Identification of the surgical indication line for the Denonvilliers’ fascia and its anatomy in patients with rectal cancer
Additional file: a representative surgical video of the identification of the Denonvilliers’ fascia
Abstract
Background
The high rate of urogenital dysfunction after traditional total mesorectal excision (TME) has caused doubts among scholars on the standard fashion of dissection. We have proposed the necessity to preserve the Denonvilliers’ fascia in patients with rectal cancer. However, how to accurately locate the Denonvilliers’ fascia is unclear. This study aimed to explore anatomical features of the Denonvilliers’ fascia by comparing autopsy findings and observations of surgical videos so as to propose a dissection method for the preservation of pelvic autonomic nerves during rectal cancer surgery.
Methods
Five adult male cadaver specimens were dissected, and surgical videos of 135 patients who underwent TME for mid-low rectal cancer between January 2009 and February 2019 were reviewed to identify and compare the structure of the Denonvilliers’ fascia.
Results
The monolayer structure of the Denonvilliers’ fascia was observed in 5 male cadaver specimens, and it was located between the rectum, the bottom of the bladder, the seminal vesicles, the vas deferens, and the prostate. The Denonvilliers’ fascia was originated from the rectovesical pouch (or rectum-uterus pouch), down to fuse caudally with the rectourethral muscle at the apex of the prostate, and fused to the lateral ligaments on both sides. The fascia was thinner on the midline with a thickness of 1.06 ± 0.10 mm. The crown shape of the Denonvilliers’ fascia was slightly triangular, with a height of approximately 5.42 ± 0.16 cm at midline. Nerves were more densely distributed in front of the Denonvilliers’ fascia than behind, especially on both sides of it. Under laparoscopic view, the Denonvilliers’ fascia was originated at the lowest point of the rectovesical pouch (or rectum-uterus pouch), with a thickened white line which was a good mark for identifying the Denonvilliers’ fascia.
Conclusion
Identification of the surgical indication line for the Denonvilliers’ fascia could help us identify the Denonvilliers’ fascia, and it would improve our ability to protect the pelvic autonomic function of patients undergoing TME for rectal cancer.
Abbreviations
-
- CRC
-
- colorectal cancer
-
- nNOS
-
- neuronal nitric oxide synthase
-
- TME
-
- Total mesorectal excision
1 BACKGROUND
Colorectal cancer (CRC) is a commonly diagnosed malignancy and leading cause of cancer death in the world. The CRC incidence in East Asia such as China, South Korea, Japan, and Singapore has surpassed the global average in recent decades, and the likelihood of rectal cancer incidence diagnosis increases in males [1]. Surgical resection is the most effective treatment measure for curing patients with rectal cancer [2]. Despite a series of studies on rectal cancer surgery with pelvic autonomic nerve preservation, the rate of postoperative urogenital dysfunction in patients with rectal cancer, especially in men, remains high, seriously affecting the patient's postoperative quality of life [3-5]. In 1982, Heald et al. [6] proposed the theory of total mesorectal excision (TME) as the gold standard surgery for rectal cancer. However, after traditional TME, the occurrence rate of urogenital dysfunction was still high [7-9]. The reason is that the surgery directly damages the pelvic autonomic nerves [10-12].
Because the pelvic autonomic nerve is thick in the retrorectal and lateral space, it is easy to be identified at this site in a TME surgery, especially under laparoscopy. However, the distribution of the pelvic autonomic nerves in front of the rectum is clump-like and difficult to identify, challenging the dissection of the anterior wall of the rectum. Laparoscopic rectal cancer surgery is widely performed [13-17]. Laparoscopy can magnify the field of surgical vision, but we do not know whether laparoscopy can help us better identify the distribution of the pelvic autonomic nerves in front of the rectum to maximize the preservation of these nerves under the premise of ensuring tumor resection.
It is difficult to assess sexual function in female patients, and there is much controversy about the origin of the Denonvilliers’ fascia. A series of our studies focuses on the male patients and male cadaver specimens. We have found that some pelvic autonomic nerves were closely related to Denonvilliers’ fascia and preservation of Denonvilliers’ fascia may have a better effect on the protection of urogenital function [18-21].
It is difficult for most scholars to locate the Denonvilliers' fascia. The specific aim of this study is to find how to accurately locate Denonvilliers' fascia by comparing autopsy findings and observations of surgical videos.
2 MATERIALS AND METHODS
2.1 Cadaver specimens
Five formalin-preserved pelvises from adult men who died naturally were provided by the Department of Human Anatomy, Histology and Embryology, Guangdong Pharmaceutical University (Guangzhou, Guangdong, China), following donation by their families.
2.2 Autopsy identification of the Denonvilliers’ fascia
TME was performed by incisively dissociating the rectum using the intermediate approach, pulling the rectum forward, dissecting the mesorectum along the retroperitoneum, continuing the dissection along the rectum intrinsic fascia, posteriorly entering the retrorectal space until reaching the pelvic floor. The left side of thin layered retroperitoneum was dissected and opened, reaching the back side, followed by dissecting through the anterior peritoneum, dissociating the bladder and the rectal preperitoneum until reaching the Douglas fossa and joining the top of the Denonvilliers’ fascia. The Denonvilliers’ fascia was dissociated between the seminal vesicle and the rectum to maintain its integrity.
Dissection was performed between the fascia propria of the rectum and the presacral fascia posteriorly in the retrorectal space that contains loose areolar tissue and is devoid of vessels and nerves, leaving the dense and tough tissue strips laterally, which are the lateral ligaments. The medial pelvis was divided into the left and right parts along the median sagittal plane, pulling the lateral rectum laterally, and the posterior lateral plexus was further dissociated to expose the hypogastric nerve to find the anatomical relationship between the Denonvilliers’ fascia and the lower abdomen. The start and end points of the Denonvilliers’ fascia were confirmed, the fascia was extracted, and the length of the fascia was measured and recorded.
2.3 Surgical video selection
We selected the cases with complete surgical videos of mid-low rectal cancer resection performed at The Third Affiliated Hospital of Sun Yat-sen University between January 1, 2009 and February 28, 2019. Inclusion criteria were as follows: patient's age between 18 and 75 years; tumor location within 12 cm from the anal verge; pathologic stage T1-2N0M0 classified according to the 7th edition of the American Joint Committee on Cancer (AJCC) TNM staging system; American Society of Anesthesiology function class I-III; and R0 resection. The exclusion criteria were as follows: emergency surgery; preoperative urogenital dysfunction; preoperative major pelvic surgery; or local excision.
The main equipment for TME included an Olympus Laparoscopy System (Shinjuku-ku, Tokyo, Japan) and Stoze Full HD Laparoscopy System (Tuttlingen, Germany), Harmonic Ultrasonic Knives (Johnson & Johnson, New Brunswick, NJ, USA), vernier calipers (accurate to 0.01 mm; Johnson & Johnson), and conventional surgical instruments. All were performed by the same group of surgeons. The study was approved by the Ethics Committee of the Third Affiliated Hospital of Sun Yat-sen University (No. [2015]2-125). Written informed consent was obtained from all patients.
2.4 Surgical video observation
Combining the autopsy results, mainly focusing on the membranous structure in front of the rectum and its connective tissue bundles, the lateral ligaments and the middle rectal artery were identified and confirmed. The anatomical structural differences between the cadaver and the living body were identified.
3 RESULTS
3.1 Clinicopathologic characteristics
We have collected 135 cases with complete surgical videos of mid-low rectal cancer resection. The patients in this group were all male, with a median age of 58 (range, 21-71) years. The Department of Human Anatomy, Histology and Embryology, Guangdong Pharmaceutical University had provided 5 cadaver specimens. The median age of the 5 men at the time of death was 83 (range, 71-95) years.
3.2 The Denonvilliers’ fascia identified in male cadaver specimens
The Denonvilliers’ fascia was found in all 5 cadaver specimens. This structure extended from the level of the seminal vesicle posterolaterally to the presacral fascia, down to fuse caudally with the rectourethral muscle at the apex of the prostate (Figure 1). This structure separated the space between the mesorectum and the posterior wall of the pelvic organs into two spaces. Both spaces were avascular and loose around the midline.
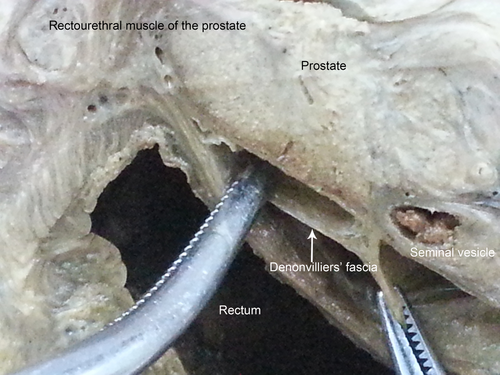
The Denonvilliers’ fascia was found caudal to the peritoneal reflection at the rectovesical pouch and fused to the lateral ligaments on both sides. The fascia was thinner on the midline and with a thickness of 1.06 ± 0.10 mm. The fascia gradually became a relatively dense film from the middle to the side. The crown shape of the Denonvilliers’ fascia was slightly triangular, with a height of approximately 5.42 ± 0.16 cm at the midline. In the 5 cadaver specimens, the fascia was a monolayer structure that was easily identifiable. There was no change in the thickness of the fascia due to fixation with formalin because its main ingredient is fiber.
3.3 The Denonvilliers’ fascia observed on videos of rectal cancer surgery
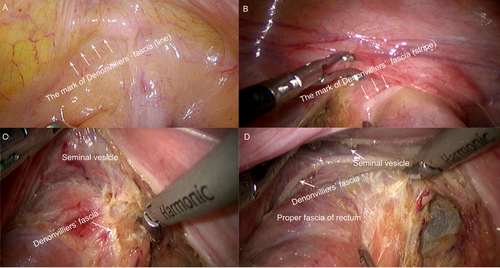
The Denonvilliers’ fascia was originated at the lowest point of the rectovesical pouch (or the rectum-uterus pouch), as viewed laparoscopically as a thickened white line (Figure 2A) or stripe (Figure 2B) (Additional file: surgical video). This was the surgical indication line. Thickened white lines/stripes were observed on all 135 videos. They went along laterally to the junction of the mesorectum and the retroperitoneum, where a “yellow-white line” appeared. The thickened white line was a good mark for identifying the Denonvilliers’ fascia. An incision was made in front of this line, and dissection was performed in front of the Denonvilliers' fascia (Figure 2C); continuing the incision forward would allow us to visibly see a thin envelope that encapsulates the seminal vesicles and the prostate. Another incision was made behind this line, and dissection was performed behind the Denonvilliers' fascia to ensure its preservation (Figure 2D). There was also a rectal intrinsic fascia that completely enveloped the mesorectum (Figurte 2D). As shown on the 135 videos, the dissections were made in front of the Denonvilliers’ fascia in 73 (54.1%) patients and behind the Denonvilliers’ fascia in 62 (45.9%) patients. In the patients with dissections made in front of the Denonvilliers’ fascia, a ‘U’ shaped incision was made through this fascia, whereas the lower part of Denonvilliers’ fascia were preserved, and returned to the rear of this fascia. This ‘U’ shape incision made on Denonvilliers' fascia was a very popular practice. After the dissection either in front of or behind the white line, a fine and thin layer of the Denonvilliers’ fascia remained, and a very dense tissue structure was encountered, which is the stopping point of the lower part of the Denonvilliers’ fascia. The hypogastric nerve could be identified in 12 patients on surgical video.
3.4 Identifying the lateral ligaments in male cadaver specimens
There was a fused area that formed a screen-shaped structure, applying medial traction to the rectum. The fused area was the lateral ligaments.
The inferior hypogastric plexus was located on both sides of the rectum and was a continuation of the hypogastric nerve (Figure 3). The inferior hypogastric plexus contained parasympathetic fibers from the pelvic splanchnic nerves (S2, 3 and 4), and sympathetic fibers from the sacral sympathetic trunks. The plexus runs along the pelvic sidewall, with a quadrangular reticular structure located slightly below the peritoneum, covering 1/3 of the outer side of the rectum and the posterolateral side of the prostate and seminal vesicles.

The branches of the inferior hypogastric plexus were mainly distributed in the rectum and urogenital organs. A small branch of the inferior hypogastric plexus that gives rise to the rectal plexus constitutes the lateral ligaments. The side of the Denonvilliers’ fascia terminates in the lateral ligaments, and the lower ventral plexus distributes in the branch of the urogenital organs, and the small branches of the middle rectum are located in the lateral front of the fascia (Figure 3).
3.5 Identifying the lateral ligaments on videos of rectal cancer surgery
The lateral structure of the Denonvilliers’ fascia was not observed during laparoscopic surgery. Hemorrhage occurred easily at the anterior lateral side of the mesorectum at the low segment in 5 (3.7%) patients. There are 12 (8.9%) patients could be identified with the hypogastric nerve from surgical video.
4 DISCUSSION
There weren't controversies regarding the separation of the posterior and lateral rectal walls. The correct plane for separation of the posterior and lateral rectal walls was avascular in most cases except where it was crossed by the lateral ligaments. By pursuing the lipoma-like outer surface of the mesorectum, the autonomic nerve plexuses could be preserved [6]. The lateral ligaments could simply be cut by Harmonic Ultrasonic Knives. However, the distribution of the pelvic autonomic nerves in the anterior rectal wall is complicated and difficult to recognize. Therefore, there are still many controversies about the separation of the anterior rectal wall [22].
The TME theory proposed by Heald et al. [6] has become the new gold standard for rectal cancer surgery: the rectum and its mesentery are removed as a complete anatomical structure while preserving the pelvic autonomic nerves as much as possible. Heald et al. [23] believe that the Denonvilliers’ fascia is the front boundary of the rectal intrinsic fascia and acts as a barrier to rectal cancer. Therefore, TME should be performed in front of the Denonvilliers' fascia to completely remove the mesorectum so that no residual tumor is left. This operative procedure is widely accepted all over the world [24, 25].
According to our anatomical observations, the Denonvilliers' fascia terminates at the lateral ligaments, which present as constant, dense connective bundles that are located on the lateral sides of the lower part of the rectum and extend between the rectal visceral fascia and pelvic parietal fascia, above the levator ani. The lateral ligaments constitute the inferior hypogastric plexus that gives rise to the rectal plexus, extends toward the rectum and the vessels from the lower part of the rectum toward the iliac lymph nodes. A small branch of the internal pudendal artery lies in front of the fascia, and nerve fibers from the lateral ligaments form a neurovascular bundle in the anterolateral side of the Denonvilliers’ fascia. The components of the inferior hypogastric plexus include some parasympathetic nerves and are closely related to urogenital function [26-28].
If the dissection is performed behind the Denonvilliers' fascia, it would damage the rectal intrinsic fascia, destroy the mesangial tissue, and affect radical tumor resection. If the dissection is performed in front of the Denonvilliers' fascia, well-defined, bead-like plump seminal vesicles and the prostate could be located. However, if a slight inadvertent injury to the neurovascular bundle occurs in the anterolateral side of the Denonvilliers’ fascia, the visual field would be stained by blood, and the anatomical structures would be unclear, resulting in damage to the parasympathetic corpus cavernosum. Additionally, it is easy to damage the parasympathetic corpus cavernosum from the pelvic plexus in front of the Denonvilliers’ fascia, which plays an important compensatory role in the damage of the pelvic wall and cause urogenital dysfunction [25]. We believe that the preservation of the Denonvilliers’ fascia is of great significance in reducing the rate of postoperative urogenital dysfunction in rectal cancer patients [26-28], which is supported by the results from other studies [29-31].
In clinical practice, most surgeons are unable to accurately identify the Denonvilliers’ fascia, leading to the destruction of the Denonvilliers’ fascia and damage to the pelvic autonomic nerves. At present, a popular practice is to incise the rectovesical pouch (or rectum-uterus pouch) at the point of 1 cm above the peritoneal reflection. It would enter the surgical plane in front of the Denonvilliers' fascia and then separates in the loose space in front of the Denonvilliers' fascia. This process coincides with the modified “U”-shaped resection of the Denonvilliers’ fascia proposed by Heald et al. [23]. Although this method preserves the anterolateral side of the Denonvilliers’ fascia to avoid damage to the inferior hypogastric plexus, it still damages the ramus communicans in front of the Denonvilliers' fascia and damages the pelvic autonomic nerves. Our clinical observations showed that this method did not cause significant sexual dysfunction.
We combined cadaver dissection with surgical video observations and found that the Denonvilliers’ fascia was originated at the rectovesical pouch (or rectum-uterus pouch), presenting as a thickened white strip/line. The thickened white line is a good mark for identifying the Denonvilliers' fascia. Our results indicate that if a dissection is made in front of the white line, the ramus communicans in front of the Denonvilliers' fascia would be damaged. However, if a dissection is performed behind the white line, damages to the inferior hypogastric plexus and the ramus communicans in front of the Denonvilliers' fascia could be avoided.
5 CONCLUSIONS
The Denonvilliers' fascia can be completely removed by dissection in front of the white line in the peritoneal reflection, if the tumor located in the anterior rectal wall or the tumor had invaded the rectal anterior membrane. For tumors located in the posterior wall of the rectum, Denonvilliers’ fascia could be reserved by dissociation behind the white line, avoiding excessive damage to the pelvic plexus, protecting urogenital function and improving the quality of life of patients.
AUTHORS’ CONTRIBUTIONS
Jianglong Huang and Jiafeng Fang collected the data, and drafted the manuscript; Jing Liu provided and dissected the cadaver specimens and revised the paper; Zongheng Zeng, Bo Wei and Tufeng Chen assisted in design the study and analyzed the data; Hongbo Wei revised the manuscript critically for important intellectual content and was responsible for article quality control. All authors read and approved the final manuscript.
ACKNOWLEDGEMENTS
Not applicable
COMPETING INTERESTS
The authors declare that they have no competing interests
AVAILABILITY OF DATA AND MATERIALS
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
CONSENT FOR PUBLICATION
Not applicable.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Ethics Committee of the Third Affiliated Hospital of Sun Yat-sen University (Guangzhou, China).
FUNDING
This study was supported by the Sun Yat-sen University clinical research 5010 program (2016Y9031).




