Cancer situation in China: an analysis based on the global epidemiological data released in 2024
Abstract
Background
Cancer remains a major cause of mortality and a significant economic burden in China. Exploring the disparities in cancer patterns and control strategies between China and developed countries may offer valuable insights for policy formulation and enhance cancer management efforts. This study examined the incidence, mortality, and disability-adjusted life year (DALY) burden of cancer in China, and compared these metrics with those observed in the United States (US) and the United Kingdom (UK).
Methods
Data on cancer incidence, mortality, and DALYs for China, the US, and the UK were sourced from the GLOBOCAN 2022 online database and the Global Burden of Disease 2021 study (GBD 2021). We utilized Joinpoint regression models to analyze trends in cancer incidence and mortality across these countries, calculating annual percent changes (APCs) and determining the optimal joinpoints.
Results
In 2022, China recorded around 4,824,703 new cancer cases and 2,574,176 cancer-related deaths, contributing to 71,037,170 DALYs. China exhibited a lower cancer incidence rate compared to the US and the UK. Although cancer-related mortality in China is slightly lower than that in the UK, it is significantly higher than that in the US. Additionally, China experienced significantly higher DALY rates compared to both the US and UK. The cancer landscape in China was also undergoing significant changes, with a rapid rise in the incidence and burden of lung, colorectal, breast, cervical, and prostate cancers. Meanwhile, the incidence and burden of stomach cancer continued to decline. Although the incidence of liver and esophageal cancers was decreasing, the burden of liver cancer was increasing, while the burden of esophageal cancer remained largely unchanged.
Conclusions
The cancer profile of China is shifting from that of a developing country to one more typical of a developed country. The ongoing population aging and the rise in unhealthy lifestyles are expected to further escalate the cancer burden in China. Consequently, it is crucial for Chinese authorities to revise the national cancer control program, drawing on successful strategies from developed countries, while also accounting for the regional diversity in cancer types across China.
List of abbreviations
-
- AAPC
-
- average annual percent change
-
- APC
-
- annual percent change
-
- ASIR
-
- age-standardized incidence rate
-
- ASMR
-
- age-standardized mortality rate
-
- CI
-
- confidence interval
-
- DALY
-
- disability-adjusted life year
-
- EBV
-
- Epstein-Barr virus
-
- GBD
-
- Global Burden of Disease
-
- GHDx
-
- Global Health Data Exchange
-
- H. pylori
-
- Helicobacter pylori
-
- HBV
-
- hepatitis B virus
-
- HPV
-
- human papillomavirus
-
- IARC
-
- International Agency for Research on Cancer
-
- IHME
-
- Institute for Health Metrics and Evaluation
-
- UK
-
- United Kingdom
-
- US
-
- United States
-
- WHO
-
- World Health Organization
1 BACKGROUND
Cancer is a leading cause of death globally, imposing a significant economic strain on public health systems [1, 2]. The incidence, mortality, and disability-adjusted life year (DALY) burden associated with cancer vary substantially across different countries and regions, with notable differences between developing and developed nations [3]. Various factors, such as ecological, environmental, demographic, cultural, and genetic influences, contribute to the wide-ranging cancer incidence rates, mortality rates, and DALY burdens [4]. Developed countries continuously update their cancer spectrum to optimize cancer control systems, while most developing countries have limited information on cancer.
As the largest developing country in the world, China bears a substantial cancer burden. Its cancer spectrum differs significantly from that of developed countries like the United States (US) and the United Kingdom (UK). Owing to swift economic and social progress, China is experiencing a significant shift from a cancer spectrum typical of developing countries to one characteristic of developed countries [5, 6]. The incidence and mortality rates of lung [7], breast [8], colorectal [9], and prostate cancers [10] have increased rapidly, while the rates of liver [11], stomach [12], esophageal [13], and cervical cancers [14] have remained high in China over the past few decades. To adapt to the current socio-economic conditions in China, it is essential to establish an effective cancer control system. The cancer prevention and control strategies of developed countries like the US and the UK offer valuable insights for China. Therefore, comparing cancer incidence rates, mortality rates, and DALYs between China and developed countries can provide useful references for enhancing cancer prevention and control efforts in China.
Here, we examined the rates and trends of cancer incidence, mortality, DALY burden, and control strategies in China, comparing them with those in the US and the UK. Our analyses were based on the data retrieved from the GLOBOCAN 2022 online database [15] and the Global Burden of Disease 2021 study (GBD 2021) [16]. By exploring the differences in cancer patterns and control strategies between these countries, we aimed to provide insights that could inform policy planning and enhance cancer control measures in China.
2 MATERIALS AND METHODS
2.1 Data sources
The data on cancer incidence and mortality used in this study were sourced from the GLOBOCAN 2022 online database (https://gco.iarc.fr/en) [15]. GLOBOCAN, a project led by the International Agency for Research on Cancer (IARC), provides national estimates for cancer incidence, mortality, and prevalence by site and sex across 185 countries and territories, covering 36 different cancer types [3]. All age-standardized incidence and mortality rates (ASIR and ASMR) in GLOBOCAN 2022 were calculated using the world standard population as a reference [3].
Data on DALYs attributable to cancers in China, the US, and the UK for the years 1990 and 2021 were sourced from the GBD 2021 online results tool (https://www.healthdata.org/research-analysis/gbd) [16], developed by the Institute for Health Metrics and Evaluation (IHME). The GBD project annually estimates mortality, years of life lost, years of life lived with disability, and DALYs by age and sex for 88 risk factors and combinations across 204 countries and territories and 811 subnational locations [17]. In this study, we presented estimates of DALYs per 100,000 population in 2021 for 32 cancer sites in China, the US, and the UK, categorized by sex and age. We also displayed percentage and rank changes in all-age and age-standardized DALY rates from 1990 to 2021 to highlight trends in the cancer burden across these countries. All age-standardized DALY rates were calculated using the GBD reference population [17].
The ASIRs and ASMRs of cancer for trend analysis were obtained from the Global Health Data Exchange (GHDx) (https://ghdx.healthdata.org/) via the GBD results tools repository (https://vizhub.healthdata.org/gbd-results/). The search parameters were “total cancers”, “tracheal, bronchus, and lung cancer”, “breast cancer”, “colon and rectum cancer”, “liver cancer”, “cervical cancer”, “stomach cancer”, “prostate cancer”, and “esophageal cancer” for cause; “incidence” and “deaths” for measurements; “China”, “United States of American”, and “United Kingdom” for location; “1990-2021” for years; “rate” for metrics; “male, female and both” for sex; and “age-standardized” for age.
2.2 Statistical analysis
The joinpoint regression analysis is an effective method for analyzing trends over time to identify the time points in which the trend significantly changes. Therefore, we employed Joinpoint regression models [18] to analyze the temporal trends in ASIRs and ASMRs for selected cancer sites across China, the US, and the UK from 1990 to 2021. Using Joinpoint software (version 4.8.0.1; National Cancer Institute, Rockville, MD, US), we systematically assessed the time trends and identified statistically significant shifts between joinpoints. The models allowed for up to 3 segments (2 join-points). To quantify the direction and extent of these trends, the annual percent change (APC) was calculated. A trend was described as either “increasing” or “decreasing” when the slope (APC) significantly deviated from zero. The statistical significance of the trend was determined by examining their 95% confidence intervals (CIs). An APC with a 95% CI greater than zero was interpreted as a significant upward trend, whereas an APC with a 95% CI less than zero was considered a significant downward trend. If the 95% CI included zero, the ASIR or ASMR was considered stable. A P value of less than 0.05 was considered to indicate statistical significance.
3 RESULTS
3.1 Cancer incidence and mortality patterns in China, the US, and the UK
According to estimates from GLOBOCAN 2022, there were 19,976,499 new cancer cases (including non-melanoma skin cancer) diagnosed globally in 2022. Nearly 24.2% of these cases (4,824,703) were reported in China, comprising 2,533,906 males and 2,290,797 females. The ASIR for all cancers in China was 201.6 per 100,000 population (Supplementary Table S1). Males exhibited a higher ASIR compared to females (209.6 vs. 197.0 per 100,000 population, respectively). When both sexes are combined, lung cancer had the highest ASIR (40.8 per 100,000 population), followed closely by breast cancer (33.0 per 100,000 population; data pertains to females only), thyroid cancer (24.6 per 100,000 population), colorectal cancer (20.1 per 100,000 population), liver cancer (15.0 per 100,000 population), cervical cancer (13.8 per 100,000 population), stomach cancer (13.7 per 100,000 population), prostate cancer (9.7 per 100,000 population), and esophageal cancer (8.3 per 100,000 population; Figure 1A and Supplementary Table S1). Notably, in 2022, digestive cancers (including colorectal, stomach, liver, and esophageal cancers) accounted for 30.4% of all cancer cases diagnosed in China.
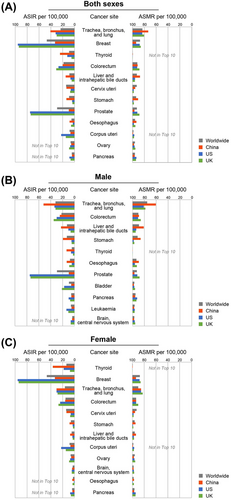
As detailed in Supplementary Table S2, approximately 2,574,176 individuals in China died from cancer (including non-melanoma skin cancer) in 2022, representing 26.4% (2,574,176 out of 9,743,832) of all cancer deaths globally. The ASMR for all cancers in China was 96.5 per 100,000 population. Men experienced an ASMR nearly 46.8% higher than that of women (127.5 per 100,000 population for men vs. 67.8 per 100,000 population for women). Lung cancer was the leading cause of cancer mortality, with an ASMR of 26.7 per 100,000 population, followed by liver cancer (12.6 per 100,000 population), stomach cancer (9.4 per 100,000 population), colorectal cancer (8.6 per 100,000 population), esophageal cancer (6.7 per 100,000 population), breast cancer (6.1 per 100,000 population), and cervical cancer (4.5 per 100,000 population; Figure 1A and Supplementary Table S2). Notably, the ASMR for digestive cancers was significantly higher compared to cancers from other systems.
In 2022, there were significant differences in cancer incidence and mortality between China, the US, and the UK. The ASIR for all cancers in China (201.6 per 100,000 population) was similar to the global average (196.9 per 100,000 population) but lower than that in the US (367.0 per 100,000 population) and the UK (307.8 per 100,000 population; Supplementary Table S1). However, the ASMR in China was significantly higher than that in the US but slightly lower than that in the UK (96.5 per 100,000 population in China compared to 82.3 per 100,000 population in the US and 98.3 per 100,000 population in the UK; Supplementary Table S2). The combined proportion of lung, breast, colorectal, and prostate cancers in China (42.9% of all new cases) was comparable to that in the US (37.4%) and the UK (47.1%; Supplementary Table S1). Unlike in the US and UK, where breast and prostate cancers were the most prevalent, lung and colorectal cancers were the most common in China (Supplementary Table S1). Cancers such as liver, stomach, esophageal, and cervical were more frequently diagnosed in China (22.8% of all new cases) than in the US (4.3%) and the UK (6.0%; Supplementary Table S1). These cancers accounted for 31.9% of all cancer deaths in China, whereas they were responsible for less than 12% of cancer deaths in either the US or UK (Supplementary Table S2).
Figure 1B and C summarized the top 10 cancer types by ASIR and ASMR for males and females across China, the US, and the UK in 2022. Lung and colorectal cancers were among the five most frequently diagnosed cancers for men in all three countries. However, Chinese men had significantly higher incidences of liver, stomach and thyroid cancers compared to their counterparts in the US and UK. Conversely, the ASIRs for prostate cancer, bladder cancer, and leukemia were higher among men in the US and UK than in China. For women, breast, lung, and colorectal cancers were the most common across the three countries. Chinese women showed a higher likelihood of developing thyroid and cervical cancers, while women in the US and UK had higher incidences of corpus uteri tumors. Notably, both men and women in China had higher ASMRs for stomach and liver cancers compared to those in the US and UK.
3.2 Temporal trends of cancer incidence and mortality in China, the US, and the UK
The time trend analysis in cancer incidence data from GHDx between 1990 and 2021 revealed that the ASIR for all cancers in Chinese men increased from 256.3 per 100,000 population in 1990 to 283.2 per 100,000 in 2011, followed by a period of stabilization until 2019 and a significant increase from 2019 to 2021 (Table 1). The ASIR for all cancers in Chinese women showed an upward trend until 2008, followed by a slight decrease until 2016, and then a notable rise between 2016 and 2021 (Table 1). However, the ASIR trends of all cancers in the US are quite different from that in China. Both sexes experienced a slight increase in ASIR from 1990 to 2000, followed by a sharp rise between 2000 and 2004/2005, and finally, a steady decline from 2004/2005 to 2021 (Table 1). Unlike China and the US, the ASIR for all cancers in the UK showed an overall downward trend from 1990 to 2021. For men in the UK, the ASIR remained relatively stable until 2016, and for women in the UK, until 2014. After these points, both sexes experienced a significant decline in ASIR through 2021 (Table 1). Additionally, the ASMR for both men and women in all three countries showed a significant decline during the study period, with the exception of Chinese men, who experienced a notable increase between 1997 and 2003 (Table 1).
| Country | Sex | ASIR/ASMR (per 100,000 population) | Trends 1 | Trends 2 | Trends 3 | 1990-2021, AAPC (95%CI) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1990 | 2021 | Years | APC (95%CI) | Years | APC (95%CI) | Years | APC (95%CI) | |||
| ASIR | ||||||||||
| China | Male | 256.3 | 317.6 | 1990-2011 | 0.6a (0.5 to 0.7) | 2011-2019 | 0.1 (−0.5 to 0.7) | 2019-2021 | 5.3a (0.9 to 9.9) | 0.8b (0.5 to 1.1) |
| Female | 167.7 | 210.7 | 1990-2008 | 0.3a (0.2 to 0.4) | 2008-2016 | −0.3 (−0.8 to 0.2) | 2016-2021 | 3.8a (3.0 to 4.6) | 0.7b (0.5 to 0.9) | |
| US | Male | 919.7 | 1415.4 | 1990-2000 | 0.7a (0.5 to 0.8) | 2000-2004 | 10.4a (9.6 to 11.2) | 2004-2021 | −0.2a (−0.3 to −0.2) | 1.4b (1.3 to 1.5) |
| Female | 654.1 | 931.4 | 1990-2000 | 0.4a (0.2 to 0.6) | 2000-2005 | 7.3a (6.6 to 8.0) | 2005-2021 | −0.3a (−0.4 to −0.3) | 1.1b (1.0 to 1.2) | |
| UK | Male | 429.7 | 389.4 | 1990-2011 | 0.1a (0 to 0.2) | 2011-2016 | −0.5 (−1.6 to 0.7) | 2016-2021 | −2.3a (−3.2 to −1.4) | −0.4b (−0.6 to −0.1) |
| Female | 360.1 | 330.3 | 1990-2002 | 0 (−0.2 to 0.1) | 2002-2014 | 0.4a (0.2 to 0.6) | 2014-2021 | −1.9a (−2.4 to −1.5) | −0.3b (−0.4 to −0.2) | |
| ASMR | ||||||||||
| China | Male | 243.0 | 190.3 | 1990-1997 | −0.8a (−1.2 to −0.3) | 1997-2003 | 0.8 (0 to 1.5) | 2003-2021 | −1.4a (−1.5 to −1.3) | −0.8b (−1.0 to −0.7) |
| Female | 137.9 | 93.5 | 1990-2004 | −0.9a (−1.0 to −0.8) | 2004-2014 | −2.7a (−2.9 to −2.4) | 2014-2021 | 0.1 (−0.3 to 0.5) | −1.2b (−1.3 to −1.1) | |
| US | Male | 217.2 | 140.6 | 1990-1994 | −0.4 (−0.9 to 0.1) | 1994-2002 | −1.5a (−1.7 to −1.3) | 2002-2021 | −1.7a (−1.7 to −1.6) | −1.5b (−1.6 to −1.4) |
| Female | 138.3 | 103.1 | 1990-1994 | 0.1 (−0.3 to 0.6) | 1994-2002 | −0.6a (−0.8 to −0.4) | 2002-2021 | −1.4a (−1.4 to −1.3) | −1.0b (−1.1 to −0.9) | |
| UK | Male | 240.9 | 158.2 | 1990-2008 | −1.6a (−1.7 to −1.6) | 2008-2018 | −0.6a (−0.8 to −0.4) | 2018-2021 | −2.6a (−3.8 to −1.3) | −1.4b (−1.5 to −1.3) |
| Female | 156.4 | 117.6 | 1990-2010 | −1.0a (−1.1 to −1.0) | 2010-2018 | −0.1 (−0.4 to 0.1) | 2018-2021 | −2.5a (−3.5 to −1.6) | −0.9b (−1.1 to −0.8) | |
- Abbreviations: ASIR, age-standardized incidence rate; ASMR, age-standardized mortality rate; APC, annual percent change; AAPC, average annual percent change; CI, confidence interval.
- a Indicates that the APC is significantly different from zero at the alpha = 0.05 level.
- b Indicates that the AAPC is significantly different from zero at the alpha = 0.05 level.
During the same study period, notable variations in cancer incidence trends were observed among China, the US, and the UK (Table 2). For lung cancer, the ASIRs were lower for women than for men in all three countries. In 1990, the ASIR for lung cancer in men was higher in the US and the UK than in China, but it rapidly declined throughout the study period, eventually falling far below the ASIR in China. For women, although the US initially had the highest lung cancer ASIR and experienced a significant increase from 1990 to 2000, it has since been on a downward trend, reaching 32.5 per 100,000 population in 2021. However, the ASIR for lung cancer in Chinese women saw significant increases during 1990-2005 and 2015-2021. Similarly, the ASIR for breast cancer and prostate cancer in the US was the highest, but after a brief increase between 1990 and 1994/1995, it began to decline sharply. In contrast, the ASIR for these cancers in China was initially much lower but then rose significantly. For colorectal cancer, the ASIR for both men and women in the US began to decrease rapidly from 2002 and 2001, respectively, while in China, it maintained a rapid upward trend throughout the whole study period. However, although the ASIRs for colorectal cancer in men and women of the UK experienced brief increases (2004-2007 for men in the UK and 2002-2019 for women in the UK), it showed a significant decline for most of the time during the study period. It's important to note that the ASIRs for liver cancer in China showed an overall downward trend during the entire study period. Although the ASIR for liver cancer in Chinese men experienced slight increases between 1990-2001 and 2004-2021, there was a sharp decline from 2001 to 2004. For Chinese women, the ASIR for liver cancer generally decreased, with the exception of a slight increase between 2008 and 2016, whereas in the US and UK, these rates of both sexes remained significantly increased throughout the study period. The overall ASIR of stomach cancer exhibited a downward trend in all three countries, particularly in China. As for esophageal cancer, the ASIR showed an overall decline in China, while it remained relatively stable in the US and the UK. Conversely, the ASIR for cervical cancer in China showed a downward trend before 1999, but then rose from 10.4 per 100,000 population in 1999 to 13.4 per 100,000 in 2021, while a sharp decline in cervical cancer ASIR was observed in both the US and the UK during the same period (dropping from 16.7 to 12.6 per 100,000 population in US, while dropping from 16.4 to 10.3 per 100,000 population in UK).
| Country | Sex | ASIR (per 100,000 population) | Trends 1 | Trends 2 | Trends 3 | 1990-2021, AAPC (95%CI) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1990 | 2021 | Years | APC (95%CI) | Years | APC (95%CI) | Years | APC (95%CI) | |||
| Tracheal, bronchus, and lung cancer | ||||||||||
| China | Male | 48.5 | 62.6 | 1990-1997 | 0.6 (−0.3 to 1.5) | 1997-2005 | 2.8a (2.0 to 3.6) | 2005-2021 | 0.1 (−0.1 to 0.3) | 0.9b (0.6 to 1.2) |
| Female | 20.0 | 28.2 | 1990-2005 | 1.6a (1.5 to 1.7) | 2005-2015 | −0.1 (−0.4 to 0.1) | 2015-2021 | 2.3a (2.0 to 2.7) | 1.2b (1.1 to 1.3) | |
| US | Male | 87.1 | 43.1 | 1990-1995 | −0.5 (−1.1 to 0.1) | 1995-2008 | −1.9a (−2.1 to −1.7) | 2008-2021 | −3.6a (−3.8 to −3.3) | −2.4b (−2.5 to −2.2) |
| Female | 39.6 | 32.5 | 1990-2000 | 1.5a (1.2 to 1.8) | 2000-2009 | −0.6a (−1.0 to −0.3) | 2009-2021 | −2.8a (−3.0 to −2.5) | −0.8b (−1.0 to −0.6) | |
| UK | Male | 81.1 | 40.1 | 1990-2002 | −2.8a (−2.9 to −2.6) | 2002-2013 | −1.4a (−1.6 to −1.1) | 2013-2021 | −2.8a (−3.3 to −2.4) | −2.3b (−2.4 to −2.1) |
| Female | 29.9 | 31.5 | 1990-2002 | 0.5a (0.2 to 0.8) | 2002-2013 | 1.3a (0.9 to 1.6) | 2013-2021 | −1.9a (−2.4 to −1.4) | 0.2 (0 to 0.4) | |
| Breast cancer | ||||||||||
| China | Male | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Female | 17.8 | 37.0 | 1990-2011 | 2.5a (2.4 to 2.6) | 2011-2015 | 0.5 (−1.1 to 2.2) | 2015-2021 | 3.6a (3.1 to 4.1) | 2.5b (2.2 to 2.7) | |
| US | Male | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Female | 124.3 | 97.0 | 1990-1995 | 0.6a (0.1 to 1.2) | 1995-2003 | −0.7a (−1.1 to −0.4) | 2003-2021 | −1.3a (−1.4 to −1.2) | −0.8b (−1.0 to −0.7) | |
| UK | Male | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Female | 103.9 | 83.7 | 1990-1994 | 0.8 (−0.4 to 2.0) | 1994-2009 | −0.3a (−0.5 to −0.1) | 2009-2021 | −1.5a (−1.8 to −1.3) | −0.6b (−0.8 to −0.4) | |
| Colorectal cancer | ||||||||||
| China | Male | 22.3 | 42.2 | 1990-1998 | 0.6a (0.2 to 1.0) | 1998-2011 | 2.9a (2.8 to 3.1) | 2011-2021 | 2.1a (1.9 to 2.3) | 2.1b (1.9 to 2.2) |
| Female | 16.4 | 21.9 | 1990-1998 | 0.1 (−0.3 to 0.5) | 1998-2016 | 0.8a (0.7 to 0.9) | 2016-2021 | 2.9a (2.3 to 3.5) | 1.0b (0.8 to 1.1) | |
| US | Male | 57.5 | 44.9 | 1990-2002 | 0.1 (−0.1 to 0.2) | 2002-2005 | −3.0a (−5.5 to −0.5) | 2005-2021 | −1.1a (−1.3 to −1.0) | −0.9b (−1.1 to −0.6) |
| Female | 39.9 | 32.2 | 1990-2001 | 0.5a (0.4 to 0.7) | 2001-2005 | −2.4a (−3.5 to −1.2) | 2005-2021 | −1.2a (−1.3 to −1.1) | −0.7b (−0.9 to −0.6) | |
| UK | Male | 52.1 | 45.5 | 1990-2004 | −0.3a (−0.5 to −0.2) | 2004-2007 | 1.2 (−2.3 to 4.9) | 2007-2021 | −0.9a (−1.1 to −0.8) | −0.4b (−0.8 to −0.1) |
| Female | 36.4 | 32.8 | 1990-2002 | −0.7a (−0.9 to −0.5) | 2002-2019 | 0.1 (0 to 0.3) | 2019-2021 | −2.9 (−6.7 to 1.1) | −0.4b (−0.7 to −0.1) | |
| Liver cancer | ||||||||||
| China | Male | 15.1 | 14.3 | 1990-2001 | 1.1a (0.6 to 1.5) | 2001-2004 | −3.9 (−10.1 to 2.8) | 2004−2021 | 0.2 (0 to 0.5) | 0.1 (−0.5 to 0.8) |
| Female | 6.0 | 4.9 | 1990-2008 | −1.1a (−1.3 to −0.9) | 2008-2016 | 0.9 (0 to 1.9) | 2016-2021 | −2.1a (−3.6 to −0.5) | −0.7b (−1.1 to −0.4) | |
| US | Male | 3.5 | 8.3 | 1990-1998 | 4.5a (4.3 to 4.7) | 1998-2010 | 3.2a (3.1 to 3.3) | 2010-2021 | 1.1a (1.0 to 1.1) | 2.8b (2.7 to 2.8) |
| Female | 1.5 | 3.2 | 1990-1998 | 4.0a (3.5 to 4.5) | 1998-2017 | 2.2a (2.2 to 2.3) | 2017-2021 | 0.8a (0.1 to 1.5) | 2.5b (2.4 to 2.7) | |
| UK | Male | 2.8 | 8.8 | 1990-1995 | 0.2 (−1.6 to 2.0) | 1995-2014 | 5.7a (5.6 to 5.9) | 2014-2021 | 1.4a (1.0 to 1.7) | 3.8b (3.5 to 4.1) |
| Female | 1.4 | 4.3 | 1990-1995 | 0.6 (−0.5 to 1.7) | 1995-2015 | 5.1a (5.0 to 5.2) | 2015-2021 | 1.4a (1.1 to 1.7) | 3.7b (3.5 to 3.9) | |
| Cervical cancer | ||||||||||
| China | Male | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Female | 11.8 | 13.4 | 1990-1999 | −1.6a (−1.9 to −1.2) | 1999-2004 | 4.0a (2.8 to 5.3) | 2004-2021 | 0.6a (0.5 to 0.7) | 0.5b (0.3 to 0.7) | |
| US | Male | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Female | 20.5 | 12.6 | 1990-1996 | −1.5a (−2.2 to −0.7) | 1996-2004 | −3.4a (−4.1 to −2.7) | 2004-2021 | −0.4a (−0.6 to −0.2) | −1.4b (−1.6 to −1.1) | |
| UK | Male | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Female | 30.4 | 10.3 | 1990-1999 | −6.8a (−7.1 to −6.4) | 1999-2005 | −3.1a (−4.5 to −1.7) | 2005-2021 | −1.7a (−2.0 to −1.4) | −3.5b (−3.8 to −3.2) | |
| Stomach cancer | ||||||||||
| China | Male | 67.6 | 44.5 | 1990-1998 | −1.6a (−2.0 to −1.3) | 1998-2004 | 1.1a (0.3 to 1.9) | 2004-2021 | −2.3a (−2.4 to −2.1) | −1.4b (−1.6 to −1.3) |
| Female | 30.2 | 15.2 | 1990-2005 | −1.5a (−1.7 to −1.2) | 2005-2014 | −4.3a (−5.0 to −3.5) | 2014-2021 | −0.7 (−1.9 to 0.5) | −2.1b (−2.5 to −1.8) | |
| US | Male | 11.7 | 6.8 | 1990-1999 | −1.4a (−1.6 to −1.2) | 1999-2006 | −2.5a (−2.9 to −2.0) | 2006-2021 | −1.7a (−1.8 to −1.6) | −1.8b (−1.9 to −1.7) |
| Female | 5.3 | 3.6 | 1990-2001 | −0.7a (−0.9 to −0.6) | 2001-2007 | −2.3a (−2.8 to −1.7) | 2007-2021 | −1.2a (−1.3 to −1.1) | −1.2b (−1.4 to −1.1) | |
| UK | Male | 21.6 | 8.2 | 1990-1998 | −2.8a (−3.0 to −2.6) | 1998-2005 | −3.9a (−4.3 to −3.5) | 2005-2021 | −2.8a (−3.0 to −2.7) | −3.1b (−3.2 to −2.9) |
| Female | 9.1 | 4.0 | 1990-1999 | −2.6a (−2.8 to −2.4) | 1999-2009 | −3.3a (−3.5 to −3.0) | 2009-2021 | −1.9a (−2.1 to −1.6) | −2.5b (−2.7 to −2.4) | |
| Prostate cancer | ||||||||||
| China | Male | 5.0 | 9.3 | 1990-1999 | 3.2a (2.7 to 3.6) | 1999-2014 | 1.3a (1.1 to 1.5) | 2014-2021 | 2.3a (1.9 to 2.8) | 2.1b (1.9 to 2.3) |
| Female | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | |
| US | Male | 135.4 | 108.0 | 1990-1994 | 2.4a (1.6 to 3.2) | 1994-2013 | −1.6a (−1.7 to −1.5) | 2013-2021 | −0.3 (−0.7 to 0) | −0.8b (−0.9 to −0.6) |
| Female | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | |
| UK | Male | 61.1 | 76.1 | 1990-2006 | 1.9a (1.7 to 2.1) | 2006-2016 | −0.3 (−0.7 to 0) | 2016-2021 | −1.9a (−2.8 to −1.0) | 0.6b (0.4 to 0.8) |
| Female | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | |
| Esophageal cancer | ||||||||||
| China | Male | 36.1 | 24.8 | 1990-2005 | −0.3a (−0.6 to −0.1) | 2005-2016 | −2.9a (−3.4 to −2.3) | 2016-2021 | 0.4 (−1.4 to 2.4) | −1.1b (−1.5 to −0.7) |
| Female | 14.4 | 6.4 | 1990-2004 | −1.2a (−1.3 to −1.1) | 2004-2015 | −5.5a (−5.8 to −5.3) | 2015-2021 | −0.1 (−1.0 to 0.8) | −2.6b (−2.7 to −2.4) | |
| US | Male | 7.0 | 7.1 | 1990-2001 | 1.3a (1.1 to 1.5) | 2001-2006 | 0 (−0.9 to 0.9) | 2006-2021 | −0.9a (−1.1 to −0.8) | 0 (−0.2 to 0.2) |
| Female | 1.9 | 1.7 | 1990-2001 | 0.7a (0.6 to 0.9) | 2001-2008 | −1.3a (−1.7 to −1.0) | 2008-2021 | −0.9a (−1.0 to −0.7) | −0.4b (−0.5 to −0.3) | |
| UK | Male | 10.5 | 11.0 | 1990-1994 | 3.3a (1.9 to 4.7) | 1994-2006 | 0.8a (0.6 to 1.1) | 2006-2021 | −1.0a (−1.2 to −0.8) | 0.3b (0 to 0.5) |
| Female | 4.8 | 4.4 | 1990-1995 | 2.1a (1.3 to 2.9) | 1995-2002 | 0.1 (−0.5 to 0.6) | 2002-2021 | −0.9a (−1.0 to −0.8) | −0.2b (−0.4 to 0) | |
- Abbreviations: AAPC, average annual percent change; APC, annual percent change; ASIR, age-standardized incidence rate; CI, confidence interval; N/A, not applicable; UK, United Kingdom; US, United States.
- a Indicates that the APC is significantly different from zero at the alpha = 0.05 level.
- b Indicates that the AAPC is significantly different from zero at the alpha = 0.05 level.
As summarized in Table 3, the ASMR trends of lung, liver, stomach, and esophageal cancers for all three countries were generally consistent with their ASIR trends. In breast cancer, the ASMR in the US and the UK sharply declined throughout the study period, while the ASMR in China did not change significantly. A similar pattern was also observed in prostate cancer. Unlike the steadily decreasing ASMR of colorectal cancer in the US and the UK, the ASMR for colorectal cancer in Chinese men remained largely unchanged overall. However, in Chinese women, the ASMR gradually increased after a slow decline from 1990 to 2014. Regarding cervical cancer, the ASMR in the US and the UK generally followed a downward trend throughout the study period, whereas, the ASMR in China first sharply declined between 1990 and 1999, then sharply increased until 2003, after which it began to decrease significantly again.
| Country | Sex | ASMR (per 100,000 population) | Trends 1 | Trends 2 | Trends 3 | 1990-2021, AAPC (95%CI) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1990 | 2021 | Years | APC (95%CI) | Years | APC (95%CI) | Years | APC (95%CI) | |||
| Tracheal, bronchus, and lung cancer | ||||||||||
| China | Male | 51.4 | 56.5 | 1990-1997 | 0.4 (−0.4 to 1.2) | 1997-2004 | 2.7a (1.8 to 3.6) | 2004-2021 | −0.6a (−0.8 to −0.4) | 0.4b (0.1 to 0.6) |
| Female | 20.9 | 24.4 | 1990-2004 | 1.2a (1.1 to 1.4) | 2004-2015 | −1.0a (−1.2 to −0.8) | 2015-2021 | 1.7a (1.3 to 2.2) | 0.5b (0.4 to 0.7) | |
| US | Male | 74.8 | 34.8 | 1990-1995 | −1.2a (−1.6 to −0.7) | 1995-2007 | −2.1a (−2.3 to −1.9) | 2007-2021 | −3.5a (−3.6 to −3.3) | −2.6b (−2.7 to −2.4) |
| Female | 31.7 | 24.2 | 1990-2001 | 0.8a (0.6 to 1.0) | 2001-2009 | −1.0a (−1.5 to −0.6) | 2009-2021 | −2.7a (−2.9 to −2.4) | −1.0b (−1.2 to −0.9) | |
| UK | Male | 75.9 | 33.0 | 1990-2005 | −3.2a (−3.2 to −3.1) | 2005-2008 | −0.9 (−3.6 to 1.8) | 2008-2021 | −2.5a (−2.6 to −2.3) | −2.7b (−2.9 to −2.4) |
| Female | 26.7 | 24.5 | 1990-2002 | 0 (−0.2 to 0.3) | 2002-2014 | 0.3a (0.1 to 0.6) | 2014-2021 | −1.9a (−2.4 to −1.4) | −0.3b (−0.5 to −0.1) | |
| Breast cancer | ||||||||||
| China | Male | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Female | 9.0 | 8.2 | 1990-2001 | 0.4a (0.2 to 0.5) | 2001-2015 | −1.4a (−1.5 to −1.3) | 2015-2021 | 1.2a (0.7 to 1.6) | −0.3b (−0.4 to −0.2) | |
| US | Male | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Female | 28.2 | 17.2 | 1990-1994 | −1.3a (−2.0 to −0.7) | 1994-2010 | −2.0a (−2.1 to −1.9) | 2010-2021 | −1.2a (−1.4 to −1.0) | −1.6b (−1.7 to −1.5) | |
| UK | Male | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Female | 36.3 | 19.5 | 1990-1994 | −1.1a (−1.7 to −0.5) | 1994-2010 | −2.5a (−2.6 to −2.4) | 2010-2021 | −1.5a (−1.7 to −1.3) | −1.9b (−2.1 to −1.8) | |
| Colorectal cancer | ||||||||||
| China | Male | 18.6 | 18.9 | 1990-1998 | −0.4 (−0.8 to 0.1) | 1998-2003 | 0.9 (−0.3 to 2.1) | 2003-2021 | −0.1 (−0.2 to 0.1) | 0 (−0.2 to 0.2) |
| Female | 13.2 | 9.3 | 1990-2004 | −1.1a (−1.2 to −1.0) | 2004-2014 | −2.2a (−2.5 to −2.0) | 2014-2021 | 0.5a (0.1 to 0.9) | −1.1b (−1.2 to −1.0) | |
| US | Male | 25.3 | 15.2 | 1990-2001 | −1.4a (−1.5 to −1.2) | 2001-2010 | −2.5a (−2.8 to −2.1) | 2010-2021 | −1.4a (−1.6 to −1.1) | −1.7b (−1.8 to −1.6) |
| Female | 17.3 | 10.7 | 1990-2001 | −1.0a (−1.2 to −0.9) | 2001-2010 | −2.5a (−2.7 to −2.2) | 2010-2021 | −1.3a (−1.6 to −1.1) | −1.6b (−1.7 to −1.5) | |
| UK | Male | 30.1 | 18.7 | 1990-2014 | −1.8a (−1.8 to −1.7) | 2014-2018 | 0.1 (−1.4 to 1.6) | 2018-2021 | −2.4a (−3.9 to −0.8) | −1.6b (−1.8 to −1.4) |
| Female | 20.6 | 13.2 | 1990-2010 | −2.0a (−2.1 to −2.0) | 2010-2019 | 0.2 (−0.1 to 0.5) | 2019-2021 | −2.9 (−5.9 to 0.2) | −1.5b (−1.7 to −1.2) | |
| Liver cancer | ||||||||||
| China | Male | 15.2 | 12.4 | 1990-2001 | 0.9a (0.5 to 1.4) | 2001-2005 | −3.4a (−6.6 to −0.2) | 2005-2021 | −0.5a (−0.8 to −0.2) | −0.4 (−0.8 to 0.1) |
| Female | 6.3 | 4.6 | 1990-2001 | −0.5a (−1.0 to 0) | 2001-2005 | −3.3 (−7.2 to 0.7) | 2005-2021 | −0.2 (−0.6 to 0.1) | −0.7b (−1.3 to −0.2) | |
| US | Male | 2.9 | 6.1 | 1990-2001 | 3.4a (3.0 to 3.7) | 2001-2016 | 2.3a (2.1 to 2.4) | 2016-2021 | 0.5 (−0.2 to 1.2) | 2.4b (2.2 to 2.6) |
| Female | 1.3 | 2.6 | 1990-1999 | 3.0a (2.3 to 3.7) | 1999-2018 | 2.1a (1.9 to 2.2) | 2018-2021 | 0.4 (−1.6 to 2.6) | 2.2b (1.9 to 2.5) | |
| UK | Male | 2.6 | 6.9 | 1990-1994 | −2.8 (−5.5 to 0) | 1994-2015 | 4.9a (4.7 to 5.1) | 2015-2021 | 1.0a (0.5 to 1.6) | 3.1b (2.7 to 3.5) |
| Female | 1.4 | 3.9 | 1990-1995 | −0.6 (−2.5 to 1.3) | 1995-2016 | 4.7a (4.6 to 4.9) | 2016-2021 | 1.2a (0.5 to 1.9) | 3.3b (2.9 to 3.6) | |
| Cervical cancer | ||||||||||
| China | Male | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Female | 7.0 | 4.6 | 1990-1999 | −2.8a (−3.3 to −2.2) | 1999-2003 | 2.1 (−1.4 to 5.8) | 2003-2021 | −1.3a (−1.6 to −1.1) | −1.3b (−1.8 to −0.8) | |
| US | Male | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Female | 3.8 | 2.7 | 1990-2006 | −1.5a (−1.6 to −1.4) | 2006-2015 | 0 (−0.4 to 0.3) | 2015-2021 | −2.0a (−2.6 to −1.4) | −1.2b (−1.3 to −1.0) | |
| UK | Male | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Female | 6.0 | 2.2 | 1990-1995 | −7.6a (−8.6 to −6.6) | 1995-2008 | −2.9a (−3.4 to −2.5) | 2008-2021 | −1.8a (−2.3 to −1.2) | −3.2b (−3.5 to −2.9) | |
| Stomach cancer | ||||||||||
| China | Male | 64.7 | 32.6 | 1990-1998 | −2.2a (−2.6 to −1.7) | 1998-2003 | 1.0 (−0.4 to 2.5) | 2003-2021 | −3.3a (−3.5 to −3.1) | −2.3b (−2.6 to −2.1) |
| Female | 29.8 | 12.0 | 1990-2004 | −1.8a (−2.0 to −1.6) | 2004-2014 | −5.2a (−5.8 to −4.5) | 2014-2021 | −1.4a (−2.7 to −0.1) | −2.8b (−3.2 to −2.5) | |
| US | Male | 7.8 | 3.8 | 1990-1994 | −2.1a (−2.7 to −1.5) | 1994-2010 | −2.8a (−2.9 to −2.7) | 2010-2021 | −1.7a (−2.0 to −1.5) | −2.3b (−2.5 to −2.2) |
| Female | 8.2 | 3.4 | 1990-2002 | −1.7a (−1.8 to −1.6) | 2002-2008 | −2.9a (−3.5 to −2.3) | 2008-2021 | −1.4a (−1.6 to −1.2) | −1.8b (−1.9 to −1.7) | |
| UK | Male | 18.0 | 6.1 | 1990-1999 | −3.2a (−3.4 to −3.1) | 1999-2006 | −4.5a (−4.9 to −4.2) | 2006-2021 | −3.0a (−3.1 to −2.8) | −3.4b (−3.5 to −3.3) |
| Female | 3.6 | 2.1 | 1990-1999 | −2.9a (−3.1 to −2.7) | 1999-2009 | −3.8a (−4.0 to −3.5) | 2009-2021 | −1.8a (−2.1 to −1.6) | −2.8b (−2.9 to −2.6) | |
| Prostate cancer | ||||||||||
| China | Male | 4.8 | 4.9 | 1990-2000 | 2.0a (1.5 to 2.5) | 2000-2010 | −1.9a (−2.5 to −1.3) | 2010-2021 | 0.1 (−0.3 to 0.6) | 0.1 (−0.2 to 0.3) |
| Female | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | |
| US | Male | 29.4 | 16.5 | 1990-1993 | 1.2a (0.2 to 2.1) | 1993-2012 | −2.9a (−3.0 to −2.8) | 2012-2021 | −0.7a (−1.0 to −0.4) | −1.9b (−2.0 to −1.8) |
| Female | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | |
| UK | Male | 30.7 | 22.8 | 1990-1995 | 0.8 (−0.1 to 1.7) | 1995-2010 | −1.6a (−1.8 to −1.4) | 2010-2021 | −0.6a (−1.0 to −0.3) | −0.9b (−1.1 to −0.7) |
| Female | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | |
| Esophageal cancer | ||||||||||
| China | Male | 38.2 | 23.8 | 1990-2004 | −0.3 (−0.5 to 0) | 2004-2016 | −3.2a (−3.7 to −2.7) | 2016-2021 | −0.2 (−2.2 to 1.8) | −1.4b (−1.8 to −1.0) |
| Female | 15.3 | 5.8 | 1990-2004 | −1.4a (−1.6 to −1.3) | 2004-2014 | −6.4a (−6.7 to −6.0) | 2014-2021 | −1.5a (−2.3 to −0.7) | −3.1b (−3.3 to −2.9) | |
| US | Male | 6.6 | 6.4 | 1990-2002 | 0.9a (0.7 to 1.1) | 2002-2006 | −0.4 (−1.8 to 1.1) | 2006-2021 | −0.9a (−1.1 to −0.8) | −0.2 (−0.4 to 0) |
| Female | 1.6 | 1.3 | 1990-2002 | 0.1 (0 to 0.2) | 2002-2008 | −1.9a (−2.3 to −1.5) | 2008-2021 | −1.0a (−1.1 to −0.8) | −0.7b (−0.8 to −0.6) | |
| UK | Male | 10.7 | 10.6 | 1990-1994 | 3.0a (1.7 to 4.2) | 1994-2004 | 0.7a (0.4 to 1.0) | 2004-2021 | −1.0a (−1.1 to −0.9) | 0.1 (−0.1 to 0.2) |
| Female | 4.7 | 4.1 | 1990-1999 | 1.1a (0.7 to 1.4) | 1999-2011 | −1.4a (−1.6 to −1.1) | 2011-2021 | −0.7a (−1.0 to −0.3) | −0.4b (−0.6 to −0.3) | |
- Abbreviations: AAPC, average annual percent change; APC, annual percent change; ASMR, age-standardized mortality rate; CI, confidence interval; N/A, not applicable; UK, United Kingdom; US, United States.
- a Indicates that the APC is significantly different from zero at the alpha = 0.05 level.
- b Indicates that the AAPC is significantly different from zero at the alpha = 0.05 level.
3.3 Cancer burden in China, the US, and the UK
In 2021, the GBD study estimated that cancers were responsible for 71,037,170 DALYs in China (Supplementary Table S3). The highest cancer-related DALY burden in China was attributed to lung cancer, accounting for 18,920,203 DALYs (26.6% of all cancer-related DALYs), followed by stomach cancer (10,642,127 DALYs; 15.0%), esophageal cancer (6,898,666 DALYs; 9.7%), colorectal cancer (6,848,390 DALYs; 9.6%), and liver cancer (4,890,023 DALYs; 6.9%). Together, these five cancers contributed to over 67% of the total cancer DALY burden in China.
Figure 2 highlights that leukemia and cancers of the brain and central nervous system were the leading causes of cancer burden among children and adolescents under 20 years of age in China. For young adults (20-44 years) and middle-aged men (45-59 years) in China, liver, lung, and stomach cancers were the most significant contributors, with lung and stomach cancers remaining predominant in older men (60 years and above). In young and middle-aged Chinese women, lung, breast, stomach, and cervical cancers were the top contributors to cancer burden, whereas lung, stomach, colorectal, and breast cancers were the most burdensome in older women.
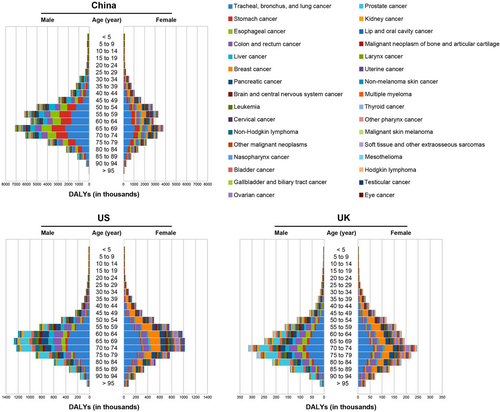
The cancer burden varied significantly between China, the US, and the UK in 2021. China exhibited a higher age-standardized DALY rate for all cancers compared to the US and UK, with rates of 3459.8, 2932.2, and 3075.3 per 100,000 population, respectively (Supplementary Table S3). In China, the populations bearing the highest cancer burden were generally younger than those in the UK (Figure 2). Lung cancer was the leading cause of cancer burden in all three countries (Supplementary Table S3). Besides lung cancer, the top cancer burden contributors for China included digestive cancers—specifically stomach, esophageal, colorectal, and liver cancers—whereas in the US and UK, colorectal, breast, pancreatic, and prostate cancers were more prominent (Supplementary Table S3). Regarding the age distribution of DALY, leukemia and cancers of brain and central nervous system were the top contributors among children and adolescents in all three countries (Figure 2). For young men, liver and lung cancers led to the highest DALY in China, while in the US and UK, colorectal cancer and brain and central nervous system cancers were more significant (Figure 2). In young women, breast and cervical cancers were the leading cause of DALY in the US and UK, but breast and lung cancers were predominant in China (Figure 2). For middle-aged men, the top cancer burden contributors were lung and colorectal cancers in the US and UK, but those in China were lung and stomach cancers (Figure 2). In middle-aged women, lung and breast cancers were the leading cause of DALY in all three countries (Figure 2). Among the elderly, lung cancer remained the most significant contributor to the DALY burden across all three countries (Figure 2).
3.4 Shifts of cancer burden in China, the US, and the UK
From 1990 to 2021, China saw a 32.7% reduction in its age-standardized DALY rate, dropping from 5141.9 (95% uncertainty interval [UI] = 4517.0-5783.8) per 100,000 population in 1990 to 3459.8 (95% UI = 2902.3-4122.9) per 100,000 in 2021. This decline was more pronounced in females (38.1%) than in males (28.8%). Figure 3 outlines the shifts in all-age DALY rates for 32 different cancer types in China. By 2021, lung cancer had become the leading contributor to the DALY burden, overtaking stomach cancer, which held that position in 1990. Colorectal cancer, liver cancer, breast cancer, cervical cancer, and prostate cancer rose in the rankings, becoming the fourth, fifth, sixth, tenth, and seventeenth leading causes of DALY burden, respectively. In contrast, the burden of stomach cancer declined. It fell by 18.3%, leading to a drop in its rankings—from first to second. Meanwhile, the rankings for esophageal cancer remained stable, despite a 51.4% decrease in its age-standardized DALY rate, respectively, over the same period.
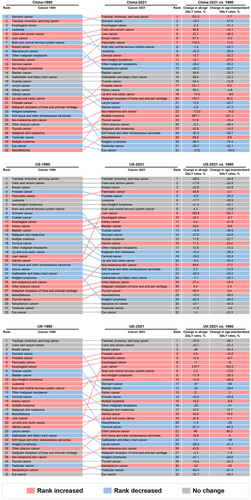
The trends in the cancer burden of the US and the UK during this period differed notably from those in China (Figure 3). While lung, colorectal, and breast cancers remained the top 3 cancers contributing to the DALY burden in both countries, their all-age and age-standardized DALY rates saw substantial declines over the past 31 years. The most significant change was observed in liver cancer, with all-age DALY rates increasing by 183.8% in the US and 215.7% in the UK, resulting in its ranking rising from nineteenth to ninth in the US and from nineteenth to seventh in the UK. Additionally, the age-standardized DALY rate for cervical cancer dropped sharply, particularly in the UK, where it fell by 61.3% between 1990 and 2021, causing it to drop out of the top 20 causes of DALY burden by 2021, down from fourteenth in 1990.
4 DISCUSSION
In this study, we carried out a thorough epidemiological assessment of cancer incidence, mortality, and DALYs in China, drawing on the latest data from GLOBOCAN 2022 and GBD 2021. We also examined the temporal trends over the past 31 years in these metrics and compared them between China, the US, and the UK using high-quality data from the GHDx database. Our results indicated that China exhibits a lower cancer incidence rate compared to the US and the UK. Although cancer-related mortality in China is slightly lower than that in the UK, it is significantly higher than that in the US. Additionally, China faces much higher DALY rates compared to both the US and the UK. A significant portion of cancer-related mortality and DALYs in China are attributed to digestive cancers, including colorectal, stomach, liver, and esophageal cancers. Moreover, the cancer landscape of China is shifting from that of a developing country to one more reflective of a developed country, with a rapid rise in the incidence and burden of lung, colorectal, breast, cervical, and prostate cancers. Meanwhile, the incidence and burden of stomach cancer continued to decline. Although the incidence of liver and esophageal cancers was decreasing, the burden of liver cancer was increasing, while the burden of esophageal cancer remained largely unchanged.
GLOBOCAN 2022 estimates indicated that 24.2% of all new cancer diagnoses globally occurred in China, whereas China accounted for 26.4% of worldwide cancer deaths. The ASIR for all cancers in China was lower than that in the US and UK, while ASMR for all cancers in China was slightly lower than that in the UK, it is considerably higher than that in the US. Moreover, China's DALY rates were significantly higher than those observed in both the US and UK. Several factors explain this discrepancy. First, the higher mortality rate in China could be attributed to variations in cancer patterns across different countries. Besides lung, breast, and colorectal cancers, stomach, liver, and esophageal cancers—known for their poor prognosis and substantial DALY burden—are the most prevalent in China [19]. However, the most common cancers in the US and UK, such as prostate cancer, uterine tumors, and skin melanoma, generally have lower mortality rates [20]. Second, there is a lack of awareness about early cancer screening in China, leading to lower rates of early detection, which adversely affects prognosis and DALY burden. Despite higher cancer incidence in the US and the UK, early detection is more common, resulting in better outcomes [21, 22]. Third, healthcare availability and access vary widely across China [23], contributing to the situation. Lastly, China has been slower to adopt new anti-cancer drugs and treatments [24].
Based on the data from the GHDx database, the trend analysis revealed that the ASMR for both sexes in China, the US, and the UK significantly declined over the study period, except for Chinese men, who saw a notable increase between 1997 and 2003. The ASIR trends for all cancers in the US and the UK differ significantly from those in China. Both men and women in the US saw a slight increase in ASIR from 1990 to 2000, followed by a sharp rise between 2000 and 2004/2005, and then a steady decline from 2004/2005 to 2021. For men in the UK, the ASIR stayed consistent until 2016, while for women, it remained steady until 2014. After these years, both sexes in the UK experienced a notable decline through 2021. However, the ASIR for all cancers in Chinese men increased between 1990 and 2011, followed by a period of stabilization until 2019 and a significant increase from 2019 to 2021, while the ASIR for all cancers in Chinese women showed an upward trend until 2008, followed by a slight decrease until 2016, and then a notable rise between 2016 and 2021. These findings highlighted the significant differences in cancer prevention and management between China and the US or the UK. As a result, it has become increasingly important for China to learn from the effective practices used in cancer prevention and management in the US and the UK.
One of the most effective strategies employed by the US and the UK in cancer prevention is the implementation of population-based screening programs, which has significantly reduced mortality and the DALY burden for certain cancer types. For instance, the UK introduced national screening for breast and cervical cancers in the 1980s, contributing to a decline in ASMR for breast cancer from 28.9 per 100,000 population to 15.9 per 100,000 population between 1990 and 2013, and for cervical cancer from 4.8 per 100,000 population to 1.6 per 100,000 population during the same period [25]. Similarly, since the UK began colorectal cancer screening in 2006, the ASMR for colorectal cancer dropped from 14.4 per 100,000 population to 12.7 per 100,000 population in men and from 9.0 per 100,000 population to 8.3 per 100,000 population in women within 7 years [26]. The success of these screening programs largely depends on population coverage and adherence. In the US, where the ASMR for cervical, breast, and colorectal cancers have decreased significantly, adherence rates for these screenings were approximately 81%, 72%, and 63%, respectively [27]. In contrast, China has not yet implemented national screening for cancers other than breast and cervical cancer, although since 2006, the government has targeted high-risk populations for screening of breast, colorectal, lung, stomach, esophageal, and nasopharyngeal cancers. The increasing awareness of early cancer screening in Chinese urban areas may partly explain the reduction in stomach and esophageal cancer mortality. However, the challenge in China remains the insufficient coverage of screening across the entire country, which needs further improvement.
Smoking is a major global risk factor for cancer, linked to about 20 types of malignancies and responsible for over 70% of lung cancer cases worldwide [28, 29]. Therefore, enforcing strict tobacco control policies is an effective strategy to lower cancer ASIR and ASMR. To curb global cigarette consumption, the World Health Organization (WHO) introduced the “Framework Convention on Tobacco Control” in 2003, which was signed by 168 countries, each developing its own tobacco control measures. The US, a pioneer in anti-tobacco efforts, began implementing stringent tobacco control policies as early as the 1960s. Since then, smoking rates in the US have dropped from 41.9% in 1965 to 12.7% in 2020 [30, 31], and lung cancer mortality in US males decreased by 43% between 1990 and 2014 [32, 33]. The UK has also made significant strides in tobacco control, reducing its smoking rate from 50% in the 1970s to 15% in 2016 [34]. Between 1995 and 2013, the UK saw a continuous decline in lung cancer incidence and mortality, with reductions of over 25% and 35%, respectively (AACR Cancer progress report. org. 2023. http://www.cancerprogressreport.org/.). Despite China ratifying the Framework Convention on Tobacco Control in 2005 and adopting a national tobacco control law in 2006, its tobacco control efforts remain inadequate. The China Tobacco Control Report revealed that the smoking rate among Chinese men exceeded 50% [35, 36], resulting in a higher incidence of lung cancer compared to the US and UK. Although the smoking rate among Chinese women is relatively lower than that in the US and the UK [37], the incidence of lung cancer in Chinese women has rapidly increased and is poised to surpass that of the US and UK. However, more than half of lung cancer cases in Chinese women cannot be linked to known risk factors [38]. Large-scale studies are essential to uncover additional risk factors for lung cancer in Chinese women.
Preventing chronic infections is considered the most effective way to reduce the risk of cancers linked to infections, such as liver, cervical, stomach, and nasopharyngeal cancers [39]. Helicobacter pylori (H. pylori) infection is the leading risk factor for stomach cancer [40]. In China, the prevalence of H. pylori is approximately 20% higher than in the US and UK, which may partly explain the higher rates of stomach cancer in China [41]. However, stomach cancer incidence among Chinese men has dropped annually from 1990 to 1998, and from 2004 to 2021. A similar decline was seen in Chinese women, with a decrease between 1990 and 2021. These reductions are likely due to a lower prevalence of H. pylori, driven by increased awareness and treatment of the infection [42, 43]. Liver cancer, another infection-related cancer, has also seen declining rates in China, possibly due to the introduction of routine hepatitis B virus (HBV) vaccination for infants in 1992 [44]. However, hepatitis C virus (HCV) infection accounts for the majority of the increase in liver cancer cases in US and UK, while the incidence of liver cancer associated with alcoholic cirrhosis and HBV infection has remained stable [45, 46]. Human papillomavirus (HPV) is responsible for 99.7% of cervical cancer cases globally [47, 48]. In the US, HPV vaccination began in 2006, leading to a significant drop in the prevalence of HPV, followed by a decrease in cervical cancer incidence [49, 50]. Since 2017, China has gradually approved the bivalent, quadrivalent, and nine-valent HPV vaccines. However, these vaccines have not yet been incorporated into the national immunization program. Nasopharyngeal cancer, although rare globally, is prevalent in southern China and is closely linked to Epstein-Barr virus (EBV) infection [51]. Unfortunately, there is still no vaccine available to reduce the risk of this cancer by preventing EBV infection [52].
Besides the previously mentioned measures, promoting awareness of healthy lifestyles through education is also an effective cancer prevention strategy. Unhealthy habits, such as rising obesity rates, high red meat consumption, and sedentary behavior, contribute to the increasing incidence of lung, breast, colorectal, and prostate cancers [53, 54]. As China experiences a shift towards these unhealthy lifestyles, the rates of these cancers are also on the rise. Additionally, malnutrition and intake of nitrosamine-contaminated food may play a significant role in the high incidence of upper gastrointestinal cancers in China [5, 53]. Between 1990 and 2021, the overall incidence of stomach and esophageal cancers in China declined, likely due to improvements in hygiene, food quality, preservation methods, and reduced consumption of salty foods.
This study has some limitations. First, only the data from GHDx was used for the temporal trend analysis, so the findings may lack representativeness and should be viewed cautiously. Additionally, differences in data collection and reporting systems between countries may affect the reliability of international comparisons.
5 CONCLUSIONS
To summarize, while China has a slightly lower cancer incidence rate compared to the US and UK, its cancer-related mortality is significantly higher than that in the US and slightly lower than that in the UK. Moreover, China reported significantly higher DALY rates than both the US and the UK. This disparity is largely due to China's unique challenges, including its vast population, uneven regional development, and relatively underdeveloped cancer control strategies. As cancer profile of China shifts from that of a developing country to one more akin to a developed country, the next decade will likely see a continued rise in the cancer burden driven by population aging and the increase in unhealthy lifestyles. In response, the Chinese government should prioritize cost-effective cancer screening and vaccination programs, enforce strict tobacco control measures, and promote healthy lifestyles through education. Moreover, it is essential to tailor the national cancer control program to account for the regional variations in cancer types across the country.
AUTHOR CONTRIBUTIONS
Xiayao Diao, Chao Guo, and Yukai Jin gathered the relevant data, performed the analysis, and drafted the manuscript. Bowen Li, Xuehan Gao, Xin Du, Zhenchong Chen, Minju Jo, Yi Zeng, Chao Ding, Wenwu Liu, and Jianrong Guo performed the analysis and prepared the tables and figures. Haibo Qiu and Shanqing Li conceptualized and designed the study. All authors reviewed and approved the final version of the manuscript.
ACKNOWLEDGEMENTS
This study was funded by the National Postdoctoral Innovation Talent Support Program (BX20240042), National High-Level Hospital Clinical Research Funding (2022-PUMCH-B-011), Natural Science Foundation of Guangdong Province (2022A1515012347), Beijing CSCO research fund (Y-2019Roche-157).
CONFICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
Open Research
DATA AVAILABILITY STATEMENT
The datasets used in this study are all publicly available.




