Cancer burden of major cancers in China: A need for sustainable actions
Abstract
Cancer is still a major health problem in China although numerous efforts have been made for its prevention and control. Findings from this study showed that lung cancer remains the most common type of cancer diagnosed, and was attributed to nearly 30% of all cancer-related deaths. The incidence of the five most common cancers, in China, in 2015, including cancers of the lungs, stomach, colorectum, liver and breast, accounted for almost 60% of all cancers diagnosed. The high cancer burden in China highlights the need for further improvement in health education, professional training and the building up an anti-cancer network for introducing and implementing sustainable actions for cancer control.
Cancer is a major global health issue and the leading cause of death in China [1, 2], with 4,285,033 new cases and 2,865,174 deaths recorded in 2018, according to the Global Cancer Observatory [3]. Recently, the American Cancer Society reported the updated cancer incidence and mortality rates in America which demonstrated a significant decrease in overall cancer mortality trend from 1991 to 2017 by a total of 29% [4]. However, the cancer burden in China remains at a high level despite improvements in health care and increasing funding on cancer control. Population-based cancer registration plays a key role in monitoring cancer burden by collecting incident cases and deaths of cancer and evaluating the effectiveness of public health strategies. The cancer registry in China has been making impressive progress on data quality and representativeness since the 1990s, covering up to 438 million people and accounting for 31.5% of the entire Chinese population in 2018 [5].
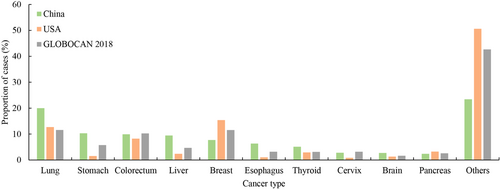
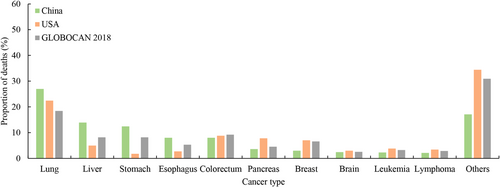
After sorting by new incident cases in both sexes, lung cancer was still the most common cancer, followed by stomach and colorectal cancer, and had an estimated number of 787,000 new cases in 2015, in China. Lung cancer was also the leading cause of cancer-related deaths. The age-standardized mortality rate of lung cancer adjusted by the Chinese stand population was 28.16 cases per 100,000 people. Nearly 30% of cancer deaths were related to lung cancer. In the urban and rural areas, lung cancer also remained the most common malignant tumor and the main cause of death. Breast cancer was the most frequently diagnosed cancer in Chinese women, with an estimated number of 304,000 new cases in the year 2015, which was the equivalent of more than 800 new cases each day. The age-standardized incidence rate per 100,000 people by the Chinese stand population was 1.4 times as high in urban areas as in rural areas (35.75 vs. 25.53 cases per 100,000 people). Gastric cancer was estimated as the second most common cancer diagnosed in China, responsible for around 403,000 new cases in 2015 (281,000 males and 122,000 females) and the third cause of mortality among all cancer types; of which a total of 291,000 persons died from it. Its number of deaths was similar in urban and rural areas (143,000 vs. 147,000 deaths). Colorectal cancer was estimated as the third most common cancer diagnosed and fifth in cancer-related death, of which the numbers of new cases and deaths in 2015 were estimated at 388,000 and 187,000. Colorectal cancer was the second most common cancer among urban residents and fifth in rural areas. A lower mortality rate from colorectal cancer was observed in rural areas. Liver cancer was the fourth most common cancer and the second leading cause of cancer-related death in China, with an estimated number of 370,000 new cases and 326,000 cancer-related deaths in 2015. The 5 most common cancer cases in both sexes accounted for almost 60% of all cancers in China. The comparative distribution of the percentages of the number of the most common cancer cases and deaths in China and America1 are presented in Figure 1 and 2. All cancer data reported above were extracted from the 2015 report of the cancer epidemiology in China [5].
The cancer patterns presented disparity in different rural and urban areas and showed temporal change. In addition, the cancer burden was different between males and females. For instance, areas with higher liver cancer incidence and mortality rates were concentrated in the Jiangsu province, together with some coastal counties in the southeast of China. The incidence of breast cancer was higher in some developed areas, such as eastern coastal urban areas [6]. From 2000-2011, an increasing trend of lung cancer incidence was observed in females [7]. For cancer-related mortality, according to the WHO Mortality Database, the average annual percentage change (AAPC) of age-standardized mortality from colorectal cancer increased by 0.7% from 1987 to 2000 [8]. An increasing trend of liver cancer mortality was also observed from 1991 to 2011 [9]. Overall, urban China had a higher cancer incidence and lower mortality than rural China. The top 5 commonly diagnosed cancers in the urban areas, in terms of new cases in the year 2015, were cancers of the lung and colorectum, followed by female breast cancer, stomach cancer and liver cancer, whereas the main cancers in the rural areas were lung cancer, stomach cancer, liver cancer, esophageal cancer and colorectal cancer. In terms of all cancers combined in China, the age-standardized incidence (207.99 vs 175.47 cases 100000 people) and age-standardized mortality rates (139.13 vs 75.92 deaths per 100000 people) were much higher in males, compared to females. The leading cancer types for the estimated new cancer cases and deaths by sex are presented in Table 1. The majority of the number of cases was from lung, stomach, liver, colorectal and esophageal cancers in males and were breast, lung, colorectal, thyroid and stomach cancers in females. Lung cancer was the commonest cause of cancer-related death in both genders [5].
| Estimated new cancer cases | |||||
|---|---|---|---|---|---|
| Male | Female | ||||
| Sites | Cases (10000 people) | Percent (%) | Sites | Cases (10000 people) | Percent (%) |
| Lung | 52.0 | 24.2 | Breast | 30.4 | 17.1 |
| Stomach | 28.1 | 13.1 | Lung | 26.7 | 15.0 |
| Liver | 27.4 | 12.7 | Colorectum | 16.3 | 9.2 |
| Colorectum | 22.5 | 10.5 | Thyroid | 15.1 | 8.5 |
| Esophagus | 17.7 | 8.2 | Stomach | 12.2 | 6.9 |
| Prostate | 7.2 | 3.3 | Cervix | 11.1 | 6.2 |
| Bladder | 6.2 | 2.9 | Liver | 9.6 | 5.4 |
| Pancreas | 5.4 | 2.5 | Uterine Corpus | 6.9 | 3.9 |
| Lymphoma | 5.2 | 2.4 | Esophagus | 6.9 | 3.9 |
| Brain | 5.0 | 2.3 | Brain | 5.7 | 3.2 |
| Others cancer type | 38.4 | 17.9 | Others cancer type | 36.9 | 20.8 |
| All cancers | 215.1 | 100 | All cancers | 177.8 | 100 |
| Estimated cancer deaths | |||||
|---|---|---|---|---|---|
| Male | Female | ||||
| Sites | Deaths (10000 people) | Percent (%) | Sites | Deaths (10000 people) | Percent (%) |
| Lung | 43.3 | 29.3 | Lung | 19.7 | 23.0 |
| Liver | 24.2 | 16.4 | Stomach | 9.0 | 10.5 |
| Stomach | 20.1 | 13.6 | Liver | 8.4 | 9.8 |
| Esophagus | 13.7 | 9.3 | Colorectum | 7.8 | 9.1 |
| Colorectum | 11.0 | 7.4 | Breast | 7.0 | 8.2 |
| Pancreas | 4.8 | 3.2 | Esophagus | 5.1 | 5.9 |
| Leukemia | 3.2 | 2.2 | Pancreas | 3.6 | 4.2 |
| Brain | 3.1 | 2.1 | Cervix | 3.4 | 4.0 |
| Lymphoma | 3.1 | 2.1 | Brain | 2.5 | 2.9 |
| Prostate | 3.1 | 2.1 | Ovary | 2.5 | 2.9 |
| Others cancer type | 18.4 | 12.4 | Others cancer type | 16.8 | 19.6 |
| All cancers | 148.0 | 100 | All cancers | 85.8 | 100 |
The age-specific cancer incidence was observed to increase with age. It was lowest among the population within the age group of 35-39 years old and then increased substantially, peaking in the 80-84-year age group. Women aged less than 50 years had lower cancer incidence, both in urban and rural areas. Nearly for all age groups, the incidence from all cancer combined was slightly higher in urban women, compared to rural women. The age-specific mortality also showed a continuously increasing trend by age. In males, the age-specific mortality in rural areas was higher for people with an age < 75 years old and over 4 years old as compared to urban residents. Age-specific mortality for rural females was higher within the age group 20-74 years old than urban females [5]. The distribution of age-specific incidence varied by cancer types. For instance, for female breast cancer, the mean age at diagnosis was 45-55 years old and the incidence peak was estimated in the 50-54 years group [10], whereas the mean age at diagnosis for liver cancer was higher. According to data from the China national cancer registry, the mean diagnosed age of liver cancer in 2014 was 62.35 years in men and 68.99 years in women [11]. People aged 65-70 years old accounted for the largest proportion of the total lung cancer patients [12]. For digestive cancer, the risk of gastric cancer [13] and esophageal cancer[14] increased in adults over 40 years in China, while the incidence from colorectal cancer began to increase obviously from the age of 50 years [8].
In recent years, the Chinese government has issued a series of comprehensive guidelines and actions to decrease the cancer burden [15-18]. Generally, the strategies could be broadly categorized into three types, namely, promoting health education and increasing cancer awareness, emphasizing the importance of early cancer detection and treatment, and improving the level of clinical treatment. The priority of primary prevention is to find possible risk factors associated with cancer risk. A series of epidemiological studies were conducted to identify potential risk factors [19-22] which provided critical evidence for targeted interventions. Nationally, cigarette smoking is considered as the main cause of lung cancer [23]. The first tobacco control law was introduced in China in the early 1990s and on October 11, 2005. Further, the World Health Organization Framework Convention on Tobacco Control has also been ratified in China [24]. However, despite such implementation, the prevalence of smoking is still currently high. The tobacco smoking rates in Yunnan (28.2%) and Northeastern areas are much higher and have also relatively higher lung cancer mortality, compared to Hainan (20.9%) and Xinjiang (16.2%) [25]. The increasing trend of lung cancer incidence suggested that measures to reduce the prevalence of smoking should be stricter. Local culture, education levels and economic capacity should be considered in future anti-tobacco policies, for which areas with higher lung cancer mortality deserve more attention.
The full-coverage of hepatitis B vaccination played an important role in reducing the liver cancer burden [26]. However, the protective effect of vaccination is seriously lagging. Thus, the benefit of vaccination could not be instantly obvious. The occurrence of cancer is complex, multifactorial, and occurs through different stages. Therefore, it is difficult to urge cancer burden through primary prevention. Thus, since 2005, with the support of governmental funding, a great deal of mass screening has been gradually conducted, covering rural and urban areas, and some high-risk regions. At present, cancers of the lung, esophagus, stomach, colorectum, liver, nasopharynx, female breast, and cervix are all enrolled into the scope of free screening.
Developments in artificial intelligence [27] and the introduction of accurate screening methods could reduce false negatives and increase diagnostic sensitivity. In addition, simple and novel technologies for early detection are also in great need in China, such as self-sampling for cervical cancer screening [28], although the acceptance was previously observed as being low, more emphasis should be placed on such technologies. Data from the National Cancer Registry of China (NCCRC) showed that cancer survival increased substantially for the overall combined cancers from 2003 to 2015 [29], which could be partly attributed to the implementation of mass screening, although the effectiveness of screening on liver cancer was unclear [30-32]. Other reasons to improve cancer survival may include improvements in the health care system and New Cooperative Medical Scheme [33-35]. Additionally, the policy of zero-tariff on the import of anti-cancer drugs has dramatically alleviated the economic and mental burden of cancer patients. With the expansion of medical insurance and a decrease in the price of anti-cancer medications, more and more patients, since recent years, can now afford cancer treatments. Hospitals are also being reformed according to guidelines for establishing more modern hospital management system. In the future, the diagnosis and treatment of cancer will be more convenient, affordable and quicker.
Cancer burden diversifies at provinces and population level, due to the differences in sociodemographic characteristics, screening methods and other factors. High-quality population-based epidemiological data offer the opportunity to identify the distribution features of the main cancers, indicating some underlying risk factors. Cancer control strategies and policies should be timely implemented based on different cancer statistics. The National Cancer Registry of China was first established in Henan and Shanghai provinces. It has performed fundamental work by providing scientific basic information and targeted directions for cancer prevention and control, which started from the 1960s. Since the year 2008, as the National Cancer Registry of China became funded by the Chinese Government, the coverage and data quality has steadily improved. These high-quality cancer statistics offer new insights to allocate health resources more reasonably and make greater contributions to narrow disparities across regions and populations.
Although the Chinese government is providing significant efforts to reduce China's cancer burdens, cancer remains a major health problem. The different burden in different areas and gender deepen the complexity and aggravate the difficulties for proper cancer control. More epidemiological data are required to accurately identify the trend change and geographical distribution characteristics of cancer incidence and mortality to provide better guidance for policy-makers to develop more timely strategies on cancer prevention and control.
ACKNOWLEDGMENTS
Not applicable.
AUTHORSHIP
Wanqing Chen and Maomao Cao designed the study and performed overall data interpretation. He Li and Dianqin Sun were responsible for writing and revising the manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The authors are accountable for all aspects of the work to ensure the accuracy or integrity of any part of the work. This article is not related to animals or human trial.
CONSENT FOR PUBLICATION
Not applicable.
CONFLICT OF INTEREST STATEMENT
No authors report any conflict of interest.
DATA AVAILABILITY
All data that is used in this article were extracted from previously public papers, which were provided clearly in references part.
FUNDING
This study is supported by CAMS Innovation Fund for Medical Sciences (2016-12 M-2-004), and Sanming Project of Medicine in Shenzhen (SZSM201911015).
REFERENCES
- 1 Data from America were extracted from Siegel R L, Miller K D, Jemal A. Cancer Statistics, 2020. CA Cancer J Clin, 2020, 70(1): 7-30.
- 2 Some columns may not total 100% due to rounding.




