The inferior gluteal nerve often has a cutaneous branch: A discovery with application to hip surgery and targeting gluteal pain syndromes
Abstract
The inferior gluteal nerve has been traditionally described as a solely motor branch innervating the gluteus maximus. However, during routine dissection of the gluteal region, a cutaneous branch of the inferior gluteal nerve was identified. As the gluteal region is vulnerable to the development of pressure ulcers and iatrogenic injury with for example, surgical approaches and injection therapies, a comprehensive understanding of its cutaneous innervation is important. Therefore, the aim of this study was to elucidate the anatomy of this cutaneous branch of the inferior gluteal nerve in a series of cadavers. Twelve sides from six fresh-frozen cadaveric specimens were dissected. When a cutaneous branch was identified piercing the gluteus maximus, its origin from the inferior gluteal nerve was verified and the diameter and length of it measured. Additionally, for localization, the distance from the midline to the exit point of the cutaneous branch from the gluteus maximus was measured. One to two cutaneous branches were identified as arising from the inferior gluteal nerve on nine sides (75%). The branch(es) were usually located in the lower outer quadrant of the gluteus maximus. These branches had a mean distance of 12.5 cm from the midline. Their mean diameter and length was 0.7 mm and 28.6 cm, respectively. On all sides with a cutaneous branch of the inferior gluteal nerve, the skin over the posterior aspect of the greater trochanter was innervated by superior and inferior cluneal nerves and supplemented by cutaneous branch(es) of the inferior gluteal nerve. Side or sex was not a predictor of the presence of a cutaneous branch of the inferior gluteal nerve. To our knowledge, a cutaneous branch derived from the inferior gluteal nerve has not been previously described. Based on our cadaveric findings, the majority of individuals will have the area of skin over the greater trochanter innervated by this nerve. Therefore, surgeons and pain specialists should be aware of its presence and might develop surgical procedures that help avoid it or develop technical advances that target it for various pain syndromes in this area. We propose naming these cutaneous branches the lateral cluneal nerves, which would necessitate renaming the middle cluneal nerves to medial cluneal nerves. Clin. Anat. 31:937–941, 2018. © 2018 Wiley Periodicals, Inc.
INTRODUCTION
The inferior gluteal nerve usually arises from the ventral rami of the fifth lumbar and first and second sacral spinal nerves. It leaves the pelvis via the greater sciatic foramen inferior to the piriformis and divides into branches which pass posteriorly into the deep surface of the gluteus maximus (Standring, 2016). The inferior gluteal nerve is vulnerable to iatrogenic injury during posterior and posterolateral approaches to the hip (Schumm et al., 1975; Abitbol et al., 1990; Ling and Kumar, 2006; Apaydin et al., 2009). The posterior approach is the most common and practical of those used to expose the hip joint. Moreover, the posterior approaches allow excellent visualization of the femoral shaft, thus are popular for revision joint replacement surgery in cases in which the femoral component needs to be replaced (Crenshaw, 1987; Hoppenfeld et al., 2009).
Both superior and inferior gluteal nerve entrapment syndromes have been described (Rask, 1980; Pećina et al., 1997). Even though these nerves have not been described as having a cutaneous distribution, some authors have found tenderness over the greater sciatic foramen in patients with entrapment of them and have suggested instilling anesthetic at the point of entrapment for pain control (Rask, 1980). Additionally, as the gluteal region is vulnerable to the development of pressure ulcers, the loss of sensitivity in this region could predispose one to the development of such ulcers (van Vliet et al., 1993). Additionally, posterior approaches to the hip can severe such cutaneous branches and thus lead to sensory loss or neuropathies.
During routine dissection of the gluteal region, a cutaneous branch of the inferior gluteal nerve was identified. As the gluteal region is vulnerable to iatrogenic nerve injury, a comprehensive understanding of its cutaneous innervation is important. Therefore, the aim of this study was to elucidate the anatomy of this cutaneous branch of the inferior gluteal nerve in a series of cadavers.
MATERIALS AND METHODS
In the prone position, 12 gluteal regions from six fresh-frozen adult cadaveric specimens were dissected. Three specimens were male and three were female. The mean age at death was 74 years (range, 54–90 years). When a cutaneous branch was identified piercing the gluteus maximus and supplying the overlying skin, its origin from the inferior gluteal nerve was verified and the diameter and length of it measured. Additionally, for localization, the distance from the midline to the exit point of the cutaneous branch from the gluteus maximus was measured. All measurements were made with microcalipers (Mitutoyo, Kanagawa, Japan) with a resolution of 0.01 mm and an accuracy of ±0.025 mm. When necessary, either 2.5 loupe magnification or a surgical microscope (OPMI CS NC31, Carl Zeiss, Oberkochen, Germany) was used for dissections. Statistical analysis of measurements/presence between sides and sex was performed with significance set at P < 0.05. Anatomical ethical and scientific guidelines were followed for this study (Tomaszewski et al., 2017; Henry et al., 2018).
RESULTS
One to two cutaneous (two branches were found on three sides) branches were identified as arising from the inferior gluteal nerve on nine sides (75%) (Figs. 1-3). The branch(es) were usually (89%) (one left side (11%) was found to have a cutaneous branch in the upper outer quadrant) located in the lower outer quadrant of the gluteus maximus and all traveled in an inferosuperior or inferolateral direction. These branches had a mean distance of 12.5 cm (range 9.5–14.5 cm) from the midline where they left the deep surface of the gluteus maximus to travel subcutaneously to the skin overlying this muscle. Their mean diameter and length (from exit from the gluteus maximus to termination in the skin) were 0.7 mm and 28.6 cm, respectively. On all sides with a cutaneous branch of the inferior gluteal nerve, the skin over the posterior aspect of the greater trochanter was innervated by superior and inferior cluneal nerves and supplemented by cutaneous branches of the inferior gluteal nerve (Fig. 4). All cutaneous branches of the inferior gluteal nerve arose from branches of the nerve that had already innervated the gluteus maximus muscle. Side or sex was not a predictor of the presence, size or length of a cutaneous branch of the inferior gluteal nerve (P > 0.05). No anatomical variations were noted on any side where cutaneous branches of the inferior gluteal nerve were identified. No specimen had signs of previous surgery to the gluteal region.
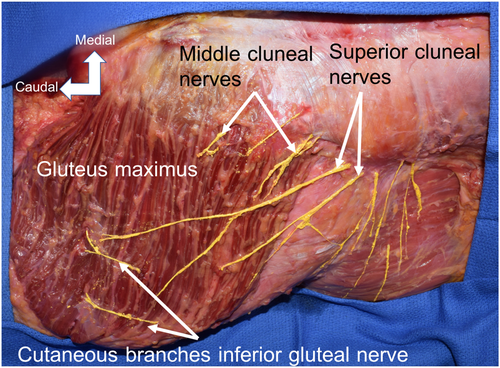
Right cadaveric gluteal region. For reference, the iliac crest is outlined. Note the cutaneous branches of the inferior gluteal nerve. Nerve branches are colored yellow for clarity. [Color figure can be viewed at wileyonlinelibrary.com]
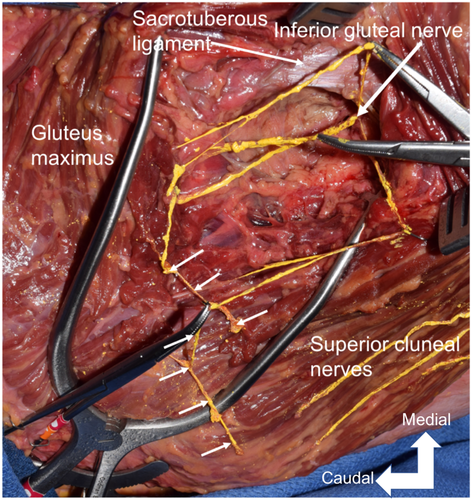
Deeper dissection of the cutaneous branches of the inferior gluteal nerve as seen in Figure 1. Note the three branches of the inferior gluteal nerve with the medial and lateral branches terminating as cutaneous branches at the white arrows. [Color figure can be viewed at wileyonlinelibrary.com]
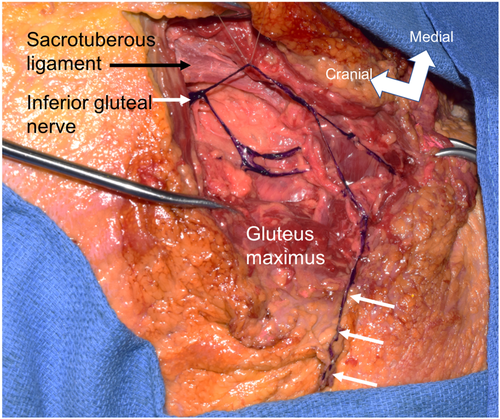
Left cadaveric gluteal region noting a terminal cutaneous branch (arrows) of the inferior gluteal nerve. Nerves are colored purple for clarity. [Color figure can be viewed at wileyonlinelibrary.com]
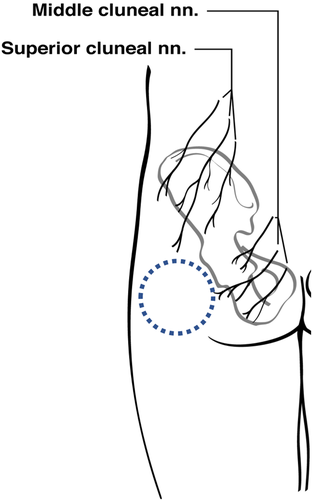
Schematic drawing of the left gluteal region and general region (blue dotted circle) where the cutaneous branches of the inferior gluteal nerve were identified. [Color figure can be viewed at wileyonlinelibrary.com]
DISCUSSION
We identified cutaneous branches of the inferior gluteal nerve on the majority (75%) of cadaveric sides (Figs. 1-3). These were always very small (mean diameter of 0.7 mm) and delicate branches and thus could be easily overlooked with routine dissection of the gluteal area. In fact, due to their size, smaller branches could have been missed during dissections. Therefore, the incidence might be greater than found in our initial study. Additionally, when such branches were identified, they were always terminal branches of muscular branches of the inferior gluteal nerve and did not arise directly from this nerve.
Isolated injury to the inferior gluteal nerve is rare. However, the nerve is vulnerable to injury with pelvic/hip fractures, and intramuscular injections (Pećina et al., 1997). Parenthetically, Farrell et al. (2005) concluded that for posterior approaches to the hip resulting in motor nerve palsies, either complete or incomplete, the majority of patients will not have resolution.
Nerve Injury Following Hip Surgery
Injuries to regional peripheral nerves occur in 0.5%–8% of patients following insertion of a prosthetic hip (Solheim and Hagen, 1980; Abitbol et al. 1990; Nercessian et al. 1994). Sciatic nerve palsy after total hip replacement is the most common nerve injury followed by injury to the femoral nerve (Dietze et al. 2014). Although previous studies regarding nerve injury following posterior approaches to the hip have focused on injury to the superior gluteal, femoral, obturator, and sciatic nerves (Weber et al. 1976; Solheim and Hagen 1980; Johanson et al. 1983; Duparc et al. 1997; Patil and Friedman, 2005; Hurd et al. 2006; Ince et al. 2007), the inferior gluteal nerve is also at risk (Ling and Kumar, 2006) with such procedures. However, the incidence of inferior gluteal nerve injury after posterior surgical approaches to the hip is still uncertain (Abitbol et al. 1990). Abitbol et al. (1990) reported superior or inferior gluteal nerve injuries in 78% of patients undergoing a lateral approach for hip arthroplasty. In another 10 patients who underwent posterior approaches, postoperative electromyographic results for the gluteus maximus were abnormal. Although the posterior approach has been reported to be the most commonly used approach for hip replacement, it is the approach most likely to be associated with damage to the inferior gluteal nerve (Ling and Kumar, 2006).
Topography of the Inferior Gluteal Nerve and Its Cutaneous Branch
Ling and Kumar (2006) depicted the inferior gluteal nerve as entering the deep surface of the gluteus maximus medial to the greater trochanter of the femur and posterior to the proximal part of its neck. Apaydin et al. (2009) studied 36 cadaveric inferior gluteal nerves and created an imaginary triangle formed by connecting the greater trochanter, ischial tuberosity, and posterior inferior iliac spine. They found that the upper one half of such a triangle was effectively a danger zone for injuring the inferior gluteal nerve. They also found that the inferior gluteal nerve entered the deep surface of the gluteus maximus ∼5 cm from the apex of the greater trochanter. Based on their study, dividing the gluteus maximus with standard techniques may damage the inferior gluteal nerve and thus would also endanger this nerve's cutaneous branches as found in this study.
In the classical posterior approach, the gluteus maximus is split by a 10–15 cm curved incision centered on the posterior aspect of the greater trochanter. The part of the incision that runs from 6 to 8 cm above and posterior to the greater trochanter is in line with the fibers of the gluteus maximus which is split by blunt dissection and retracted (Crenshaw, 1987). Deep surgical dissection necessitates detaching the muscle close to its insertion and reflecting it posteriorly. In this study, the cutaneous branches of the inferior gluteal nerve were usually located in the lower outer quadrant of the gluteus maximus and traveled in an inferosuperior or inferolateral direction. These branches had a mean distance of 12.5 cm from the midline and an average length of 28.6 cm and thus, would be endangered during posterior approaches to the hip.
CONCLUSIONS
To our knowledge, a cutaneous branch derived from the inferior gluteal nerve has not been previously described. Most cadavers in our study had an area of skin over the greater trochanter innervated by this nerve. Therefore, surgeons and pain specialists should be aware of its presence and might develop surgical procedures that help avoid it or develop technical advances that target it for various pain syndromes in this area. We would propose naming these cutaneous branches the lateral cluneal nerves, which would necessitate renaming the middle cluneal nerves to medial cluneal nerves.