budd-Chiari syndrome occurs when the hepatic vein becomes thrombosed. When this occurs acutely, there is marked dilatation and congestion of the central veins and sinusoids often with centrilobular hemorrhage. Depending on the case and extent of the lesion, thrombi may be seen in the central veins with necrosis or atrophy of the pericentral hepatocytes. Depending on the extent of injury, long-term findings will vary. They may include scarring, necrosis, and regeneration.
Cardiac Failure
Cardiac failure may occur because of any number of conditions. The differential diagnosis of cardiac failure in the setting of portal hypertension is routinely considered during cardiac transplantation workup and occasionally during renal transplant workup. Although the cardiac failure is known at the time of workup, the question posed to the pathologist is whether the portal hypertension is due to the cardiac condition or other hepatic causes. The hepatic pathology of cardiac failure manifests as marked sinusoidal dilatation and congestion. Over time, central venular fibrosis and sinusoidal fibrosis may develop.