Developing a liver cancer program in the nonacademic medical center
This study was supported by a grant from the Maybelle Clark Macdonald Fund (to P. H. Newell) for hepatitis B screening and education. Funding for a screening and tracking program for at-risk patients was provided by a grant from the Providence Foundation (to K.F.).
Potential conflict of interest: Nothing to report.
Abbreviations
-
- AASLD
-
- American Association for the Study of Liver Diseases
-
- BCLC
-
- Barcelona Clinic Liver Cancer
-
- CT
-
- computed tomography
-
- EMR
-
- electronic medical record
-
- ER
-
- emergency room
-
- GI
-
- gastrointestinal
-
- HCC
-
- hepatocellular carcinoma
-
- HCV
-
- hepatitis C virus
-
- LIRADS
-
- Liver Imaging Reporting and Data System
-
- MRI
-
- magnetic resonance imaging
-
- PCP
-
- primary care provider
-
- US
-
- ultrasound
Hepatocellular carcinoma (HCC) is among the major causes of cancer-related death worldwide and is the fastest growing cause of solid-organ cancers in the United States, having increased 72% between 2003 and 2012, with most cases related to hepatitis C virus (HCV).1 Although robust evidence to support surveillance for HCC in the at-risk population is lacking, recent meta-analyses and international guidelines support such a policy.2, 3 Identification of early HCC by surveillance of patients with chronic liver disease allows application of curative treatments.
The key to developing an effective community-based liver cancer program is effective collaboration among primary care physicians, gastroenterologists and hepatologists, surgeons, diagnostic and interventional radiologists, oncologists, and transplant programs through the continuum of cancer care management. Clinicians involved in care of patients with chronic liver disease are well versed at collaborating closely with colleagues from multiple disciplines in complex patient care; this serves them well in developing community programs to manage HCC.
The rationale and motivation for establishing a community HCC screening program is 3-fold: (1) randomized trials and meta-analyses demonstrate HCC screening yields diagnosis at earlier tumor stages and results in an increased proportion of curative treatments and improved survival4; (2) guidelines established by AASLD and international organizations recommend screening at-risk populations; and (3) unfortunately, there is potential for litigation against local health care systems that fail to screen for HCC according to guidelines. To motivate commitment of resources from local grant funding agencies and community cancer centers to our community HCC program, we obtain regional and state public health data to frame the challenge of HCC at the local level. For example, reported cases of HCC in Oregon have grown 4-fold over the last 15 years and are predominantly attributable to HCV in recent years (Fig. 1).5 HCC accounts for about a third of yearly HCV-related deaths in the state, which occurs at about twice the national average.
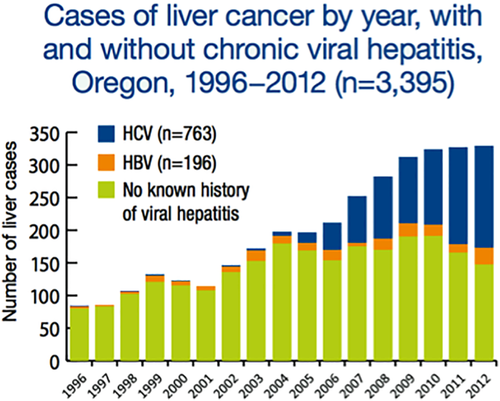
HCC cases reported to the Oregon Health Authority: 1996 to 2012. Reproduced with permission from Oregon Health Authority.5
In our community to date, gastrointestinal (GI) and hepatology specialists have largely adopted the responsibility for screening for HCC, with ongoing efforts to further engage primary care providers (PCPs). We screen our patients every 6 months with ultrasound according to American Association for the Study of Liver Diseases (AASLD) guidelines. Our practice has made an effort to standardize the ultrasound technique by purchasing high-quality equipment and designating dedicated ultrasonography technicians who perform HCC screening in our office. We have obtained funding from local grant agencies, pharmaceutical companies, and the community cancer center to support the development of educational materials and to sponsor educational conferences for local physicians and patients concerning the appropriate target population and the benefits of HCC screening. To improve and track compliance for physicians, we have made efforts to add prompts and “dashboards” in the electronic medical record (EMR) within our practice and in the hospital system used by a large number of local primary care physicians.
The success of an automated system that reminds patients about ultrasound appointments, transmits results to patients and physicians, and maintains the recall database depends on a substantial commitment of resources and personnel. Integration of this process with the EMR is an ongoing challenge but is imperative. This can be particularly problematic when the patient population is fragmented over several health care and EMR systems. We regularly update a database of at-risk patients; patients are removed once HCC is detected, or upon transplantation, progression to nonreversible hepatic decompensation or prohibitive comorbidities, or death. Since instituting a screening program over the last 5 years, patients diagnosed by screening have increased 3-fold at our tumor board (Fig. 2A), mainly as a result of screening ultrasound ordered by GI/hepatology specialists (Fig. 2B).
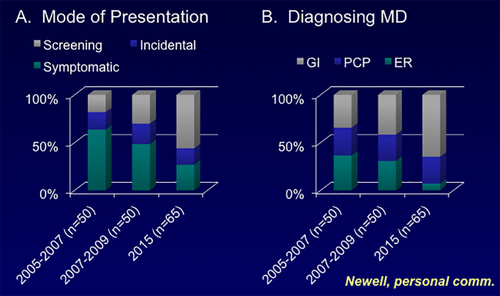
Impact of screening on HCC diagnosis on mode of presentation and specialty of diagnosing provider. Abbreviation: ER, emergency room.
When screening results are positive, our diagnostic imaging colleagues generally make the diagnosis of HCC during a multidisciplinary liver tumor board held weekly at the community cancer center.6 The tumor board is well attended by GI/hepatology specialists, hepatobiliary surgeons, interventional radiologists, medical and radiation oncologists, oncology nurse navigators, and trainees (Fig. 3). All participants, including regional providers accessing the conference via remote conferencing links, bring results of hepatoma screening and other liver tumor cases to this working conference. The group discusses diagnostic and treatment strategies for patients upon initial diagnosis, and reviews progress of patients undergoing treatment. Each week, about one-third of cases are new and two-thirds are review cases. Imaging is pushed to a central server from several regional hospitals, and the history and laboratory data are generally available in the EMR. Our diagnostic radiology colleagues use the Liver Imaging Reporting and Data System (LIRADS) criteria for diagnosis of HCC.7 A close working relationship is maintained with our regional liver transplant program. The conference serves as an efficient patient management tool while facilitating review of imaging for quality assessment and diagnostic consensus; provides efficient collective input on the appropriate next steps in diagnostics and treatment; generates continuing medical education credits; and functions as a teaching opportunity for medical and surgical trainees, nurse practitioners, and physician assistants.
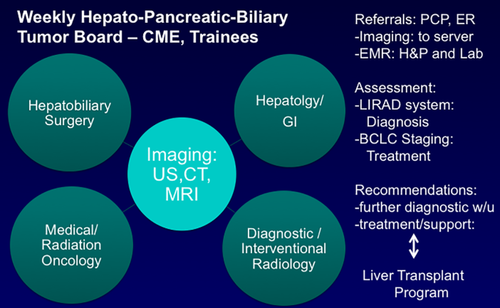
Community-based multidisciplinary liver cancer tumor board. Abbreviations: CT, computed tomography; ER, emergency room; MRI, magnetic resonance imaging; US, ultrasound.
Treatment recommendations generally follow the Barcelona Clinic Liver Cancer (BCLC) Staging and Treatment Algorithm (Fig. 4), complementing imaging data on extent of tumor with available clinical information such as hepatic reserve, medical comorbidities, transplant candidacy, functional capacity, and patient wishes.8 Interventional radiology receives the bulk of treatment referrals from the tumor board (∼60% to 70%), and many patients undergoing locoregional therapy are re-presented to the board to determine next steps. We aim to ensure that patients get established with both gastroenterology/hepatology and medical oncology departments regardless of the initial treatment plan, because patients can decompensate over the course of HCC treatment or their cancers can progress. The community cancer center invests in this process by providing an oncology nurse navigator who educates patients and facilitates communication between providers. Additionally, the cancer center is the primary access point to research protocols for patients. Finally, this multidisciplinary approach to HCC provides opportunities for community-based clinical outcomes research.9
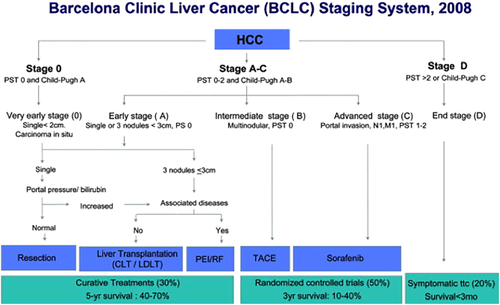
Updated BCLC staging system and treatment strategy, 2011. Reproduced with permission from Journal of Hepatology.10 Copyright 2012, European Association for the Study of the Liver. CLT, cadaveric liver transplant: LDLT, liver donor liver transplant.
The greatest potential to reduce HCC diagnosis and deaths in the community is primary prevention by identifying and treating hepatitis B and C. Expanding access to viral hepatitis care and increasing treatment capacity is necessary to substantiality impact virally induced HCC in particular. We are actively involved with patient care and legal advocates at the regional and state levels to increase access to curative direct-acting antivirals for viral hepatitis treatment.
Resource commitment to an HCC screening program results in diagnosis at earlier stages and improves survival. A collaborative multidisciplinary liver tumor conference increases efficiency of evaluation and treatment of patients with HCC (Fig. 4). A close working relationship with a liver transplant program is essential, and involvement of a community cancer center can generate valuable resources such as nurse navigators and physician collaborators.