Intramyocardial Hematoma After Percutaneous Coronary Intervention for Chronic Total Occlusion: Two Case Reports
ABSTRACT
Percutaneous coronary intervention (PCI) for chronic total occlusion (CTO) is an extremely challenging procedure, with intramyocardial hematoma (IMH) being one of its rare yet severe complications. In this report, we detail two cases of IMH occurring during PCI for CTO, emphasizing the importance of avoiding catheter pressure entrapment and high - dose antegrade angiography during recanalization. Both cases were the right coronary artery (RCA) CTO. In one case, after antegrade recanalization, the patient developed pericardial tamponade secondary to IMH due to these risky factors (catheter pressure entrapment and high—dose antegrade angiography), which necessitated surgical intervention. In the other case, following the same risky factors and repeated angiography, the patient experienced hypotension due to IMH, diagnosed by transthoracic echocardiography. However, as the hematoma did not involve the pericardium, conservative management was adopted.
1 Introduction
Chronic total occlusion (CTO) is defined as complete coronary artery occlusion lasting for over 3 months, with thrombus grading according to the TIMI (Thrombolysis in Myocardial Infarction) flow classification resulting in grade 0 blood flow [1]. Approximately 18.2%−52.0% of patients with coronary artery disease have CTO of the coronary arteries [2-5]. CTO lesions present technical challenges in percutaneous coronary intervention (PCI), critical for patient outcomes [6, 7]. Consequently, the presence of a CTO increases the complexity of interventional treatment. At the same time, CTO is also associated with a higher risk of myocardial ischemia and potential mortality [8, 9]. PCI) for CTO are thus highly complex and associated with a significant risk of complications. Among these complications, coronary perforation (CP) is particularly feared. Intramyocardial hematoma (IMH) is extremely rare clinically. Here, we present two rare cases that were successfully treated with different therapeutic approaches. IMH is extremely rare clinically. We present two rare cases that were successfully treated with different therapeutic approaches.
2 Cases Report
2.1 Case One
An 86-year-old female patient with a history of unstable angina and prior PCI was admitted for further coronary intervention. Six months ago, she had stenting of the left anterior descending artery (LAD), and 3 months ago, an attempt to recanalize the CTO of the right coronary artery (RCA) failed. Recent angiography showed 70% stenosis in the proximal LAD, 70% restenosis within the previously placed the LAD stent, and complete occlusion of the mid-RCA. A 3.5 × 23 mm stent was implanted in the left main coronary artery (LMCA)-LAD under intravascular ultrasound (IVUS) guidance, and the RCA was successfully recanalized with two stents implanted in the mid-RCA. During preparation for the third stent, unrecognized catheter pressure entrapment caused a sudden drop in blood pressure and heart rate when a high—pressure syringe was used for antegrade imaging. The third stent was immediately implanted, and right coronary angiography showed no active extravasation. After symptomatic treatment, the patient was transferred to the cardiac intensive care unit. Within 1 h post-intervention, the patient developed hypotension (69/41 mmHg) and tachycardia (125 beats/min) with concurrent ST-segment elevation on electrocardiogram (ECG). Transthoracic echocardiography (TTE) confirmed moderate pericardial effusion (about 200 mL of blood fluid), and subsequent pericardial puncture extracted blood fluid. After autotransfusion of 220 mL of blood, the patient's blood pressure improved to 110/70 mmHg and heart rate decreased to 70 beats/min. Immediate coronary angiography revealed no apparent bleeding source (Video 1).
Post-operation hypotension in the patient was suspected to result from blood loss or cardiac tamponade caused by unrecognized catheter pressure entrapment. This was confirmed by the presence of moderate pericardial effusion (around 200 mL), and the patient was treated with pericardial puncture and autotransfusion. Owing to the ongoing drainage of a considerable quantity of fresh, crimson blood from the pericardium of the patient, the patient was transferred to the cardiac surgical department to undergo thoracotomy. During the urgent thoracotomy, an IMH and three small lacerations were identified in the right ventricular surface along the acute marginal branch, with additional hematoma noted in the posterior lateral branch region of the left ventricle (Video 2). Hemostasis was accomplished by patch grafting and suturing over the damaged regions. The patient showed steady recovery: extubated on Day 5, transferred from Cardiac Surgery Intensive Care Unit on Day 6, and discharged on Day 10.
2.2 Case Two
A 53-year-old male patient was admitted to our facility due to unstable angina. Six months before this admission, two stents had been successfully implanted in the left coronary artery. The primary objective of the current admission was to address CTO of the RCA. The procedure commenced with an attempt to recanalize the RCA, which was ultimately successful. However, during the subsequent phase, the operator encountered difficulty in withdrawing the extended catheter (Guiderzilla). Unaware of the pressure entrapment, repeated contrast injections were performed. This unfortunate event led to diffuse contrast extravasation from the RCA (Video 3). As a result, there was a sudden and significant decline in both blood pressure and heart rate. In response to the hemodynamic instability, vasopressors and inotropes were immediately administered. This prompt intervention effectively stabilized the patient's hemodynamic status. Left coronary angiography was then conducted, revealing TIMI 3 flow in the left coronary artery. Moreover, there were no obvious signs of rupture or dissection in the RCA. To manage the situation, two stents were rapidly implanted in the proximal and mid-segments of the RCA. Post-operative coronary angiography demonstrated no significant irregularities in the stents and no further contrast extravasation. Intra-operative fluoroscopy also showed no evidence of pericardial effusion.
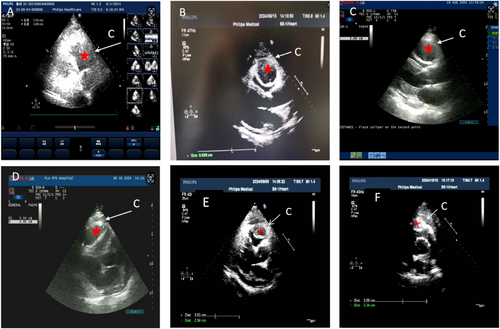
The patient's ECG post-operation indicated sinus rhythm, albeit with ST-segment changes. Post-operatively, the patient reported chest pain and exhibited signs of irritability. The blood pressure (120−140/70−80 mmHg), and the heart rate ranged (80−90 beats/min). Serial ECG monitoring did not reveal any significant dynamic changes. To alleviate the patient's discomfort, intravenous midazolam (10 mg) was administered for sedation, and subcutaneous morphine (10 mg) was given for analgesia, along with other symptomatic treatments. At 7:00 AM the following morning, the patient's blood pressure dropped to 83/57 mmHg. To maintain an adequate blood pressure, norepinephrine was administered via micro-infusion. Echocardiograms performed at 6:00 PM, 8:00 PM, and 11:00 PM detected IMH measuring 82 × 47 mm, with clear boundaries and evidence of right ventricular compression. On the second post-operative day, the patient presented with intermittent restlessness, clammy skin, and peripheral cyanosis. Physical examination revealed a heart rate of 111 beats per minute, a blood pressure of 85/68 mmHg (maintained with continuous norepinephrine infusion), and scattered moist rales in both lungs. In light of the patient's critical condition, he was transferred to the intensive care unit for a week of vasopressor support and fluid resuscitation. Once the patient's hemodynamics were stabilized, the vasopressors were gradually discontinued, and the patient was transferred to the general ward for further treatment. One week later, the patient was discharged. The discharge echocardiogram showed a right ventricular wall hematoma measuring 87 × 48 mm, with clear boundaries and right ventricular compression (Figure 1A−D). Post-operatively, at the 1-month follow-up, the patient encountered a transient episode of ventricular tachycardia. This arrhythmic event was effectively managed through conservative medical treatment. Subsequently, cardiac echocardiography was performed at both the 1- and 2-month time points after the operation to comprehensively assess the patient's cardiac structural and functional status, aiming to detect any potential post-operative changes or complications in a timely manner(Figure 1E,F). At the 3-month follow-up, the patient remained asymptomatic.
3 Discussion
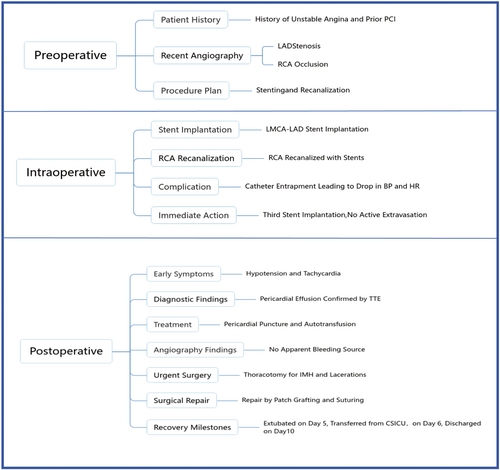
IMH following retrograde CTOPCI is extremely rare and seldom reported [10, 11]. Our first case demonstrates the severe consequence of IMH leading to pericardial tamponade, which required urgent surgical intervention. This underscores the importance of vigilant monitoring and readiness for surgical management in cases where IMH poses an immediate threat to life. The second case illustrates that conservative management can be effective when the hematoma is confined to the myocardium without pericardial involvement, provided that close surveillance is maintained to detect any progression or complications (Flow 1).
We believe that by presenting these two distinct scenarios, we provide a comprehensive view of the spectrum of IMH management. This case report serves as a reminder to all interventional operators to be cautious of the potential for IMH, especially during high-risk procedures like CTO interventions, and to be prepared for both conservative and surgical management strategies as indicated. Our report is unique as IMH, a rare and life—threatening condition, developed after CTO surgery. Fortunately, early diagnosis and appropriate treatment led to the patient's successful recovery.
Myocardial contrast echocardiography (MCE) [12] and TTEassessment of the hematoma is a promising surveillance technique that can aid in early detection and management, potentially improving outcomes in patients with IMH.
4 Conclusion
In coronary angiography and related interventional procedures, myocardial hematoma, a complication that demands attention, is found in this study to be associated with significant risk factors such as catheter entrapment, excessive insertion depth, prolonged injection time, and large dosage of contrast medium; the findings offer guidance for optimizing procedures and reducing risks in clinical practice, and it is necessary in the future to develop more comprehensive and standardized operating protocols and preventive strategies to enhance treatment safety and effectiveness and safeguard patients' health.
Acknowledgments
We thank Dr. Chongyi Wang for providing the second case for this study. And we thank AiMi Academic Services (www.aimieditor.com) for English language editing and review services.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.




