Incidence of and survival with bone and soft tissue sarcoma: A nation-wide study over four decades
Abbreviations
-
- AAPC
-
- average annual percentage change
-
- BS
-
- bone sarcoma
-
- CI
-
- confidence interval
-
- STS
-
- soft tissue sarcoma
Demographic and environmental factors determine the incidence of and survival with malignancies, including sarcoma [1]. Accordingly, the annual incidence of soft tissue sarcomas (STS) has markedly increased since the early 2000s [2, 3]. Likewise, there appears to be an overall increase in the incidence of bone sarcomas (BS) since 1975 [4, 5]. In parallel, one study reports moderate improvement in the survival of adult patients with BS and STS up to 2007 [6]. Previous studies were often based on cancer registries with low coverage rates [3, 7, 8], focused on limited time periods [3, 9, 10], or did not include data from recent years [3, 6]. Thus, current data from high-income European countries with an advanced health care system on incidence and prognosis of sarcoma patients are scarce. Consequently, the purpose of this study was to analyse the incidence of and survival with BS and STS in the general population of Austria from 1983 to 2020. A detailed description of materials and methods is outlined in the Supplementary Materials (Supplementary Materials and Methods).
Across the 38-year observation period, 2,491 patients in Austria were diagnosed with BS (Supplementary Tables S1-S2, Supplementary Figure S1). Male-to-female ratio was 1.27, favouring males (range over the years: 0.56-1.23), which remained constant over time (P = 0.529; Supplementary Table S3).
Throughout the observation period, mean age-adjusted BS incidence was 0.80 per 100,000 (95% confidence interval [CI]: 0.61-0.98; Figure 1A). We observed a significant increase in incidence from 1983 to 2020, with an average annual percentage change (AAPC) of 7.2% (95%CI: 6.2%-8.5%; P < 0.001; Supplementary Table S4). Similar results were obtained in a sensitivity analysis excluding the initial 7 years of the observation period (ie, 1983-1989; AAPC: 1.5% [95%CI: 1.0%-2.1%]; P < 0.001) and chondrosarcoma diagnoses (AAPC: 5.8% [95%CI: 4.9%-7.2%]; P < 0.001; Supplementary Figure S2A; Supplementary Table S4).
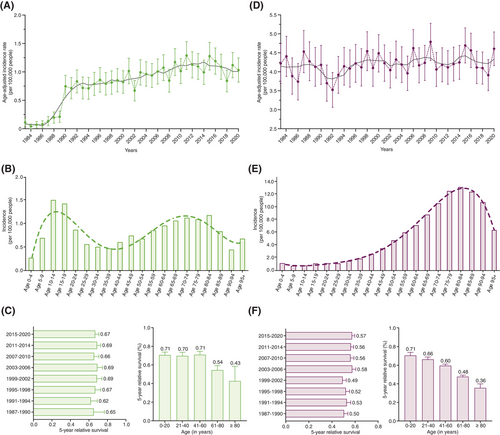
Age at diagnosis of BS followed a bimodal distribution, with peaks in incidence around the age of 15 years and 70 years (Figure 1B), both in males and females (Supplementary Figure S3A). Notably, a shift towards increased BS incidence in older age groups was present in recent years (Supplementary Figure S4A, Supplementary Figure S5A). In a sensitivity analysis excluding all chondrosarcoma diagnoses, a similar pattern was observed (Supplementary Figure S2B).
Five-year relative survival was 65.9% (95%CI: 63.9%-67.9%). No change in 5-year relative survival was found from the first time period (1987-1990; 5-year relative survival: 65.3% [95%CI: 50.7%-76.7%]) to the last time period (2015-2020; 5-year relative survival: 66.7% [95%CI: 62.5%70.7%]; P = 0.735; Figure 1C). Of note, the youngest age group (0-20 years) had better 5-year relative survival than the oldest age group (≥ 81 years; P < 0.001; Supplementary Table S5, Figure 1C).
From 1983 to 2020, 11,893 diagnoses of STS had been documented across Austria (Supplementary Tables S1-S2). Over the years, male-to-female ratio ranged from 0.56 to 1.23, with an average of 0.86, and a significant trend towards female predominance (P < 0.001; Supplementary Table S3).
Age-adjusted incidence for STS amounted to 4.20 (95%CI: 3.72-4.68; Figure 1D). Over the entire observation period, there was no change in incidence (AAPC: 0.1% [95%CI: -0.1%-0.3%]; P = 0.260; Supplementary Table S4).
Two age peaks in STS incidences were observed, one small one in age groups 0-4 years, and a second, pronounced peak from 75 years onwards (Figure 1E; Supplementary Figure S3B). Notably, in recent years, there was a shift towards higher incidences in older age groups (Supplementary Figure S4B, Supplementary Figure S5B).
Five-year relative survival for STS was 53.6% (95%CI: 52.6%-54.7%). Over the entire observation period, 5-year relative survival improved significantly (P = 0.001; Figure 1F). A significant reduction in 5-year relative survival was observed between age groups 21-40 and 41-60 (P < 0.001), 41-60 and 61-80 (P < 0.001), and 61-80 and ≥ 81 years (P < 0.001; Figure 1F; Supplementary Table S5).
We here report an increase in BS incidence in Europe (average, 7.2% per year). The incidence of STS, on the other hand, remained stable. Furthermore, we discovered a shift in STS incidences from younger to older age groups, especially in more recent years of observation, aligning with findings from Australia [2]. Similarly, a time-dependent shift in the well-known bimodal age distribution [3] of BS from younger to older age groups was present. This shift appeared to be neither driven by the known peak incidence of chondrosarcoma diagnoses between ages 40 and 60 years, nor by an increase in diagnoses of atypical cartilaginous tumours (ACTs; chondrosarcoma G1).
We found constant 5-year survival rates in BS patients, averaging 65.9%. In contrast, there was a trend towards improved 5-year relative survival of STS patients from the first (50.5%) to the last time period (57.4%), in line with previous studies [2, 6, 7].
Our study has several strengths, including data deriving from a nation-wide cancer registry with standardised reporting, internal review and low death-certificate only rate. Further, the Austrian health care system is characterised by low-key access to any level of the system, and a relatively uniform public health sector with only little variations between counties, ensuring country-wide high-quality care.
Some limitations warrant consideration. First, numbers reported must be interpreted bearing in mind the low population size of Austria (∼9 million inhabitants in 2020). Second, we did not stratify our analyses according to anatomical location, tumour grading or staging. Yet, subgroup-specific analyses of incidence and survival rates may be biased by low case numbers, changing diagnostic criteria, enhanced diagnostics, and raised awareness. Third, we observed a relative underreporting of sarcomas in general, and BS during the first few years of the observation period that cannot be fully explained given the compulsory entry of any patient with a cancer diagnosis in the Austrian National Cancer Registry. However, sensitivity analyses excluding the first 7 years of the observation period with lower reporting rate, as well as all chondrosarcoma diagnoses (including both low- and high-grade chondrosarcomas) yielded similar results. In addition, an underreporting of sarcoma diagnoses in the elderly population due to other, more predominant illnesses, poor general health, and inability or reluctance to consult medical professionals, cannot be ruled out. Yet, our study design precludes definite evidence on this point.
Our findings suggest a growing health care burden due to BS, given the expensive and time-consuming treatment of these malignancies. This study shows that both BS and STS are increasingly common in elderly individuals. Five-year relative survival remained unchanged for BS patients, while it significantly improved for STS patients, potentially reflecting the increasing implementation of multimodal treatment concepts.
AUTHOR CONTRIBUTIONS
Maria Anna Smolle: Conceptualization; methodology; funding acquisition; formal analysis; visualization, and writing—original draft version. Florian Alexander Wenzl: Methodology; formal analysis, and writing—original draft version. Joanna Szkandera: Supervision; validation, and writing—review & editing. Susanne Scheipl: Supervision; validation, and writing—review & editing. Bernadette Liegl-Atzwanger: Supervision; validation, and writing—review & editing. Jasminka Igrec: Supervision; validation, and writing—review & editing. Andreas Leithner: Project administration; funding acquisition; supervision; validation, and writing—review & editing.
ACKNOWLEDGEMENTS
The authors have nothing to report.
CONFLICT OF INTEREST STATEMENT
Maria Anna Smolle reports support for attending scientific meetings by implantcast, Alphamed Fischer, ImplanTec and PharmaMar, outside of the submitted word. Florian Alexander Wenzl reports research support by the Foundation for Cardiovascular Research— Zurich Heart House, Kurt und Senta Herrmann Foundation, Theodor und Ida Herzog-Egli Stiftung, 4TEEN4 Pharmaceuticals GmbH, PAM Theragnostics GmbH, and Sphingotec GmbH, financial support by the Research Funding for excellent research by the University of Zurich, Fonds zur Förderung des akademischen Nachwuchses of the University of Zurich, Amgen Switzerland, European Society of Cardiology, Swiss Society of Cardiology, Swiss Heart Foundation, and Medical University of Graz, support for attending scientific meetings by 4TEEN4 Pharmaceuticals GmbH, PAM Theragnostics GmbH, Sphingotec GmbH, European Society of Cardiology, Swiss Society of Cardiology, Foundation for Cardiovascular Research— Zurich Heart House, and Critical Care Clinical Trialists Consortium, support in biomarker measurements by Roche Diagnostics, 4TEEN4 Pharmaceuticals GmbH, PAM Theragnostics GmbH, and Sphingotec GmbH, as well as membership in the Steering Committee of the National Registry of Acute Myocardial Infarction in Switzerland, outside of the submitted work. Susanne Scheipl reports grants by FFG “MedSens”, support for attending meetings by Alphamed and PharmaMar, as well board membership in the Austrian Cancer Aid Styria, outside of the submitted work. Joanna Szkandera, Bernadette Liegl-Atzwanger, Jasminka Igrec and Andreas Leithner have no conflicts of interest to declare.
FUNDING INFORMATION
This study received funding by Stadt Graz Kulturamt (FIF-A 16-0299/2024-0001). The funding source had to influence on conceptualization, design, data collection, analysis, decision to publish, or preparation of the manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study has been approved by the institutional review board of the Medical University of Graz, Austria (IRB-No. 36-156 ex 23/24).
Open Research
DATA AVAILABILITY STATEMENT
The datasets generated and/or analysed during the current study are not publicly available due to regulatory issues but are available from the corresponding author on reasonable request.




