Association between modifiable lifestyle and the prevalence of atrial fibrillation in a Chinese population: Based on the cardiovascular health score
Abstract
Background
The Cardiovascular Health (CVH) Score was comprised of a series of modifiable lifestyle and health factors, which was published by American Heart Association in 2010. Its relationship with atrial fibrillation (AF) remains unclear.
Hypothesis
Individuals with a higher CVH Score had a lower risk of AF.
Methods
Participants ≥40 years of age were recruited from the Jidong community. Information regarding the following 7 CVH metrics, including smoking, body mass index, diet, physical activity, total cholesterol, and fasting blood glucose, were collected. AF was confirmed with a standard 12-lead electrocardiography or based on the patients' medical histories. A multivariable logistic regression model was used to evaluate the relationship between ideal CVH and AF prevalence.
Results
This study included 4477 individuals, among whom 48 had AF (1.07%). Overall, participants with higher ideal components scores had a lower risk of AF (odds ratio [OR]: 0.78; 95% confidence intervals [CI]: 0.62-0.97; P trend = 0.024). Subgroup analyses showed that the trend was consistent in the male participants ages 40 to 60 years. Moreover, patients with 5 to 7 ideal components or 3 to 4 ideal components were associated with 57% and 59% reduced risks for AF, respectively. We also detected a significant association between ideal health factors and the prevalence of AF (OR: 0.79; 95% CI: 0.68-0.93; P = 0.004).
Conclusions
Ideal health behavior and factors are associated with lower prevalence of AF in a community-based population. Improving healthy behavior and these factors may be beneficial to decrease the prevalence of AF.
1 INTRODUCTION
Atrial fibrillation (AF) is the most common arrhythmia in the clinic, and comorbidities with AF have been associated with an increased risk of morbidity and mortality.1 AF may cause many fatal complications such as thromboembolic events and heart failure. Notably, patients with AF are associated with an approximately 5-fold increase in the risk of stroke.2 Therefore, the early identification of patients at risk for AF is of important significance for the prophylaxis of AF and related complications. Although there are many factors, such as an unhealthy diet, obesity, inactivity and smoking,3, 4 the overall associations between healthy behavior and factors are rarely reported.
The American Heart Association (AHA) recently established the concept of ideal cardiovascular health (CVH) metrics based on 4 healthy behavior metrics (nonsmoking, normal weight, moderate physical activity, and a healthy diet) and health factors (normal cholesterol, blood pressure, and fasting blood glucose [FBG]). 5 Each of these metrics could be applied to categorize the individuals into 3 levels, namely ideal, intermediate, or poor, scored with 2, 1, or 0 points, respectively.6 Therefore, the CVH metric is accordingly scored from 0 to 14 points, with 14 indicting ideal health for all 7 domains. Subsequent studies related ideal CVH scores with a lower risk of cardiovascular disease (ie, coronary artery disease and myocardial infarction) and stroke.7-9 However, the potential association between CVH scores and the risk of AF has rarely been evaluated. Therefore, we performed a cross-sectional study in a Chinese community population to explore the association between CVH metrics and AF prevalence.
2 METHODS
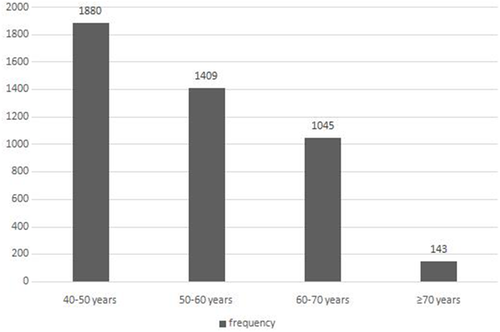
Our study employed a cross-sectional examination of baseline data collected in 2013 to 2014 from the Jidong community located in Tangshan, Hebei Province, China. This community is primarily comprised of employees of Jidong Oilfield Inc. and their families. All residents over 18 years old (9078 residents) were invited after excluding individuals who were unable or unwilling to participate. Among these participants, we further excluded participants under 40 years old (4374), as well as those with missing data regarding healthy behavior, health factors, electrocardiography (ECG) data, or potential confounders (227). Ultimately, a total of 4477 participants ages 40 to 82 years were eligible and completed the baseline screening program (Figure). At baseline, a clinical interview with a thorough physical examination was conducted by trained professional physicians from the hospital of Jidong Oilfield Inc. for each participant. The study protocol was approved by the medical ethics committee of Jidong Oilfield Inc., and this study was conducted in accordance with the Declaration of Helsinki.
2.1 Assessment of CVH metrics
Based on the published report by the AHA, the following 7 healthy behavior metrics were applied to define CVH in our study: smoking, physical activity, body mass index (BMI), healthy diet, total cholesterol, blood pressure, and FBG.5 The dietary intake, smoking, and physical activity statuses were assessed with a semiquantitative questionnaire, and the other indices were measured at the time of baseline recruitment.
2.2 Smoking
According to the AHA guidelines, we classified smoking as ideal (never or quit smoking >12 months previously), intermediate (former smoking within the previous 12 months), or poor (current smoking).
2.3 Physical activity
Based on a self-report, physical activity was classified as ideal (≥150 min/wk of moderate intensity or ≥75 min/wk of vigorous intensity), intermediate (1–149 min/wk of moderate intensity or 1–74 min/wk of vigorous intensity), or poor (none), which was defined in our previous publication.10
2.4 Body mass index
BMI (kg/m2) was calculated as the body weight (accurate to 0.1 kg) divided by the square of the height (accurate to 0.1 m). For the BMI, ideal, intermediate, and poor were defined as BMI <25 kg/m2, 25 to 29.9 kg/m2, and ≥30 kg/m2, respectively.
2.5 Diet
Dietary intake was assessed with a questionnaire on food consumption frequency.11, 12 All of the participants were asked about the frequencies and quantities of the consumption of major food items during past year, including fiber-rich whole grains, vegetables, fruits, eggs, red meat (beef, lamb, and pork), seafood, milk, soybean products, nuts, sugar/sweet drinks, and tea. Salt intake was assessed according to a self-report. The healthy components of dietary intake were defined as follows: 4.5 or more servings per day of fruits and vegetables, 3 or more servings per day of fiber-rich grains, 2 or more servings per week of fish or shellfish, salt intake below 6 g per day, and a sugary drink consumption of once per week or less. We classified dietary intake as ideal (4–5 components), intermediate (2–3 components), or poor (0–1 components) according to the AHA definition.
2.6 Blood pressure, total cholesterol, and fasting blood glucose
Blood pressure was measured using a mercury sphygmomanometer. Two readings of the systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured at a 5-min interval with the participants resting in a chair, and the averages of the readings were used for the analyses. We classified blood pressure as ideal (SBP <120 mmHg and DBP <80 mmHg and untreated), intermediate (SBP 120–139 mmHg or DBP 80–89 mmHg or treated to goal), or poor (SBP >140 mmHg or DBP ≥90 mmHg). FBG was classified as ideal (<100 mg/dL and untreated), intermediate (100–125 mg/dL or treated to goal), or poor (≥126 mg/dL). Total cholesterol status was defined as ideal (<200 mg/dL and untreated), intermediate (200–239 mg/dL or treated to goal), or poor (≥240 mg/dL). All of these classifications were according to the AHA definition.
2.7 Clinical assessment
The participants underwent a physician-administrator clinical interview, a medical history collection, and a physical examination by a well-trained physician at our medical center. AF was diagnosed by a standard 12-lead ECG or a Holter report. Participants who did not exhibit AF on the ECG test but had a history of AF/atrial flutter based on all available medical records were also diagnosed with AF. The participants who were deemed to have experienced paroxysmal/persistent AF or an atrial flutter were verified upon review by another cardiology physician who was informed of all of the baseline recruitments. Diagnosis of heart failure, stroke, and myocardial infarction were determined by cardiology physicians according to the established major and minor criteria13-15 or determined by a self-report history. Alcohol consumption was defined as the consumption of 2 standard units (1 standard unit: 120 mL of wine, 360 mL of beer, 45 mL of spirits/day) or more. To evaluate the overall influence of the CVH metrics, we created a dichotomized variable for each component of the CVH metrics. “Ideal” was coded as 1, and “nonideal” (the “intermediate” and “poor” categories combined) was coded as 0.
2.8 Statistical analyses
Descriptive analyses were used to summarize the baseline characteristics of the participants based on the presence of AF. Continuous variables were described by the mean (standard deviation) and were compared using analysis of variance. Categorical variables were described with percentages and were compared using χ2 tests. Logistic regression was used to evaluate the relationships between the prevalence of AF and each of the components of the CVH metrics using odds ratio (OR) and 95% confidence interval (CI); ideal behavior and health factors were also separately evaluated. The model was adjusted for age, sex, alcohol consumption, previous heart failure, myocardial infarction, and stroke because these factors are known or possible risk factors for AF. We estimated the associations between the CVH metrics and AF stratified by sex and age, as well as the total number of ideal behavior/health factors combined. All statistical tests were 2-sided with a significance level of P ≤ 0.05. All analyses were performed using SAS 9.3 (SAS Institute, Cary, NC).
3 RESULTS
We identified 55 cases of AF (0.61%) among 9078 participants (4768 men and 4310 women). After excluding the participants with missing data and those under the age of 40 years, 48 cases of AF (1.07%) were identified in the final sample of 4477 individuals (2216 men and 2259 women); the prevalence in men and women were 1.4% and 0.71%, respectively. We reported age-stratified prevalence of AF (Table 1), and found that the prevalence of AF in the elder is significantly higher in both sexes. Table 2 provides the baseline characteristics of the individuals with and without AF. Men accounted for a larger proportion (66.7%) of the AF group than women (P < 0.05). The participants with AF were older and tended to have previous myocardial infarction, stroke, and heart failure. Regarding CVH metrics, the participants with AF had significantly lower FBG levels. No differences in the other ideal CVH metrics were found between participants with and without AF.
| Men | P Value | Women | P Value | |||
|---|---|---|---|---|---|---|
| Age 40–59 Years | Age ≥ 60 Years | Age 40–59 Years | Age ≥ 60 Years | |||
| AF | 12 (0.76%) | 20 (3.10%) | <0.0001 | 9 (0.52%) | 7 (1.29%) | 0.0629 |
| Non-AF | 1558 (99.24%) | 626 (96.9%) | 1710 (99.48%) | 535 (98.71%) | ||
- Abbreviations: AF, atrial fibrillation.
| Characteristic | AF Group | Non-AF Group | P Value |
|---|---|---|---|
| No. | 48 | 4429 | |
| Age, y | 58.5 ± 9.4 | 52.9 ± 8.7 | <0.001 |
| Gender, male, no. (%) | 32 (66.7) | 2184 (49.3) | |
| Alcohol consumption, no. (%) | 17 (35.4) | 1313 (29.6) | 0.384 |
| Myocardial infarction, no. (%) | 3 (6.3) | 37 (0.8) | 0.009 |
| Stroke, no. (%) | 4 (8.3) | 111 (2.5) | 0.034 |
| Heart failure, no. (%) | 1 (2.1) | 5 (0.1) | 0.063 |
| Blood pressure, no. (%) | 0.357 | ||
| Nonideal | 39 (81.3) | 3344 (75.5) | |
| Ideal | 9 (18.8) | 1085 (24.5) | |
| Fasting blood glucose, no. (%) | 0.007 | ||
| Nonideal | 23 (47.9) | 1328 (30.0) | |
| Ideal | 25 (52.1) | 3101 (70.0) | |
| Diet, no. (%) | 0.182 | ||
| Nonideal | 39 (81.3) | 3216 (72.6) | |
| Ideal | 9 (18.8) | 1213 (27.4) | |
| Physical activity, no. (%) | 0.168 | ||
| Nonideal | 23 (47.9) | 1692 (38.2) | |
| Ideal | 25 (52.1) | 2737 (61.8) | |
| Smoking, no. (%) | 0.236 | ||
| Nonideal | 16 (33.3) | 1143 (25.8) | |
| Ideal | 32 (66.7) | 3286 (74.2) | |
| BMI, no. (%) | 0.067 | ||
| Nonideal | 29 (60.4) | 2088 (47.1) | |
| Ideal | 19 (39.6) | 2341 (52.9) | |
| Total cholesterol, no. (%) | 0.279 | ||
| Nonideal | 17 (35.4) | 1255 (28.3) | |
| Ideal | 31 (64.6) | 3174 (71.7) |
- Abbreviations: AF, atrial fibrillation; BMI, body mass index.
- Sample size: N = 4477. Data are presented as mean ± standard deviation or number (n). Differences between the groups were tested by the unpaired t test (for continuous variables) and the χ2 or the Fisher exact test (for categorical variables) when appropriate.
We subsequently evaluated the association between each CVH metric and the prevalence of AF. After adjusting for age, sex, alcohol consumption, previous heart failure, stroke, myocardial infarction, and the other 6 CVH metrics, participants of ideal physical activity were found to have lower AF prevalence in the common population. The participants who exhibited more physical activity (≥150 min/wk of moderate intensity or ≥75 min/wk of vigorous intensity) had significantly decreased odds of AF compared with the inactive individuals (OR: 0.55; 95% CI: 0.31-0.99). The stratified analysis indicated that the inverse association between ideal diet (OR: 0.22; 95% CI: 0.05-0.92) and ideal FBG (OR: 0.35; 95% CI: 0.15-0.84) and AF prevalence was significant in the male and the 40- to 60-year-old age groups, respectively. No significant relationships were found in the other ideal CVH metrics among the subgroups (Table 3).
| Metrics | Total | Gender | Age, y | ||
|---|---|---|---|---|---|
| Male | Female | 40–59 | ≥60 | ||
| Case/participants | 48/4477 | 32/2216 | 16/2261 | 21/3289 | 27/1188 |
| Ideal smoking | |||||
| OR (95% CI) | 0.87 (0.42-1.78) | 0.93 (0.47-1.85) | 0.29 (0.05-1.58) | 0.47 (0.16-1.36) | 1.11 (0.46-2.67) |
| P value | 0.70 | 0.83 | 0.15 | 0.16 | 0.82 |
| Ideal BMI | |||||
| OR (95% CI) | 0.78 (0.42-1.46) | 0.72 (0.35-1.49) | 1.00 (0.38-2.6) | 0.70 (0.30-1.63) | 0.87 (0.41-1.86) |
| P value | 0.44 | 0.38 | 0.99 | 0.41 | 0.72 |
| Ideal physical activity | |||||
| OR (95% CI) | 0.55 (0.31-0.99) | 0.68 (0.35-1.34) | 0.38 (0.15-0.93) | 0.79 (0.37-1.72) | 0.45 (0.22-0.93) |
| P value | 0.046 | 0.27 | 0.03 | 0.56 | 0.03 |
| Ideal diet | |||||
| OR (95% CI) | 0.70 (0.33-1.46) | 0.27 (0.08-0.90) | 2.11 (0.87-5.1) | 0.97 (0.40-2.35) | 0.60 (0.23-1.54) |
| P value | 0.34 | 0.03 | 0.10 | 0.94 | 0.29 |
| Ideal blood pressure | |||||
| OR (95% CI) | 1.30 (0.60-2.84) | 0.81 (0.27-2.4) | 2.13 (0.79-5.75) | 2.06 (0.84-5.06) | 0.72 (0.21-2.54) |
| P value | 0.51 | 0.70 | 0.13 | 0.11 | 0.61 |
| Ideal total cholesterol | |||||
| OR (95% CI) | 0.88 (0.47-1.63) | 0.60 (0.31-1.19) | 1.85 (0.65-5.25) | 0.79 (0.35-1.80) | 0.87 (0.4-1.87) |
| P value | 0.68 | 0.15 | 0.25 | 0.58 | 0.71 |
| Ideal FBG | |||||
| OR (95% CI) | 0.66 (0.36-1.21) | 0.80 (0.41-1.56) | 0.44 (0.17-1.13) | 0.35 (0.16-0.79) | 1.01 (0.49-2.12) |
| P value | 0.18 | 0.51 | 0.09 | 0.01 | 0.97 |
- Abbreviations: AF, atrial fibrillation; BMI, body mass index; CI, confidence interval; FBG, fasting blood glucose; OR, odds ratio.
- a The reference group includes participants with a nonideal metric of cardiovascular health, and the following potential confounders were adjusted for each OR: age, sex, drinking, previous heart failure, stroke, and myocardial infarction.
After adjusting for age and sex, we observed that a greater number of ideal CVH metrics (summary score) was significantly associated with a lower prevalence of AF in the entire population (OR: 0.77; 95% CI: 0.62-0.95), men (OR: 0.67; 95% CI: 0.51-0.87), and those ages 40 to 60 years old (OR: 0.71; 95% CI: 0.53-0.96). These relationships remained significant after adjusting for the aforementioned factors plus potential confounders. The adjusted ORs for AF were 0.78 (95% CI: 0.63-0.97), 0.67 (95% CI: 0.51-0.88), and 0.72 (95% CI: 0.53-0.98) in the total group, men, and 40- to 60-year-old group, respectively. These associations between the numbers of ideal CVH metrics and AF prevalence did not reach the level of significance in females and those ≥60 years (Table 4).
| Total | Gender | Age, y | |||
|---|---|---|---|---|---|
| Male | Female | 40–59 | ≥60 | ||
| Model 1 | |||||
| P for trend | 0.016 | 0.003 | 0.939 | 0.069 | 0.061 |
| OR (95% CI) | 0.766 (0.618-0.951) | 0.663 (0.507-0.868) | 0.985 (0.668-1.452) | 0.745 (0.543-1.023) | 0.748 (0.552-1.014) |
| Model 2 | |||||
| P for trend | 0.024 | 0.003 | 0.951 | 0.0497 | 0.097 |
| OR (95% CI) | 0.777 (0.624-0.967) | 0.671 (0.515-0.873) | 1.013 (0.681-1.506) | 0.743 (0.552-1.000) | 0.769(0.564-1.049) |
- Abbreviations: AF, atrial fibrillation; CI, confidence interval; OR, odds ratio.
- Model 1: adjusted for age and sex. Model 2: adjusted for age, sex, drinking, previous heart failure, stroke, myocardial infarction.
The association between ideal CVH and the odds of AF was also separately observed according to the number of behavior and health factors (Table 5). We found that the participants who achieved 3 to 4 or 5 to 7 ideal CVH components exhibited 58% (OR: 0.42; 95% CI: 0.22-0.80) and 56% (OR: 0.44; 95% CI: 0.20-0.98) reductions in the odds of AF, respectively. After adjusting for age, sex, potential confounders for the risk of AF, and the other 3 component factors, we determined that a combination of 3 to 4 ideal behavior metrics decreased the odds of AF by 57% compared with 0 to 1 ideal behavior metric (OR: 0.43; 95% CI: 0.20-0.94). A similar relationship was detected when the number of ideal health factors was analyzed (OR: 0.79; 95% CI: 0.68-0.93, P = 0.004).
| No. of Participants | No. of Events (%) | OR (95% CI) | P Value | |
|---|---|---|---|---|
| All 7 componentsa | ||||
| 0–2 ideal components | 830 | 19 (2.29) | 1 | |
| 3–4 ideal components | 2164 | 19 (0.88) | 0.414 (0.215-0.798) | 0.009 |
| 5–7 ideal components | 1483 | 10 (0.67) | 0.436 (0.195-0.979) | 0.044 |
| P for liner trend | 0.613 (0.396-0.947) | 0.028 | ||
| Behaviorb | ||||
| 0–1 ideal components | 1157 | 20 (1.73) | 1 | |
| 2 ideal components | 1624 | 16 (0.99) | 0.532 (0.265-1.067) | 0.076 |
| 3–4 ideal components | 1696 | 12 (0.71) | 0.432 (0.199-0.936) | 0.034 |
| P for liner trend | 0.646 (0.435-0.961) | 0.031 | ||
| Factorsc | ||||
| 0-1 ideal components | 1824 | 27 (1.48) | 1 | |
| 2 ideal components | 1908 | 17 (0.89) | 0.759 (0.615-0.937) | 0.010 |
| 3 ideal components | 745 | 4 (0.54) | 0.671 (0.462-0.974) | 0.025 |
| P for liner trend | 0.793 (0.676-0.930) | 0.004 |
- Abbreviations: AF, atrial fibrillation; CI, confidence interval; OR, odds ratio.
- a Adjusted for age, sex, drinking, previous heart failure, stroke, and myocardial infarction.
- b Adjusted for age, sex, drinking, previous heart failure, stroke, and myocardial infarction, plus total cholesterol, fast blood glucose, systolic blood pressure, and diastolic blood pressure.
- c Adjusted for age, sex, drinking, previous heart failure, stroke, and myocardial infarction, plus current smoking, body mass index, ideal physical activity, and ideal diet.
4 DISCUSSION
The participants ages ≥40 years with ideal CVH component scores were associated with a lower prevalence of AF in this community population. This inverse association remained significant in men and participants <60 years. As expected, the behavior and health factors of ideal physical activity, dietary intake, and FBG played crucial roles. These results indicated that participants with lower CVH metrics scores may be at an increased risk for AF. Prospective cohort and interventional studies are needed to confirm our results.
4.1 Behavior
Other studies have also examined the relationships between AF and individual modifiable components.16, 17 A prospective study of 36 513 women with a median follow-up of 12 years found that moderate (>4 h weekly) physical activity reduces the risk of AF by 15% versus <1 h of exercise weekly. Moreover, participants with moderate-intensity physical activities exhibit a reduction in the incidence of AF by 28% compared with the no-exercise group according to the Cardiovascular Health Study.18 Moderate exercise may reduce the risk of AF by preventing dyslipidemia and diabetes.19, 20 Regarding dietary intake, 1 study suggested that the amount of fish intake decreases the risk of AF due to the consumption of fish oil, and docosahexaenoic acid may play an crucial role in this effect.21 The development of AF is moderately associated with the intake of ions, which may be influenced by dietary intake (soybean, grains, peanuts, and some specific vegetables and fruits).22 Interestingly, our study indicated that participants who keep a balanced diet are associated with a reduced prevalence of AF, which may be independent of the contributions of other cardiovascular risk factors.
A significant inverse relationship between current smoking and AF was proposed in previous studies.23 However, we did not observe an association between current smoking and AF prevalence in our cohort. Similarly, in a previous study in the Framingham cohort, current smoking was not found to be a significant determinant of AF risk,24 which may partially support our results. The relationship between smoking and AF remains controversial. Furthermore, no relationship was detected between BMI and AF prevalence, which may also be different from other studies conducted outside of China.25, 26 Interestingly, a previous study of 3922 elderly Chinese people indicated no association between obesity and AF prevalence (P > 0.05).27 Recent studies reported that the prevalence of AF varies according to race,28 which may partly explain the difference in prevalence of AF observed in studies from China and those from Western countries.
4.2 Factors
The present study also analyzed health factors and their associations with AF. Ideal blood pressure was found to not be significantly associated with AF prevalence. Although hypertension is widely acknowledged and has been confirmed to be among the leading contributors to AF prevalence in prospective studies,24, 29, 30 hypertension was not always a significant determinant of AF prevalence in cross-sectional studies.
Moreover, some antihypertensives, such as β-blockers and calcium channel blockers, may be protective against AF, and thereby attenuate the association between hypertension and AF. Ideal FBG may also be associated with the reduced risk of AF, perhaps reflecting the contribution of diabetes to AF.31 Our results indicate that ideal FBG significantly reduces the prevalence of AF but not in individuals over 60 years of age. This may be explained by the fact that employees of the oilfield accounted for a large proportion of the population in the present study, and these employees tended to be younger. Furthermore, elderly individuals may focus on their blood glucose levels to a greater extent than younger people. No association was detected between total cholesterol and the prevalence of AF, which is similar to the results of a multiethnic study,32 suggesting that serum cholesterol may be less important during the pathogenesis of AF.
We further explored the relationship between the number of ideal CVH metrics and the prevalence of AF. The results indicated that a single ideal cardiovascular element may not produce an obvious effect in preventing AF. However, the integration of these factors and behavior may show a profound effect due to the interactions between these elements. These results also showed that improving behavior and health factors are of significance for preventing AF. The epidemiological differences between men and women were reasonable due to the differences in the physiological characteristics and the ranges of behavior between the sexes.
4.3 Strengths and limitations
Although the results of this study are favorable, some limitations warrant consideration. First, we were not able to determine the temporal aspects of the relationships between the CVH metrics and AF because we did not conduct a cohort study. However, our follow-up study is ongoing, and prospective studies may be performed in the future. Second, this research was based on individual residents of a single community. Consistent with aforementioned epidemiologic data, the number of AF patients is relatively small (0.6%). Moreover, our study sample was primarily composed of the young and middle-aged miners of Jidong Oilfield Inc., and the proportion of elderly subjects is limited. However, the advantages of our study are the inclusion of a community-based, randomized, large sample of 4477 subjects; face-to-face clinical interviews; and a wide age range (40–82 years old), which in part make up for the weaknesses. Third, the baseline ECG measurements and Holter reports were performed only once; we were thus unable to identify individuals with asymptomatic AF. However, the method used in our study has also been applied in other published epidemiological investigations.32-34
5 CONCLUSION
Ideal healthy behavior and factors are associated with lower prevalence of AF in a community-based population. Improving healthy behavior and factors may be beneficial to decrease the prevalence of AF.
Acknowledgments
The authors appreciate all of the participants, their families, and the members of the survey team from the Jidong community. The authors thank the staff of Recovery Medical Technology Development Co., Ltd. for their important efforts.
Author contributions
Yiheng Yang and Xu Han contributed equally to this work. All authors had access to the data and a role in writing the article. Yiheng Yang, Xiaomeng Yin and Yunlong Xia designed this study. Yiheng Yang and Xu Han wrote the article. Jing Qiu and Yue Chen conducted the data analysis. Yong Zhou and Youxin Wang provided the database and reviewed the article. Huihua Li, Lianjun Gao, and Yunlong Xia conducted the quality assurance and reviewed and edited the article.
Conflicts of interest
The authors declare no potential conflict of interests.




