Older adults living with gastrointestinal cancers in 2021
Pojsakorn Danpanichkul and Yanfang Pang contributed equally to this work.
List of Abbreviations
-
- APC
-
- annual percent change
-
- ASDALY
-
- age-standardized disability-adjusted life year
-
- ASIR
-
- age-standardized incidence rate
-
- ASPR
-
- age-standardized prevalence rate
-
- ASR
-
- age-standardized rate
-
- CI
-
- confidence interval
-
- CODEm
-
- cause of death ensemble model
-
- DALY
-
- disability-adjusted life year
-
- GBD
-
- Global Burden of Disease
-
- GHDx
-
- Global Health Data Exchange
-
- GI
-
- gastrointestinal
-
- HBV
-
- hepatitis B virus
-
- HCV
-
- hepatitis C virus
-
- MASH
-
- metabolic dysfunction-associated steatohepatitis
-
- MetALD
-
- metabolic dysfunction and alcohol-associated liver disease
-
- SDI
-
- sociodemographic index
-
- UI
-
- uncertainty interval
The global average life expectancy is projected to rise to 80 years by 2040 [1]. Since cancer is closely linked to aging, its prevalence is expected to grow as the population ages. Advancements in cancer diagnosis and treatment have led to an increasing number of cancer survivors. In a 2021 consensus statement, the International Society for Geriatric Oncology updated its top priorities for improving care for older cancer patients [2, 3]. According to the Global Burden of Disease (GBD) study, there were over four million deaths from gastrointestinal (GI) cancer in 2021 [4].
The aging population, advancements in cancer management, and shifting risk factors are undoubtedly influencing the prevalence of GI cancers in older adults [5]. While aging has increasingly captured the attention of policymakers and stakeholders, epidemiological data on GI cancers in older adults remains limited. Older patients are also underrepresented in GI-specific clinical trials. This study aimed to estimate the global burden of GI cancers in older adults using the most recent GBD 2021 [6].
The general methods used for estimating disease burden in the GBD 2021 study, including GI cancer, have been detailed in previous publications [4, 6]. Briefly, data were sourced from population-based cancer registries, vital registration systems, and verbal autopsy studies (Supplementary Information S1). This GBD database defines older adults as individuals aged 70 and above. The GBD 2021 study utilized the International Classification of Disease-Tenth and Ninth Revision for GI cancers. We assessed the burden of various GI cancers in older adults, including colorectal, esophageal, liver, biliary tract, pancreatic, and gastric cancers. For liver cancer, we further analyzed the burden by five main etiologies: alcohol, chronic hepatitis B virus (HBV) infection, chronic hepatitis C virus (HCV) infection, metabolic dysfunction-associated steatohepatitis (MASH), and other causes. Several statistical methods were applied to ensure data consistency, including misclassification correction, garbage code redistribution, and noise reduction algorithms. Mortality rates were evaluated using the Cause of Death Ensemble model (CODEm), which employed Bayesian geospatial regression to account for spatial relationships in the data. The detailed CODEm methodology is listed in Supplementary Information S1. Countries were classified based on their level of development using the sociodemographic index (SDI) (Supplementary Information S2).
The incidence, prevalence, and disability-adjusted life years (DALYs) (i.e., years of life lost plus years lost due to disability) estimates were reported with a 95% uncertainty interval (UI), calculated as the 2.5th and 97.5th percentiles from a posterior distribution of 1,000 draws. Broader UIs indicate higher uncertainty, typically resulting from limited or lower-quality data, whereas narrower UIs suggest more reliable estimates. Age-standardized rates (ASRs) are calculated using the GBD 2021 standard population, developed through a robust Bayesian hierarchical cohort component model. This model integrates data from censuses, population registries, and migration statistics, ensuring consistent age-specific population estimates across all GBD metrics [7]. To evaluate changes from 2000 to 2021, the difference between the values in 2021 and 2000 was divided by the 2000 value. The Joinpoint regression program estimated the annual percent change (APC) and the corresponding 95% confidence interval (CI) in ASRs. Statistical differences between subgroups are demonstrated by non-overlapping CI.
There were 2.46 million incident cases, 6.56 million cases, and 29.16 million DALYs from GI cancer in older adults. From 2000 to 2021, incidence increased by 71%, prevalence increased by 93%, and DALYs increased by 49% (Figure 1A-C). Colorectal cancer had the highest incidence (1.04 million), followed by gastric cancer (571,500), pancreatic cancer (269,330), esophageal cancer (253,060), liver cancer (198,110), and biliary tract cancer (121,790) (Figure 1A). Colorectal cancer also had the highest prevalence (4.74 million), followed by gastric cancer (885,540), esophageal cancer (344,330), liver cancer (226,300), pancreatic cancer (200,720), and biliary tract cancer (162,450) (Figure 1B). Finally, colorectal cancer had the highest DALYs (8.85 million), followed by gastric cancer (7.47 million), pancreatic cancer (4.19 million), esophageal cancer (4.06 million), liver cancer (3.11 million), and biliary tract cancer (1.48 million) (Figure 1C). ASRs are shown in Figure 1D-F.
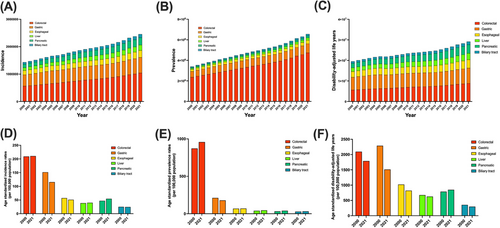
Incidence, prevalence, disability-adjusted life years, and rate per 100,000 population from GI cancer in older adults.
(A) Incidence cases from 6 types of GI cancers in older adults from 2000 to 2021. (B) Prevalences from 6 types of GI cancers in older adults from 2000 to 2021. (C) Disability-adjusted life years lost from 6 types of GI cancers in older adults from 2000 to 2021. (D) Age-standardized incidence rates per 100,000 populations in older adults in 2000 and 2021 for 6 types of GI cancers. (E) Age-standardized prevalence rates per 100,000 populations in older adults in 2000 and 2021 for 6 types of GI cancers. (F) Age-standardized disability-adjusted life years per 100,000 populations in older adults in 2000 and 2021 for 6 types of GI cancers.
Abbreviations: GI, gastrointestinal.
From 2000 to 2021, the incidence, prevalence, and DALYs all increased by 71%, 93%, and 49%, respectively. In this timeframe, the age-standardized incidence rate (ASIR) among older adults increased for pancreatic cancer (APC, 0.67%; 95% CI, 0.59% to 0.76%), liver cancer (APC, 0.15%; 95% CI, 0.06% to 0.23%), and colorectal cancer (APC, 0.06%; 95% CI, 0.02% to 0.09%), while it decreased for gastric cancer (APC, -1.27%; 95% CI, -1.46% to -1.08%) and esophageal cancer (APC, -0.52%; 95% CI, -0.74% to -0.30%), and remained stable for biliary tract cancer. The age-standardized prevalence rate (ASPR) increased for pancreatic cancer (APC, 0.95%; 95% CI, 0.86% to 1.03%), liver cancer (APC, 0.60%; 95% CI, 0.56% to 0.65%), biliary tract cancer (APC, 0.50%; 95% CI, 0.39% to 0.62%), and colorectal cancer (APC, 0.42%; 95% CI, 0.40% to 0.45%), decreased for gastric cancer (APC, -0.78%; 95% CI, -0.87% to -0.68%), and remained stable for esophageal cancer. Age-standardized DALYs (ASDALYs) from gastric cancer (APC, -1.97%; 95% CI, -2.16% to -1.77%), esophageal cancer (APC, -1.06%; 95% CI, -1.27% to -0.85%), biliary tract cancer (APC, -0.80%; 95% CI, -0.88% to -0.73%), colorectal cancer (APC, -0.74%; 95% CI, -0.83% to -0.66%), and liver cancer (APC, -0.39%; 95% CI, -0.63% to -0.14%) decreased. However, ASDALYs for pancreatic cancer (APC, 0.36%; 95% CI, 0.22% to 0.50%) increased (Supplementary Tables S1-S6). Results by country is listed in Supplementary Figure S1 and Supplementary Tables S7-S12. The burden of GI cancer among older adults stratified by sex, region, and SDI is detailed in Supplementary Figure S2 and Supplementary Information S3-S5.
Our study provides the most up-to-date assessment of the global GI cancer trends among older adults in the past two decades. In 2021, there were 6.56 million older adults living with GI cancer and 2.46 million incidences. Prevalence increased by 93%, and incidence increased by 71% from 2000 to 2021, with the main drivers being colorectal, pancreatic, and liver cancer. Older patients are frequently overlooked in trials, although the increasing incidence and prevalence in older adults highlights a need to start including them [8].
ASDALYs decreased in most types of GI cancer in older adults, although overall, DALYs increased. These contrasting trends suggest improved individual disease outcomes, likely due to better management; however, the increase in DALYs reflects an aging global population. Furthermore, ASDALYs still increased in pancreatic and MASH-associated liver cancer. Although widespread use of antiviral treatments for chronic HBV and HCV infections has significantly reduced liver disease mortality, increases in obesity and alcohol abuse have resulted in increases in non-viral-related HCC.
Our study showed several limitations. First, the analysis relied on GBD 2021 data, which depends on the quality of vital registration systems, particularly in countries with limited data quality. Methods to address missing or unreliable data in vital registration systems, especially in low-SDI regions, were detailed in the GBD capstone publication; however, sensitivity analyses to evaluate the robustness of imputation methods were not possible, given a lack of raw data [6]. GBD also does not provide alternative modeling choices. Second, due to methodological limitations, we were unable to quantify the burden based on specific subtypes, such as the rising trends in metabolic dysfunction and alcohol-associated liver disease (MetALD) or intrahepatic cholangiocarcinoma. Third, older adults were defined as over 70 per GBD's predefined age groups, and other cut-offs could not be evaluated. Fourth, GBD does not provide alternative modeling methods or detailed raw data, such as Root Mean Square Error or out-of-sample accuracy. Fifth, our study did not account for detailed factors like comorbidities and frailty, which can influence the cancer burden in older adults. Aging is a universal process, yet unique to each individual. Evaluating functional age, including other factors, is key to making informed medical decisions.
In conclusion, our study evaluated the global impact of GI cancers and found that approximately 6.56 million older adults are living with these cancers, a number that has nearly doubled over the past two decades. The change occurred heterogeneously among cancer types, regions, and socioeconomic status. As the global population ages, it is critical to strengthen geriatric oncology to support older patients throughout the cancer care continuum [2, 3]. This research underscores the importance of considering this vulnerable group when developing public health policies to address the growing burden of GI cancer. For clinicians, key assessments for older adults include Instrumental Activities of Daily Living for function, comorbidities, fall risk, and screenings for depression, nutrition, and cognition [2, 9]. Training healthcare providers is essential, and this study will support the development of a geriatric oncology curriculum for oncology trainees.
AUTHOR CONTRIBUTIONS
Conceptualization: Pojsakorn Danpanichkul, Karn Wijarnpreecha, and Ju Dong Yang. Data curation: Pojsakorn Danpanichkul and Kwanjit Duangsonk. Formal analysis: Pojsakorn Danpanichkul, Yanfang Pang, Nicole Shu Ying Tang, and Benjamin Nah. Investigation: Pojsakorn Danpanichkul, Kwanjit Duangsonk, and Yanfang Pang. Methodology: Pojsakorn Danpanichkul, Kwanjit Duangsonk, and Yanfang Pang. Project Administration: Pojsakorn Danpanichkul, Amit G. Singal, and Ju Dong Yang. Supervision: Karn Wijarnpreecha, Amit G. Singal, and Ju Dong Yang. Validation: Pojsakorn Danpanichkul, Torlap Inkongngam, and Kornnatthanai Namsathimaphorn, Krittameth Rakwong, Yanfang Pang, and Chuthathip Kaeosri. Visualization: Pojsakorn Danpanichkul, Torlap Inkongngam, Kornnatthanai Namsathimaphorn, Krittameth Rakwong, Yanfang Pang, and Chuthathip Kaeosri. Writing, original draft: Pojsakorn Danpanichkul, Torlap Inkongngam, Kornnatthanai Namsathimaphorn, Krittameth Rakwong, Kwanjit Duangsonk, Neha Mittal, and Nicole Shu Ying Tang. Writing, review, and editing: Pojsakorn Danpanichkul, Karn Wijarnpreecha, Donghee Kim, Ju Dong Yang, Amit G. Singal, Michael B. Wallace, and Mazen Noureddin. All authors have read and approved the final version of the manuscript for submission.
ACKNOWLEDGEMENTS
The figures for the world maps were created using mapchart.net.
CONFLICT OF INTEREST STATEMENT
Michael B. Wallace declared the conflict of interest as designated below: Cosmo/Aries Pharmaceuticals, Verily, Boston Scientific, Endiatix, Intervenn, AlphaMed UAE, Fujifilm for consulting; Fujifilm, Boston Scientific, Olympus, Medtronic, Ninepoint Medical, Cosmo/Aries Pharmaceuticals for Research grants; Virgo Inc for Stock/Stock Options; Boston Scientific. Microtek for consulting on behalf of Mayo Clinic, Boston Scientific, and Cook Medical for General payments/Minor Food and Beverage. Ju Dong Yang consults for AstraZeneca, Eisai, Exact Sciences, and FujiFilm Medical Sciences. Amit G. Singal has served as a consultant or on advisory boards for Genentech, AstraZeneca, Eisai, Exelixis, Bayer, Elevar, Boston Scientific, Sirtex, Histosonics, FujiFilm Medical Sciences, Exact Sciences, Roche, Abbott, Glycotest, Freenome, and GRAIL. Mazen Noureddin has been on the advisory board for 89BIO, Gilead, Intercept, Pfizer, Novo Nordisk, Blade, EchoSens, Fractyl, Terns, Siemens, and Roche diagnostic; has received research support from Allergan, BMS, Gilead, Galmed, Galectin, Genfit, Conatus, Enanta, Madrigal, Novartis, Pfizer, Shire, Viking and Zydus; and is a minor shareholder or has stocks in Anaetos, Rivus Pharma and Viking.
All other coauthors denied conflict of interest.
FUNDING INFORMATION
Not applicable.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study does not involve any ethical problem and data collection was completed in accordance with the ethical regulations.
Open Research
DATA AVAILABILITY STATEMENT
Data from the GBD study in 2021 can be accessed using the Global Health Data Exchange (GHDx) query tool (http://ghdx.healthdata.org/gbd-results-tool) which the Institute for Health Metrics and Evaluation maintains. The GBD data does not require licensing for non-commercial use.




