Long-term (8 year) outcomes and predictors of major adverse cardiac events after full metal jacket drug-eluting stent implantation
Conflict of interest: Nothing to report.
Abstract
Objectives
We examined long-term outcomes and predictors of major adverse cardiac events after the full metal jacket (FMJ) stent implantation.
Background
The FMJ procedure has been used to treat diffuse coronary artery disease (CAD), but long-term outcomes remain unknown.
Methods
The study population consisted of 347 consecutive patients (352 lesions) who had been treated for de novo diffuse CAD with FMJ stents (stent length ≥ 60 mm).
Results
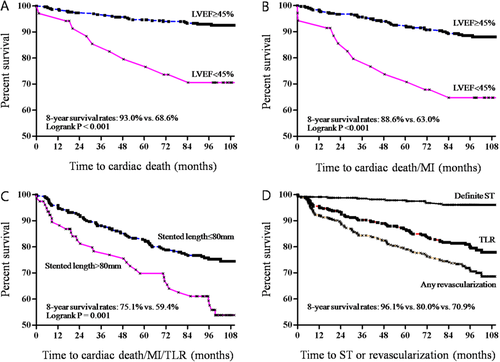
The mean age was 61.0 ± 10.1 years, and the stent length was 71.9 ± 13.7 mm. The procedural success rate was 97.7%. Major in-hospital complications (one death and two acute stent thromboses) occurred in three patients (0.7%). The median follow-up was 101 months (interquartile range, 95–108 months). During follow-up, there were 60 deaths (33 cardiac), 20 myocardial infarctions, and 94 revascularizations. Definite stent thrombosis occurred in 12 patients. The event-free survival rate for cardiac death, cardiac death/myocardial infarction, or cardiac death/myocardial infarction/target lesion revascularization was 90.5 ± 1.6, 85.8 ± 1.9, and 71.6 ± 2.5% at 8 years, respectively. Left ventricular dysfunction (ejection fraction < 45%) was an independent predictor of cardiac death (OR: 4.88; 95% CI: 1.81–13.13; P = 0.002). Left ventricular dysfunction and a stent length > 80 mm were significantly related to cardiac death/myocardial infarction. Likewise, a stent length > 80 mm was an independent predictor of cardiac death/myocardial infarction/target lesion revascularization (OR: 2.45; 95% CI: 1.16–5.19; P = 0.019).
Conclusion
Long-term outcomes appear favorable after FMJ procedures, and left ventricular dysfunction and a stent length > 80 mm are major predictors of major adverse cardiac events. These findings might be useful in identifying the most suitable treatments for patients with very diffuse CAD. © 2013 Wiley Periodicals, Inc.
INTRODUCTION
Since the advent of drug-eluting stents (DES), the full metal jacket (FMJ) stenting procedure has often been used to treat diffuse coronary artery disease (CAD). Previous studies have shown acceptable short- and medium-term outcomes from the FMJ procedure 1-6. However, long-term outcome data are limited, and there is controversy on the efficacy and safety of this approach 7. In this study, we conducted an extended follow-up of our previous cohort to examine long-term outcomes and predictors of major adverse cardiac events after the FMJ procedure.
METHODS
The study design and methods have been previously described 3. In brief, the study population consisted of 347 consecutive patients (352 lesions) at the Asan Medical Center who had been treated for de novo diffuse CAD with FMJ stents, defined as a stent length ≥ 60 mm without gaps, between February 2003 and May 2005. A Cypher™ (Cordis Corporation, Miami Lakes, FL) or Taxus™ (Boston Scientific Corporation, Natick, MA) stent was used in all patients. Stent implantation was performed according to standard techniques. Complete lesion coverage was recommended as well as angiographic optimization with <20% residual stenosis by visual estimate. All patients were pretreated with aspirin and clopidogrel. Aspirin (100–200 mg/day) was used indefinitely, and clopidogrel (75 mg/day) was used for at least 6 months. All patients also received the drug with the appropriate standard of care, which was provided at the discretion of the physicians.
Angiographic analyses were performed by two experienced angiographers. Percent diameter stenosis, minimal lumen diameter, and reference diameter using an online quantitative angiographic analysis system (XceleraCath 1.1, Philips, the Netherlands) were measured before pre-dilation and after the stenting procedure. All demographic, clinical, angiographic, and procedural characteristics were prospectively entered into the Asan Medical Center database. Echocardiographic examination was performed before angioplasty, and left ventricular ejection fraction was calculated according to a modified Simpson's rule.
Follow-up information was obtained by chart review and telephone interview. Final follow-up status was ascertained between January and February 2013, and follow-up was completed for 92.2% of patients. The unique personal identification number from the National Population Registry of the Korea National Statistical Office was used to determine the vital status of the remaining 27 patients (7.8%) who could not be contacted. All deaths were considered to be from cardiac causes unless an unequivocal non-cardiac cause could be established. The diagnosis of acute myocardial infarction was based on the universal definition of myocardial infarction 8. Stent thrombosis was defined as the definite occurrence of a thrombotic event, according to the Academic Research Consortium classification 9. Repeat revascularization was defined as any percutaneous or surgical revascularization procedure, irrespective of whether it was performed on a target or non-target lesion.
Data were expressed as the mean ± SD for continuous variables and as frequencies for categorical variables. Continuous variables were compared using the unpaired Student's t-test and categorical variables were compared using the chi-square test. Cumulative event rates were calculated by using the Kaplan–Meier method, and groups were compared by the log-rank test. A Cox proportional-hazards regression model was used to identify predictors of major adverse cardiac events. Statistical significance was defined as a two-sided value of P < 0.05.
RESULTS
The mean age of the patients was 61.0 ± 10.1 years (range, 31–86 years). A total of 72.6% were men, 57.9% had a history of hypertension, 36.3% had diabetes, 28.0% were current smokers, 74.1% had multi-vessel diseases, and 10.4% had left ventricular dysfunction (ejection fraction < 45%). Sirolimus-eluting stents were used in 75.6% of the treated lesions, while paclitaxel-eluting stents were used in the remaining 24.4% of treated lesions. Baseline angiographic and procedural characteristics are summarized in Table 1. The lesion length was 55.8 ± 12.9 mm, the reference vessel diameter was 2.82 ± 0.40 mm, the number of stent overlaps per lesion was 2.5 ± 0.7 (range, 2–6), and the total stent length was 71.9 ± 3.7 mm (range, 60–150 mm).
| Characteristics | N = 352 |
|---|---|
| Lesion characteristics | |
| Target coronary vessel | |
| Left anterior descending | 193 (54.8%) |
| Left circumflex artery | 14 (4.0%) |
| Right coronary artery | 124 (35.1%) |
| Left main to left anterior descending | 22 (6.3%) |
| Chronic total occlusion | 60 (17%) |
| Ostial lesion | 40 (11.4%) |
| Bifurcation | 54 (15.3%) |
| Procedural characteristics | |
| Balloon to artery ratio | 1.32 ± 0.18 |
| Direct stenting | 15 (4.3%) |
| Maximal inflation pressure (atm) | 15.5 ± 3.5 |
| Stents per lesion | 2.5 ± 0.7 |
| Stent length per lesion (mm) | 71.9 ± 13.7 |
| Quantitative coronary angiography | |
| Lesion length (mm) | 55.8 ± 12.9 |
| Reference vessel diameter (mm) | 2.82 ± 0.40 |
| Pre-intervention | |
| Minimal lumen diameter (mm) | 0.66 ± 0.53 |
| Diameter stenosis (%) | 68.5 ± 13.5 |
| Post-intervention | |
| Minimal lumen diameter (mm) | 2.66 ± 0.40 |
| Diameter stenosis (%) | 4.5 ± 13.4 |
| Acute gain (mm) | 1.99 ± 0.58 |
| Intravascular ultrasound guidance | 256 (72.7%) |
The procedural success rate was 97.7%. The incidence of procedural non-Q-wave myocardial infarction was 19.6%. During hospitalization, major complications occurred in three patients (0.9%). One patient died of cardiac tamponade immediately after the procedure. Two other patients developed acute stent thrombosis with Q-wave myocardial infarction 4 and 12 days after surgery, respectively. The remaining patients were discharged without complications.
Patients were followed up for 10 years, with a median follow-up of 101 months (interquartile range, 95–108 months). During follow-up, 60 deaths occurred (33 cardiac, 27 non-cardiac), 20 myocardial infarctions, and 94 revascularizations (64 target lesion revascularizations and 30 new lesion revascularizations). Definite stent thrombosis occurred in 12 patients. The cumulative probability of survival without major adverse cardiac events is shown in Fig. 1. The event-free survival rates for cardiac death, cardiac death/myocardial infarction, or cardiac death/myocardial infarction/target lesion revascularization were 90.5 ± 1.6%, 85.8 ± 1.9%, and 71.6 ± 2.5% at 8 years, respectively. As shown in Fig. 1 and Table 2, left ventricular dysfunction (ejection fraction < 45%) was an independent predictor of cardiac death (odds ratio [OR], 4.88; 95% CI: 1.81–13.13; P = 0.002). Left ventricular dysfunction and a stent length >80 mm were significantly related to cardiac death/myocardial infarction. Likewise, a stent length >80 mm was an independent predictor of cardiac death/myocardial infarction/target lesion revascularization (OR, 2.45; 95% CI: 1.16–5.19; P = 0.019). No other factors including types of DES were related to major adverse cardiac events.
| Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|
| Variables | OR | 95% CI | P | OR | 95% CI | P |
| Cardiac death | ||||||
| LVEF < 45% | 4.54 | 2.15–9.58 | <0.001 | 4.88 | 1.81–13.13 | 0.002 |
| Stent length > 80 mm | 2.52 | 1.25–5.11 | 0.010 | 2.29 | ||
| Insulin requiring DM | 2.70 | 1.07–6.86 | 0.036 | 1.89 | ||
| Cardiac death/MI | ||||||
| LVEF < 45% | 3.57 | 1.85–6.90 | <0.001 | 3.04 | 1.55–5.96 | 0.001 |
| Stent length > 80 mm | 2.50 | 1.38–4.53 | 0.002 | 2.15 | 1.17–3.93 | 0.014 |
| Cardiac death/MI/TLR | ||||||
| Stent length > 80 mm | 2.02 | 1.32–3.10 | 0.001 | 2.45 | 1.16–5.19 | 0.019 |
| Insulin requiring DM | 2.12 | 1.21–4.00 | 0.021 | 1.69 | ||
| LVEF < 45% | 1.91 | 1.10–3.31 | 0.022 | 1.57 | ||
| Mean RVD < 2.5 mm | 1.83 | 1.08–3.10 | 0.024 | 1.17 | ||
- CI, confidence interval; LVEF, left ventricular ejection fraction; DM, diabetes mellitus; MI, myocardial infarction; OR, odds ratio; RAD, reference vessel diameter.
DISCUSSION
This study showed that long-term outcomes are favorable after FMJ DES implantation, and left ventricular dysfunction and a stent length >80 mm are key predictors of major adverse cardiac events. These findings might be helpful when choosing treatment modalities for patients with diffuse CAD.
Patients with advanced CAD are expected to increase in accordance with improved life expectancy. The introduction of DES has allowed interventional cardiologists to tackle very diffuse CAD, and the FMJ approach has been used. However, many challenges remain in this approach because of frequent peri-procedural myocardial infarction, problems with future bypass surgery, and a lack of long-term outcome data. The more serious concern in using DES is the ongoing hazard of stent thrombosis, with a continuing rate of ∼0.6%/year for very late stent thrombosis 10. Despite the FMJ stenting procedure, stent thrombosis in our study was relatively low with ∼0.5%/year. However, cardiac death was significantly higher in patients with left ventricular dysfunction than those with preserved left ventricular function. Likewise, the composite outcome of cardiac death or myocardial infarction more frequently occurred in patients with left ventricular dysfunction or a stent length >80 mm. These findings suggest that patients with left ventricular dysfunction or very diffuse CAD might not be good candidates for the FMJ approach.
Sirolimus-eluting stents have been shown to be more effective than paclitaxel-eluting stents for up to 1 year 11. However, a 5-year follow-up showed no differences in clinical and angiographic outcomes between the two DES 12. In our study, there was no difference in target lesion revascularization between sirolimus- and paclitaxel-eluting stents (21.0% vs. 16.4% at 8 years, respectively, Log rank P = 0.654), supporting a late catch-up phenomenon of sirolimus-eluting stents. In addition, the composite outcome of cardiac death, myocardial infarction, or target lesion revascularization was independently related to a stent length >80 mm, indicating that other treatment options should be considered for patients requiring this stent length. Furthermore, the FMJ approach for left anterior descending CAD can make future bypass surgery difficult and is therefore used as a last resort.
DES technology has rapidly advanced over the past decade, and late stent thrombosis may be less of a clinical issue with the use of new-generation DES. The superiority of new DES over previous DES can be seen in the reduced risk of stent thrombosis 13, 14. Therefore, the FMJ approach with new DES seems to have better long-term outcomes compared with previous DES. However, most randomized trials comparing sirolimus-eluting stents with everolimus-eluting stents showed similar efficacy and safety outcomes 15, 16. In our study, sirolimus-eluting stents were predominantly used. Therefore, even in an era of new DES, our findings are helpful to determine appropriate therapeutic options for patients with very diffuse CAD.
Several potential limitations of this study should be noted. First, less modern DES were used in this study. It is likely that long-term outcomes would have been different if new-generation DES had been used. Second, the lack of a control group treated with bypass surgery or medical therapy precluded the determination of the role of treatment differences on clinical outcomes.
CONCLUSIONS
Long-term outcomes appear favorable after FMJ DES implantation, and left ventricular dysfunction and a stent length >80 mm are major predictors of major adverse cardiac events.