Age-specific effectiveness of primary human papillomavirus screening versus cytology in a cervical cancer screening program: a nationwide cross-sectional study
Abstract
Background
Primary human papillomavirus (HPV) screening is recommended for the detection of cervical intraepithelial neoplasia (CIN) in the general population; however, the triage for HPV-positive women remains a challenge. This study aimed to evaluate the age-specific effectiveness of primary HPV screening versus primary cytology screening for identifying optimal strategies for women of different ages.
Methods
The dataset of the prevalence round screening was derived from the National Cervical Cancer Screening Program in China. Primary cervical screening protocols included cytology only, HPV testing with cytology triage, and HPV testing with HPV-16/18 genotyping plus cytology triage. The primary outcomes were age-specific detection rate, colposcopy referral rate and positive predictive value (PPV) for CIN2+. Multivariate Poisson regression was used to evaluate the relative effectiveness of HPV testing and cytology according to age groups. The I2 statistic with a random-effect model was used to test the heterogeneity in relative effectiveness of HPV testing versus cytology between age groups.
Results
This study included 1,160,981 women. HPV testing with HPV-16/18 genotyping plus cytology triage significantly increased the CIN2+ detection by 36% (rate ratio [RR]: 1.36, 95% confidential interval [CI] 1.21–1.54) for women aged 35-44 years and by 34% (RR: 1.34, 95% CI 1.20-1.51) for women aged 45-54 years compared with cytology only. HPV testing with cytology triage had similar CIN2+ detection rate compared with cytology only. The PPVs were substantially increased for both HPV testing groups. Among women aged 55-64 years old, HPV testing with HPV-16/18 genotyping plus cytology triage increased the colposcopy referral rate by 19% (RR 1.19, 95% CI 1.10-1.29) compared with cytology only, but did not increase the CIN2+ detection (1.09, 0.91–1.30). The effectiveness of HPV testing with cytology triage did not change in older women. The between-age-group heterogeneity in the effectiveness was statistically significant for HPV testing with HPV-16/18 genotyping plus cytology triage versus cytology only.
Conclusions
Our results suggested that the effectiveness of primary HPV screening with different triage strategies differed among age groups. HPV testing with HPV-16/18 genotyping plus cytology triage could be used for women aged 35-54 years to detect more lesions, and HPV testing with cytology triage could balance the CIN2+ detection and the number of colposcopies for women aged 55-64 years. Longitudinal data including both prevalence and incidence screening rounds are warranted to assess age-specific triage strategies.
Abbreviations
-
- ASC-US
-
- atypical squamous cells of undetermined significance
-
- LSIL, low-grade squamous intraepithelial lesion; CI
-
- confidential interval
-
- CIN
-
- cervical intraepithelial neoplasia
-
- CIN1 +
-
- cervical intraepithelial neoplasia 1 or worse
-
- CIN2 +
-
- cervical intraepithelial neoplasia 2 or worse
-
- GDP
-
- gross domestic product
-
- HPV
-
- human papillomavirus
-
- PPV
-
- positive predictive value
-
- FPR, false-positive rate; RR
-
- rate ratio
1 BACKGROUND
The global strategy to eliminate cervical cancer requires high-performance testing for women by the age of 35 years and again at 45 years [1]. The World Health Organization highly recommends that primary human papillomavirus (HPV) testing should be given to women aged 30-49 years [2]. Although oncogenic HPV testing is known to be more effective in detecting cervical intraepithelial neoplasia (CIN), compared with cytology, and could permit a long term of screening intervals to five years [3], the roll-out of primary HPV screening in a national program is a complex process that requires a balance between the associated benefits (i.e., sensitivity and positive predictive value [PPV] for high-grade CIN) and costs (i.e., colposcopy referral and false-positive rate [FPR]). Choosing the optimal triage strategy for HPV-positive women and achieving a balance between the benefits and costs remains a challenge [2, 4]. Therefore, health policymakers have to make decisions based on the limited evidence and provide general recommendations for all women rather than specific suggestions.
As the first peak of HPV infection is usually observed in youth, previous trials in developed countries mainly focused on the heterogeneity in the effectiveness of HPV testing between women aged 25-34 years old and those aged 35 years old or older. These trials reported that the effectiveness of HPV testing in younger women was possibly similar to or higher than that in older women, and was associated with increased colposcopies and detection of regressive lesions [5-7]. These studies have mostly shown the pooled effectiveness of HPV testing for women aged 30-35 years and above, since HPV prevalence remained low at these ages. In most cases, there is no significant between-age-group heterogeneity in the effectiveness of HPV testing among women older than 35 years. However, a second peak of HPV infection has been observed among women around the age of 50 years, attributed to immunosenescence, changes in sexual behavior, or a cohort effect [8]. This could unavoidably affect the effectiveness of HPV testing in this age group [9, 10]. The second peak increases the number of women with transient HPV infection, and then complicates the choice of triage strategy among older women. Hence, the age-specific effectiveness of primary HPV screening must be carefully considered.
In China, there is a second peak of HPV infection among women around the age of 50-55 years [11]. This could reveal how the epidemic characteristics affect the effectiveness of primary HPV screening at different ages. Based on the national cervical screening program [12], we conducted a real-world study to evaluate the practicality and effectiveness of primary HPV screening in China. In a previous study [13], we compared the effectiveness of HPV testing with cytology in terms of benefits and costs for overall, lower-income and upper-income areas, respectively. This present study aimed to (1) evaluate the age-specific effectiveness of HPV testing with cytology triage, or with HPV-16/18 genotyping plus cytology triage versus cytology only, (2) estimate the between-age-group heterogeneity in the effectiveness of primary HPV screening with different triage strategies versus cytology only, and (3) determine an optimal triage strategy for HPV-positive women of different ages in the prevalence screening round.
2 METHODS
2.1 Data source and design
This was a nationwide, cross-sectional study nested in the organized cervical cancer screening program in rural China which had been previously described in detail [13]. We extracted the individual data of the initial screening round from the program's dataset between January 1, 2015 and December 31, 2017, and divided them into three screening groups according to the strategies: cytology only group – women underwent primary cytology screening; two HPV testing groups – women underwent primary HPV testing with cytology triage, or HPV-16/18 genotyping plus cytology triage. Women in the cytology only group were from 10 provinces, while those in the HPV testing groups were from 26 provinces. Although the allocation of HPV testing or cytology was not randomized, the distribution of participants was on a national scale and ensured comparability between groups. We excluded women aged <35 or >64 years because the program mainly focused on women aged 35-64 years, inadequate samples for HPV testing or cytology, or incomplete records for the primary screening. Because the program only provided primary screening for eligible women but not follow-up care for women who needed repeated screenings, we also excluded women if they were identified as having repeated primary screenings within 3 years after a screening negative.
2.2 Procedures
Screening examinations were performed in local maternal and children hospitals after routine invitation. Cervical exfoliated cells were collected by brush and placed in a liquid medium for cytology examination, HPV testing, or a combination of both. A liquid-based method was used to process the samples, and cytology diagnosis was performed in laboratories based on the location the screenings were performed. HPV testing was performed with different HPV reagents, which were approved by the Chinese Food and Drug Administration, mainly including Hybribio (Guangzhou, China), LiferiverBio (Shanghai, China), SanSure (Changsha, China), YanengBIO (Shenzhen, China), and Cobas 4800 (Roche Molecular Diagnostic, CA, USA) [13-15]. HPV testing was required to target at least 14 carcinogenic HPV genotypes (HPV-16, -18, -31, -33, -35, -39, -45, -51, -52, -56, -58, -59, -66, and -68) with or without HPV genotyping, following validation protocols from the program administration.
In the cytology only group, according to the Bethesda 2001 terminology, atypical squamous cells of undetermined significance or worse (ASC-US+) were considered the threshold of immediate colposcopy referral to increase sensitivity. The reflex HPV test was not used for women with ASC-US. In the HPV testing groups, there were two triage strategies used for HPV-positive women: cytology triage and HPV-16/18 genotyping plus cytology triage. Cytologist was not blinded to HPV testing results. HPV-positive women who underwent cytology triage were referred to colposcopy if they were cytology ASC-US+. HPV-positive women who underwent HPV-16/18 genotyping plus cytology triage were referred to colposcopy if they were positive for HPV-16/18 alone or positive for carcinogenic HPV types other than HPV-16/18 (non-HPV-16/18) types combined with cytology ASC-US+. Women who were positive for either any HPV type without genotyping or non-HPV-16/18 types combined with normal cytology were recommended for intensified screening after 12 months. If women had either visible abnormalities or contact bleeding, they were referred to immediate colposcopy, regardless of screening outcomes. Colposcopy and biopsy were performed in local hospitals according to the clinical guidelines issued by the program [12, 13]. Women with CIN2 or worse (CIN2+) were immediately treated, so CIN2 and CIN3 were not separately recorded. Those with CIN1 or less were recommended for follow-up, but the follow-up care for intensified screening and low-grade CIN were not covered by the program and hence were not included.
2.3 Definitions of outcome measures
Histological results were considered the gold standard for outcome measures. The primary outcomes were CIN2+ as well as CIN1 or worse (CIN1+). In the HPV testing groups, screening positivity had two definitions: 1) women whose primary HPV testing was positive, and 2) women who were positive for any HPV or non-HPV-16/18 types with abnormal cytology, or positive for HPV-16/18 (colposcopy referral). To define the false positive of screening, the following criteria were used to define disease-free women: 1) women who were histologically confirmed negative, 2) women whose triage was negative (no colposcopy referral), 3) women whose primary screening was negative (no triage or colposcopy referral).
2.4 Statistical analysis
We calculated age-specific positive screening rate, colposcopy referral rate, and intensified screening rate with a 95% confidence interval (CI). These indicators were presented by screening age (in 1 year). We calculated the age-specific detection rate, PPV, and FPR for CIN1+ and CIN2+, respectively. PPV was calculated as the number of diseases divided by the number of positive screening women (definition 2). FPR was calculated as the proportion of positive screening women among the disease-free women according to Leinonen et al [16]. Inverse probability weighting was applied to account for the loss-to-follow-up at the colposcopy referral stage.
To show the associations between positive screening and age, we used generalized additive models adjusting for county-level per capita gross domestic product (GDP) and the proportion of women who were ever screened. Based on the observed non-linear patterns of HPV prevalence and reproductive stage of women, we divided women into three age groups: 35-44 years (fertile), 45-54 years (perimenopause), and 55-64 years (post-menopause) [16]. We assumed that the relative effectiveness of HPV testing with different triage strategies versus cytology differed across age groups. We used the Cochran-Armitage test to calculate P values for trend in effectiveness indicators across age groups. The comparison of HPV testing versus cytology was modeled with multivariate Poisson regression and we fitted models for the three age groups as follows: , where Yi is the outcome of interest, β1i and β2i are the effects of HPV testing with the different triage methods versus cytology in the age group of i. The data were converted into adjusted rate ratios (RR) by logarithm transformation. X represents a vector of covariates, including screening age (in 1 year), history of ever screen, and county-level per capita GDP on the basis of tertiles. Pearson's Chi-square method was used to modify an over-dispersed model. We assessed heterogeneity of the RRs between age groups using the I2 statistic with a random-effect model, and P < 0.1 indicated the significance of between-age-group heterogeneity [17].
We performed two sensitivity analyses to measure how the uncertainties of non-random effect and screening threshold could affect the conclusions. First, we conducted the analyses of a more balanced sample using propensity score matching. A caliper matching algorithm with a caliper value of 0.1 standard deviation was used to match the individuals within the three screening groups in a 1:1:1 ratio. Second, we changed the threshold of colposcopy referral in the cytology only group to a low-grade squamous intraepithelial lesion or worse (LSIL+) because this threshold is usually used in organized screening programs. We then compared the age-specific effectiveness of HPV testing with different triage strategies versus cytology only, assuming that a threshold of LSIL was used in the program.
All statistical tests were two-sided, and statistical significance was set at P < 0.05. Analyses were performed using SAS v.9.4 (SAS Institute, Cary, NC, USA) and R software v.3.5.4 (R Foundation for Statistical Computing, Vienna, Austria).
2.5 Ethics approval
The Ethics Committee of the National Center for Maternal and Child Health, Chinese Center for Disease Control and Prevention approved the present study (No. FY2016-009) and waived the requirement for informed consent from individuals as the data were obtained from a government-supported program and analyzed anonymously.
3 RESULTS
The study included 1,160,981 women aged 35-64 years, of whom 327,512 underwent cytology only, 243,174 underwent HPV testing with cytology triage, and 590,295 underwent HPV testing with HPV-16/18 genotyping plus cytology triage (Table 1). In the cytology only group, 13,224 women (4.0%) were screened with ASC-US+. In the HPV testing group with cytology triage, 24,251 women (10.0%) were positive for HPV and 5256 (2.2%) were referred to colposcopy. In the HPV testing group with genotyping triage, 60,340 women (10.2%) were positive for HPV and 23,776 (4.0%) were referred to colposcopy (Figure 1). Finally, cytology only, HPV testing with cytology triage, and HPV testing with genotyping triage had 3542 (12.7 per 1000), 1585 (7.3 per 1000), and 6620 (12.6 per 1000) cases with any CIN or cancer, respectively.
| Characteristic | Cytology only | HPV testing with cytology triage | HPV testing with HPV-16/18 genotyping plus cytology triage | P |
|---|---|---|---|---|
| Total | 327,512 | 243,174 | 590,295 | |
| Age, years (Median [P25, P75]) | 48.0 (42.0, 53.0) | 46.0 (40.0, 52.0) | 47.0 (42.0, 53.0) | <0.001 |
| Age group, n (%) | <0.001 | |||
| 35-44 years | 115,312 (35.2) | 103,752 (42.7) | 223,783 (37.9) | |
| 45-54 years | 143,483 (43.8) | 98,279 (40.4) | 256,465 (43.5) | |
| 55-64 years | 68,717 (21.0) | 41,143 (16.9) | 110,047 (18.6) | |
| Ever screening, n (%)* | <0.001 | |||
| Yes | 118,602 (36.3) | 67,754 (27.9) | 216,405 (36.7) | |
| No | 208,591 (63.7) | 175,000 (72.1) | 373,376 (63.3) | |
| Screening positive, n (%) | 13,224 (4.0) | 24,251 (10.0) | 60,340 (10.2) | <0.001 |
| Colposcopy referral, n (%) | 13,224 (4.0) | 5256 (2.2) | 23,776 (4.0) | <0.001 |
| Attendance of colposcopy, n (%) | 11,273 (85.3) | 4681 (89.1) | 19,923 (83.8) | <0.001 |
| Detection of diseases, n (per 1000) | ||||
| CIN1+ | 3542 (12.7) | 1585 (7.3) | 6620 (12.6) | <0.001 |
| CIN2+ | 1222 (4.4) | 962 (4.4) | 2898 (5.9) | <0.001 |
| Positive predict value, % | ||||
| CIN1+ | 31.2 | 33.8 | 30.7 | <0.001 |
| CIN2+ | 10.7 | 20.6 | 14.3 | <0.001 |
| False-positive rate, % | ||||
| CIN1+ | 2.4 | 1.3 | 2.4 | <0.001 |
| CIN2+ | 3.1 | 1.5 | 2.9 | <0.001 |
- Note: *there were 1253 missing data in the variable, including 319 in cytology only group, 420 in HPV testing with cytology group, and 514 in HPV testing with HPV-16/18 genotyping plus cytology triage group.
- HPV, human papillomavirus. CIN, cervical intraepithelial neoplasia.
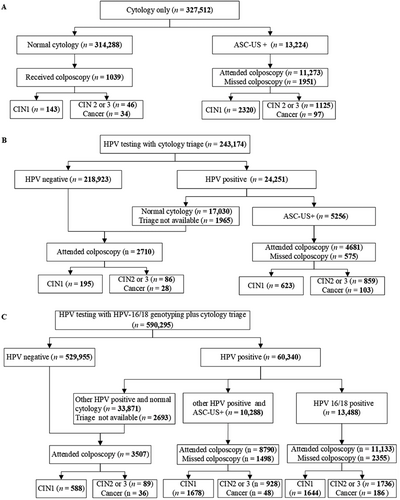
Flow diagram of eligible women for the HPV testing and cytology in the study.
Abbreviations: HPV, human papillomavirus. CIN, cervical intraepithelial neoplasia. ASC-US, atypical squamous cells of undetermined significance.
Women in the three screening groups were of similar age and were similarly distributed across age groups although the difference was statistically significant (Figure 2A). The age-specific cytological abnormal rate ranged from 3.0% to 4.6%, and the HPV positive rates were highly concordant between the two HPV testing groups ranging from 8.6% to 14.2% (Figure 2B). The associations between age and screening positivity differed between the cytology only and HPV testing groups (Figure 2C-E). Specifically, for women at the age of 55 years or older, the positive association of age and screening positivity became stronger in the HPV testing groups, but not in the cytology only group.
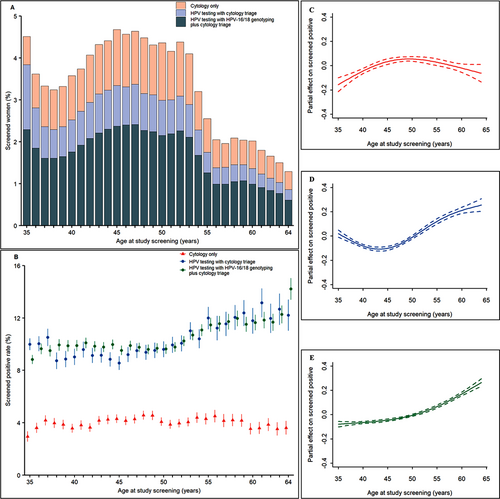
The proportion of screened women and age-specific screening positive rate of the three screening groups: (A) proportion of screened women by age; (B) age-specific screening positive rate. (C-E) Associations between age and screening positive by cytology only (C), HPV testing with cytology triage (D), and HPV testing with HPV-16/18 genotyping plus cytology triage (E).
Error bar and dotted line indicate 95% confidence intervals.
Abbreviations: HPV, human papillomavirus.
Accordingly, age-specific colposcopy referral rates and intensified screening rates in the HPV testing groups also increased with increasing age (Figure 3). The colposcopy referral rates were similar between HPV testing with HPV-16/18 genotyping plus cytology triage and cytology only groups, but significantly lower in HPV testing with cytology triage group. The intensified screening rates were significantly higher in HPV testing with cytology triage group than that in HPV-16/18 genotyping plus cytology triage after the age of 45 years old.
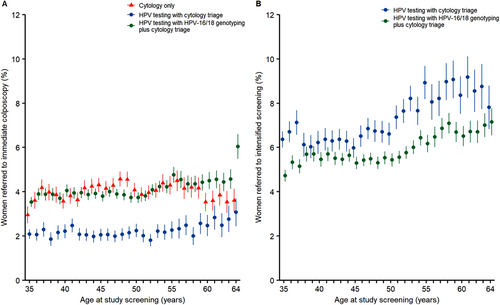
Age-specific colposcopy referral and intensified screening rates of the three screening groups. (A) Age-specific colposcopy referral rate. (B) Age-specific intensified screening rate.
Error bar indicates 95% confidence intervals.
Abbreviations: HPV, human papillomavirus.
Figure 4 shows that the age-specific detection rates of CIN1+ and CIN2+ differed between the two HPV testing groups. Specifically, the HPV testing with cytology triage group had similar CIN2+ detection rates compared with the cytology only group for women at the age of 35-64 years. The HPV testing with HPV-16/18 genotyping plus cytology triage group detected more cases of CIN2+ than the cytology only group among women aged 35-54 years, but not among women aged 55-64 years.
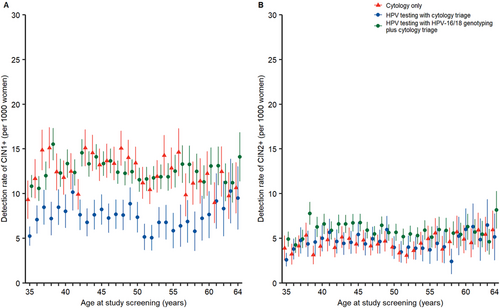
Age-specific detection rates of CIN1+ and CIN2+ in the three screening groups. (A) Age-specific detection rates of CIN1+. (B) Age-specific detection rates of CIN2+.
Error bar indicates 95% confidence intervals.
Abbreviations: HPV, human papillomavirus. CIN, cervical intraepithelial neoplasia.
Table 2 shows the relative effectiveness of CIN detection and colposcopy referral between the HPV testing and cytology only groups by age. Among women aged 35-54 years, colposcopy referral rate in the HPV testing with cytology triage group was reduced by 44% (RR = 0.56, 95% CI = 0.50–0.62) compared with the cytology only group among women aged 35-44 years, and reduced by 51% (RR = 0.49, 95% CI = 0.45–0.54) among women aged 45-54 years, whereas the detection rates of CIN2+ were similar between the two groups. Conversely, colposcopy referral rates were similar in the HPV testing with HPV-16/18 genotyping plus cytology triage group compared with the cytology only group, but the detection rates of CIN2+ were increased by 36% (RR = 1.36, 95% CI = 1.21–1.54) for women aged 35-44 years and by 34% (RR = 1.34, 95% CI = 1.20-1.51) for those aged 45-54 years. Among women aged 55-64 years, the colposcopy referral rate was reduced by 38% in the HPV testing with cytology triage group compared with the cytology only group (RR = 0.62, 95% CI = 0.55–0.69), and the detection rates of CIN2+ were similar between the two groups. The colposcopy referral rate was increased by 19% in the HPV testing with genotyping triage group compared with the cytology only group (RR = 1.19, 95% CI = 1.10-1.29), but the difference in the CIN2+ detection rates between the two groups was not statistically significant (P = 0.359). Substantial between-age-group heterogeneity in both colposcopy referral and CIN2+ detection was noted in the HPV testing with genotyping triage group (P < 0.1).
| Colposcopy referral | CIN1+ | CIN2+ | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Age group | Rate (per 1000) | RR (95% CI) | P | Detection rate (per 1000) | RR (95% CI) | P | Detection rate (per 1000) | RR (95% CI) | P |
| Cytology only | |||||||||
| 35-44 years | 3.8 | Reference | NA | 12.9 | Reference | NA | 4.3 | Reference | NA |
| 45-54 years | 4.2 | Reference | NA | 13.1 | Reference | NA | 4.1 | Reference | NA |
| 55-64 years | 4.0 | Reference | NA | 11.6 | Reference | NA | 5.1 | Reference | NA |
| P for trend | 0.025 | NA | NA | 0.034 | NA | NA | 0.048 | NA | NA |
| HPV testing with cytology triage | |||||||||
| 35-44 years | 2.1 | 0.56 (0.50–0.62) | < 0.001 | 7.4 | 0.58 (0.50–0.68) | < 0.001 | 4.3 | 0.99 (0.85–1.15) | 0.869 |
| 45-54 years | 2.1 | 0.49 (0.45–0.54) | < 0.001 | 7.1 | 0.54 (0.47–0.63) | < 0.001 | 4.5 | 1.09 (0.94–1.27) | 0.249 |
| 55-64 years | 2.5 | 0.62 (0.55–0.69) | < 0.001 | 7.4 | 0.65 (0.53–0.79) | < 0.001 | 4.7 | 0.93 (0.73–1.18) | 0.558 |
| P for trend | < 0.001 | NA | NA | 0.805 | NA | NA | 0.222 | NA | NA |
| P for heterogeneity† | NA | 0.009 | NA | NA | 0.354 | NA | NA | 0.465 | NA |
| HPV testing with HPV-16/18 genotyping plus cytology triage | |||||||||
| 35-44 years | 3.9 | 0.99 (0.92–1.06) | 0.715 | 12.9 | 0.96 (0.86–1.07) | 0.436 | 6.0 | 1.36 (1.21–1.54) | < 0.001 |
| 45-54 years | 3.9 | 0.92 (0.87–0.98) | 0.008 | 12.3 | 0.87 (0.79–0.96) | 0.006 | 5.8 | 1.34 (1.20-1.51) | < 0.001 |
| 55-64 years | 4.6 | 1.19 (1.10-1.29) | < 0.001 | 12.5 | 1.03 (0.91–1.18) | 0.612 | 5.7 | 1.09 (0.91–1.30) | 0.359 |
| P for trend | < 0.001 | NA | NA | 0.233 | NA | NA | 0.214 | NA | NA |
| P for heterogeneity† | NA | < 0.001 | NA | NA | 0.107 | NA | NA | 0.093 | NA |
- Abbreviations: HPV, human papillomavirus. CIN, cervical intraepithelial neoplasia. RR, rate ratio. CI, confidential interval. NA, not applicable.
- Note: RRs and P values for HPV testing groups were obtained by comparison with cytology only group.
- † P < 0.1 was regarded as substantial between-age-group heterogeneity in the relative effectiveness of HPV testing versus cytology.
Table 3 shows the relative PPV and FPR for CIN1+ and CIN2+ between the HPV testing and cytology only groups by age. Among women aged 35-54 years old, when compared with the cytology only group, the PPV for CIN2+ was significantly increased by 66% (RR = 1.66, 95% CI = 1.23–2.24) for women aged 35-44 years and by 108% (RR = 2.08, 95% CI = 1.54–2.82) for those aged 45-54 years, and FPRs were reduced by approximately 50% in the HPV testing with cytology triage group. Similarly, the PPV for CIN2+ was significantly increased in the HPV testing with HPV-16/18 genotyping plus cytology triage group for women aged 35-44 years (RR = 1.40, 95% CI = 1.10-1.79) and 45-54 years (RR = 1.44, 95% CI = 1.14–1.83), and FPRs were slightly reduced without statistical significance (P > 0.1 for both). Among women aged 55-64 years, the PPV for CIN2+ of the HPV testing with cytology triage group versus the cytology only group increased without significance (P = 0.098), but the reduction of the FPR remained significant (RR = 0.61, 95% CI = 0.39–0.94). However, the RR for the PPV of HPV testing with genotyping triage versus cytology only decreased to 0.92 (95% CI = 0.69–1.22), and the RR for the FPR increased to 1.20 (95% CI = 0.91–1.60). Substantial between-age-group heterogeneity in PPV was observed in the HPV testing with genotyping triage group (P = 0.035).
| CIN1+ | CIN2+ | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age group | PPV(%) | RR (95% CI) | P | FPR(%) | RR (95% CI) | P | PPV(%) | RR (95% CI) | P | FPR(%) | RR (95% CI) | P |
| Cytology only | ||||||||||||
| 35-44 | 33.3 | Reference | NA | 2.3 | Reference | NA | 11.2 | Reference | NA | 3.0 | Reference | NA |
| 45-54 | 30.7 | Reference | NA | 2.5 | Reference | NA | 9.6 | Reference | NA | 3.3 | Reference | NA |
| 55-64 | 28.6 | Reference | NA | 2.4 | Reference | NA | 12.5 | Reference | NA | 2.9 | Reference | NA |
| P for trend | < 0.001 | NA | NA | 0.009 | NA | NA | 0.258 | NA | NA | 0.783 | NA | NA |
| HPV testing with cytology triage | ||||||||||||
| 35-44 | 35.4 | 1.00 (0.76–1.32) | 0.975 | 1.3 | 0.56 (0.36–0.87) | 0.009 | 20.4 | 1.66 (1.23–2.24); | 0.001 | 1.5 | 0.52 (0.34–0.78); | 0.002 |
| 45-54 | 34.3 | 1.06 (0.76–1.46) | 0.729 | 1.2 | 0.48 (0.31–0.33) | < 0.001 | 21.8 | 2.08 (1.54–2.82); | < 0.001 | 1.4 | 0.44 (0.30–0.65); | < 0.001 |
| 55-64 | 29.6 | 0.96 (0.66–1.38) | 0.862 | 1.6 | 0.64 (0.40-1.03) | 0.066 | 18.8 | 1.37 (0.94–1.99); | 0.098 | 1.8 | 0.61 (0.39–0.94); | 0.024 |
| P for trend | 0.002 | NA | NA | <0.001 | NA | NA | 0.538 | NA | NA | 0.012 | NA | NA |
| P for heterogeneity† | NA | 0.931 | NA | NA | 0.665 | NA | NA | 0.215 | NA | 0.550 | NA | |
| HPV testing with HPV-16/18 genotyping plus cytology triage | ||||||||||||
| 35-44 | 32.8 | 1.01 (0.83–1.24) | 0.897 | 2.2 | 0.95 (0.70-1.31); | 0.774 | 15.4 | 1.40 (1.10-1.79); | 0.005 | 2.7 | 0.89 (0.66–1.20); | 0.457 |
| 45-54 | 30.9 | 0.96 (0.77–1.19) | 0.716 | 2.3 | 0.94 (0.72–1.23); | 0.656 | 14.5 | 1.44 (1.14–1.83); | 0.003 | 2.9 | 0.87 (0.68–1.11); | 0.273 |
| 55-64 | 26.8 | 0.87 (0.68–1.11) | 0.272 | 2.9 | 1.26 (0.92–1.73); | 0.157 | 12.3 | 0.92 (0.69–1.22); | 0.566 | 3.4 | 1.20 (0.91–1.60); | 0.188 |
| P for trend | < 0.001 | NA | NA | <0.001 | NA | NA | <0.001 | NA | NA | < 0.001 | NA | NA |
| P for heterogeneity† | NA | 0.646 | NA | NA | 0.321 | NA | NA | 0.035 | NA | NA | 0.187 | NA |
- HPV, human papillomavirus. CIN, cervical intraepithelial neoplasia. PPV, positive predicted value. FPR, false-positive rate. RR, rate ratio. CI, confidential interval. NA, not applicable.
- Note: RRs and P values for HPV testing groups were obtained by comparison with cytology only group.
- † P < 0.1 was regarded as substantial between-age-group heterogeneity in the relative effectiveness of HPV testing versus cytology.
Sensitivity analyses showed that the findings were similar when estimates based on the post-matching data (n = 679,257) were compared with the main results (Supplementary Table S1-S2). Furthermore, when the threshold of referral in cytology changed to LSIL+, substantial between-age-group heterogeneity was also observed (Supplementary Table S3-S4). These results indicate the robustness of the analyses and substantial between-age-group heterogeneity in the effectiveness of HPV testing.
4 DISCUSSION
To our knowledge, this is the largest study to reveal the between-age-group heterogeneity in the age-specific effectiveness of HPV testing versus cytology for detecting high-grade CIN after the age of 35 years. Although primary HPV screening is highly recommended for women aged 30 years or older, the optimal triage strategy for HPV-positive women remains a challenge [2, 4]. Our results showed that the effectiveness of HPV testing with cytology triage or HPV-16/18 genotyping plus cytology triage versus cytology only differed between women aged 35-54 years and those aged 55-64 years. This difference may be related to the second peak of HPV infection in older women in China. This means that the different triage strategies should be reconsidered for older and younger HPV-positive women when moving to the era of primary HPV screening.
Our findings support the triage of HPV16/18 genotyping plus cytology for women aged 35-54 years in primary HPV screening. For women aged 35-44 years or 45-54 years, compared with cytology only, HPV testing with genotyping triage was more sensitive (RR = 1.36 and 1.34, respectively) and had a higher PPV (RR = 1.40 and 1.44, respectively) for the detection of CIN2+, and had similar colposcopy referrals (RR = 0.99 and 0.92, respectively). In contrast, HPV testing with reflex cytology had similar detection of CIN2+ (RR = 0.99 and 1.09, respectively) compared with cytology only, although it substantially decreased the colposcopy referrals (RR = 0.56 and 0.49, respectively) and FPR (RR = 0.89 and 0.87). These findings are in line with the present understanding of sensitivity for HPV testing with HPV16/18 genotyping triage [18, 19]. In contrast to the results of studies conducted in Western countries [20, 21], HPV testing with cytology triage was not more sensitive than cytology in the present study. This could be attributed to the low threshold of referral in cytology (ASC-US+) and the fact that follow-up for HPV-positive women with normal cytology was not assured within 12 months. Detecting more high-grade CIN in the prevalence screening round would not only reduce the load of follow-up but also avert the loss to follow-up. Moreover, a negative HPV test could permit an extension of the screening interval to 5 years or longer [22].
Our results showed lower effectiveness of primary HPV screening in women aged 55-64 years compared with that in younger women, which were not in line with previous studies [5-7, 20-22]. The difference in CIN2+ detection between the HPV testing with HPV-16/18 genotyping plus cytology triage and the cytology only was not significant (RR = 1.09, P > 0.05), whereas the colposcopy referrals substantially increased (RR = 1.19). Likewise, the relative PPV between the two groups substantially decreased but the FPR increased. This means that the HPV 16/18 genotyping triage group may not benefit from the increased sensitivity and may be harmed by the burden of colposcopy referrals and psychological stress [23]. Similarly, a previous study showed that most high-grade lesions in women aged 55-59 years were positive for non-HPV-16/18 HPV, and HPV-16/18 strategy may introduce many false-negative cases [9]. In contrast, the HPV testing with cytology triage group had a lower FPR and relatively higher PPV compared with the cytology only group, but not at the expense of the reduction of CIN2+ detection, which was consistent with results in Sweden [9] and Danish [10] studies. Nonetheless, both strategies have limitations for the triage of older HPV-positive women, and an alternative triage method is warranted. Overall, cytology triage would be a balanced choice for HPV-positive women aged 55-64 years.
A possible contributing factor for the between-age-heterogeneity in relative effectiveness between HPV testing and cytology is the second peak of HPV infection in older women, which was mostly observed in areas such as China [11], East Africa [8], and Latin America [8]. The rebound of HPV infection at the age of 50 years and above has been believed to be associated with immune responses and sexual behavior change [8, 11]. Newly acquired infections do not advance to CIN rapidly at this age. Hence, it is unavoidable to increase the number of unnecessary colposcopies. Another explanation for the lower relative effectiveness of HPV testing versus cytology at older ages is using the threshold of ASC-US [24, 25]. Because the advancement of the HPV infection to CIN3 or worse is slower in older women than in younger women [24], CIN cells that remain stable at this age will be less likely to be missed by cytologists. The atrophy of cervical exfoliated cells due to drops in estrogen levels would also catch the attention of cytologists, altering the ASC-US classification [26]. Some studies suggest that lesions in older women may not be recognized by Pap smear due to the disappearance of the transformation zone [27, 28], also affecting the reflex cytology for HPV-positive women.
The clearance of HPV infection was slower in post-premenopausal women and then may advance into the persistent infection [28, 29]. Many newly diagnosed cervical cancers are found among women over 60-65 years of age [30], and appropriate screening for women who are close to the age of stopping regular screening (65 years old) could help to reduce the risk of cervical cancer in the following years. Two rounds of screening (prevalence and incidence rounds) could show the efficacy of screening in the long term [21, 22]. However, China just introduced HPV testing in the program since 2014 and could not afford two screening rounds for a woman because of limited resources. A strategy that is more sensitive in the prevalence screening round would be preferred. However, a strategy like HPV-16/18 genotyping requires more colposcopies, which are also subject to resource constraints. The expansion of the HPV vaccination also inevitably affects the performance of screening tests. For example, HPV vaccines could sharply decrease HPV-16/18 prevalence and increase the proportions of non-HPV-16/18, which have implications for benefit of the HPV-16/18 genotyping test [31, 32]. Likewise, the reduction of precancerous lesions will affect the PPV of cytology. In China, the HPV vaccine was just licensed during 2017-2019, and participants in the present study were unlikely to be vaccinated. Nonetheless, longitudinal data linking multiple rounds of screening, immunization status, and outcomes are warranted in the future.
The key limitation of this study is that the allocation of cytology and HPV testing was not random. Since the counties were distributed homogeneously within groups and the scale was large, the prevalence of CIN2+ was comparable among groups. Cytology tests were not performed in centralized laboratories, and the variations among cytopathologists may affect the performance of cytology. Furthermore, different domestic HPV reagents have been used to detect HPV infections. The statistical analyses were deficient in such data because of differences in performance among tests, but these are unlikely to have affected the principal conclusion that the effectiveness of HPV testing versus cytology differed across age groups. Finally, our study only included the results of a single round of screening. Analyses of multi-rounds of screening are beyond the scope of this study and are required to further study optimal age-specific primary HPV screening strategies.
In conclusion, the effectiveness of HPV testing significantly differed between women aged 35-54 years and those aged 55-64 years, which may be related to the second peak of HPV infection in older women. For women aged 35-54 years, HPV-16/18 genotyping plus cytology triage could be preferred for detecting more CIN2+ lesions. For women aged 55-64 years, cytology triage could better balance the CIN2+ detection and number of colposcopies. Further longitudinal studies including both prevalence and incidence rounds of screening are warranted for the age-specific triage strategies in primary HPV screening.
AUTHOR'S CONTRIBUTORS
HJW and JLW take responsibility for the integrity of the data, supervise the study, and have verified the underlying data. HLB, LM, HJW, and JLW conceived this study. YXZ, LM, LHW, WHR, and JLW performed the investigation and data collection. HLB, HJW, and SW performed formal analysis, visualization, and validation. HLB and LM drafted the manuscript. All authors revised the manuscript and approved the final manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval for the National Cervical Cancer Screening Program in Rural Areas is provided by the Ethics Committee of the National Center for Women and Children's Health, Chinese Center for Disease Control and Prevention. All participants provided written informed consent before the screening procedures. The Ethics Committee approved the use of the database and the present study protocol and waived the informed consent from the individual as the data used in this study were obtained from a national program established by the government.
CONSENT FOR PUBLICATION
Not applicable.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no conflicts of interest.
ACKNOWLEDGMENTS
We thank all research staff from institutes for maternal and child health care in provinces, cities, districts, and counties for their hard work in the implementation of the program and collection of data. We thank all experts from the national technical group of the program for the quality control. We also thank Fanghui Zhao (Cancer Hospital Chinese Academy of Medical Sciences), Lihui Wei (Peking University People's Hospital), Youlin Qiao (Cancer Hospital Chinese Academy of Medical Sciences), Yan Wang (Peking University), and Wen Chen (Cancer Hospital Chinese Academy of Medical Sciences) for advice and support on study design and formal revision of the study.
FUNDING
This study was supported by grants from the National Natural Science Foundation of China (grant no 81903328) and the Chinese Key Project of Public Health Program. The funders were not involved in the design, conduct, or reporting of the study; the writing of the manuscript; or the decision to publish the manuscript.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author, upon reasonable request.




