Observed Prevalence of Congenital Situs Inversus in the United States Before and During the SARS-CoV-2 Pandemic, 2017–2022
Funding: The authors received no specific funding for this work.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. This report is U.S. government work with no additional outside funding.
An abstract summarizing this report was presented as a poster at the 45th Annual David W Smith Workshop on Malformations and Morphogenesis, August 16–21, 2024.
ABSTRACT
Background
Reports from China describe an increase in the frequency of fetal situs inversus in 2023 after the country's “zero-Covid” policy was lifted, suggesting an association with maternal SARS-CoV-2 infection. However, a report of birth defects surveillance data from Scandinavia observed no sustained increase during the SARS-CoV-2 pandemic (2020–2022 vs. 2018–2019). We examined birth defects surveillance data to assess any increase in situs inversus in the U.S. during the SARS-CoV-2 pandemic.
Methods
We combined data from four population-based birth defects programs in Massachusetts, Minnesota, North Carolina, and Atlanta, Georgia, to compare the prevalence of situs inversus among infants and fetuses delivered before (2017–2019) and during (2021–2022) the SARS-CoV-2 pandemic. We defined situs inversus as mirror-image transposition of the heart and/or other organs, or primary ciliary dyskinesis with situs inversus, excluding isolated dextrocardia. The programs varied in the pregnancy outcomes included (live births ± non-live births); all included both prenatal and postnatal diagnoses.
Results
We identified 294 infants and fetuses with situs inversus (6.8% non-live births). We estimated the combined prevalence per 10,000 live births as 1.72 during the pandemic versus 1.71 before the pandemic (OR = 1.005; 95% CI: 0.778–1.297). The estimated annual prevalence ranged from 1.41 in 2017 to 2.21 in 2019 with no significant trend across the study period (p = 0.39).
Conclusions
We did not observe an increase in situs inversus during the SARS-CoV-2 pandemic. Because information about SARS-CoV-2 infection among individual pregnancies was not available from all programs, we could not assess a specific association with maternal infection.
1 Background
Situs inversus is a congenital condition with mirror-image left–right transposition of organs. It can involve the heart alone, the heart and other thoracic organs (e.g., lungs), abdominal organs alone, or both thoracic and abdominal organs. Some instances are associated with primary ciliary dyskinesia. It is estimated to affect approximately 1 in 10,000 births (Eitler, Bibok, and Telkes 2022). A report from China has described an abrupt four-fold increase in the frequency of fetal situs inversus (total situs inversus with dextrocardia or partial situs inversus with levocardia) diagnosed by ultrasonography at 20 to 24 weeks gestation in April–June 2023, compared with data from 2014 to 2022 (Wang et al. 2023). The authors note that this increase followed the lifting of China's “Zero-COVID” policies after which it is estimated approximately 82% of the population experienced SARS-CoV-2 infection over the subsequent 2 months (Fu et al. 2023). A second report from another prenatal care center in China documented a significant increase in the diagnosis of fetal situs inversus among mothers who had SARS-CoV-2 infection during early pregnancy in January–May 2023, following the liberalization of SARS-CoV-2 prevention and control policies compared with mothers who did not have infection (odds ratio 8.2; 95% CI: 2.5–27.4) (Qiu et al. 2024). A third report from three other hospitals in China examined the records of women who had undergone prenatal ultrasound and found an 8- to 20-fold higher incidence of situs inversus in the period following lifting of the pandemic control measures (January–April 2023) compared with the period before the pandemic (January–April 2019) and during the pandemic control measures (January–April 2022) (Xu et al. 2024). Most recently, a follow-up study to the initial report by Wang et al. examined the timing of SARS-CoV-2 infection in relation to the frequency of fetal situs inversus. Using a matched case–control study design, they estimated an odds ratio of 6.54 (95% CI: 1.76–24.34) for SARS-CoV-2 infection at four to six weeks gestation, but no increase for infection at other gestational ages (gestation weeks 1 to 3, 7 to 12, or 13 to 40) (Guo et al. 2024). In contrast, a report from Sweden, Denmark, and Norway observed no sustained increase in the prevalence of situs inversus during 2020–2022, the years of the SARS-CoV-2 pandemic in those countries, compared with the prevalence in 2018–2019 (Ludvigsson et al. 2024).
In light of these findings, we questioned whether an increase in situs inversus occurred in the United States during the SARS-CoV-2 pandemic. We examined the prevalence of congenital situs inversus from four birth defects surveillance programs in the U.S. before and during the SARS-CoV-2 pandemic. In the U.S., SARS-CoV-2 infection became widespread in Spring 2020, and continued throughout 2021 and 2022, with the dominant variant changing over time (CoVariants. 2024).
2 Methods
We combined data from population-based birth defects surveillance programs in four U.S. jurisdictions (statewide data from Massachusetts, Minnesota, and North Carolina, and local data from metropolitan Atlanta, Georgia) to estimate the prevalence of situs inversus among infants and fetuses delivered from 2017 to 2022, which includes the period before and during the SARS-CoV-2 pandemic. These programs were chosen because their methods were well-established before the SARS-CoV-2 pandemic, they directly abstract medical records to identify birth defects through at least 1 year of age, and they have near-complete data available on situs inversus for births through 2022. Details of the programs have been described more fully elsewhere (National Birth Defects Prevention Network 2024). In general, diagnoses of major congenital malformations and chromosome anomalies were ascertained through review and abstraction of medical records at birth and pediatric hospitals along with subspecialty and prenatal clinics. Three of the programs included live births, stillbirths of at least 20 weeks gestation, and pregnancies electively terminated after prenatal diagnosis of situs inversus at any gestational age. One of these three programs also included fetal losses due to spontaneous abortion before 20 weeks of gestation with these defects. The fourth program only included live births with these defects.
We defined situs inversus as mirror-image transposition of the heart and/or other organs in the thorax, abdomen, or unspecified location, or a diagnosis of primary ciliary dyskinesis with situs inversus (Kartagener syndrome). We excluded those with isolated dextrocardia without other associated defects because of the potential for misclassification with dextroposition of the heart. Both prenatal and postnatal diagnoses were included when the description from imaging or other procedures was definitive. We estimated the crude prevalence of situs inversus in all pregnancy outcomes per 10,000 live births by year of delivery.
3 Results
Due to the rarity of situs inversus in the general population and resulting variability in the annual prevalence in each jurisdiction, data from the four jurisdictions were combined for analysis. The annual prevalence among the jurisdictions ranged from 0.85 per 10,000 to 3.54 per 10,000 live births. No one program had consistently higher prevalence than the others across the years examined (data not shown).
The four jurisdictions represent a combined total population of 1.71 million live births. The contribution of each jurisdiction ranged from 17% to 40% of the total cases and from 12% to 42% of the total denominator. Assuming a baseline prevalence of one case of situs inversus per 10,000 live births, our surveillance cohort could detect a 1.3-fold increase in situs inversus with 95% power with α = 0.05. We identified 294 infants and fetuses with situs inversus from these jurisdictions, 20 of which were non-live births (6.8%; range per program 6%–12%).
The combined prevalence of situs inversus per 10,000 live births by year of delivery is shown in Table 1 and Figure 1. The symbols in Figure 1 represent the highest and lowest prevalence among the four jurisdictions each year. The combined prevalence of situs inversus for the entire period (2017–2022) was 1.72 per 10,000 live births. The estimated prevalence was 1.72 in 2021–2022 during the SARS-CoV-2 pandemic and 1.71 in 2017–2019 prior to the pandemic (OR = 1.005; 95% CI: 0.778–1.297). The estimated combined annual prevalence ranged from a minimum of 1.41 in 2017 to a maximum of 2.21 in 2019. Notably, the prevalence did not appear to increase during the years of the SARS-CoV-2 pandemic (chi-square for trend = 0.74; p = 0.39).
| Year of delivery | Denominator (live births) | Cases | Estimated prevalence (per 10,000 live births) | (95% CI) |
|---|---|---|---|---|
| 2017 | 291,711 | 41 | 1.41 | 0.96–1.85 |
| 2018 | 286,844 | 44 | 1.53 | 1.06–2.00 |
| 2019 | 285,262 | 63 | 2.21 | 1.65–2.77 |
| 2020 | 277,088 | 48 | 1.73 | 1.22–2.24 |
| 2021 | 284,462 | 48 | 1.69 | 1.19–2.18 |
| 2022 | 284,876 | 50 | 1.76 | 1.25–2.26 |
| Total | 1,710,243 | 294 | 1.72 | 1.50–1.89 |
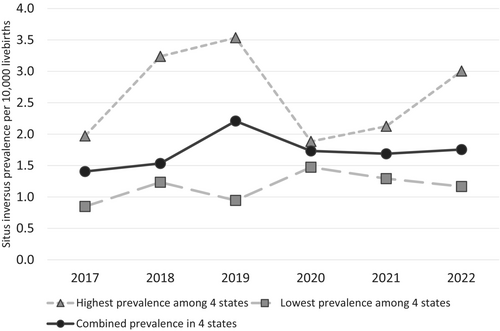
In addition, no consistent trend in the prevalence for any of the individual jurisdictions was observed (data not shown).
4 Discussion
Data from four U.S. jurisdictions do not support an observed increase in the frequency of situs inversus associated with the SARS-CoV-2 pandemic. The observed prevalence of this condition in the included jurisdictions did not appear to increase following widespread circulation of the virus.
The contrast of this finding to the marked increase observed in China could be due to several factors. SARS-CoV-2 infection spread abruptly in China after restrictions were lifted, and it is estimated that the majority of the population was infected within 2 months (Fu et al. 2023). Assuming that infection spread equally throughout the population, this would have resulted in the majority of women in the early weeks of pregnancy being infected in a very short time. In comparison, SARS-CoV-2 infection in the U.S. spread more slowly and was sustained over a prolonged period with several distinct waves resulting from circulation of different variants of the virus (CoVariants 2024). If situs inversus was associated with maternal SARS-CoV-2 infection in the United States, the earliest affected deliveries would have been expected in late 2020 or early 2021 and presumably would have remained increased throughout 2021 and 2022. Prevention measures recommended in the U.S. throughout the pandemic may have resulted in a much smaller proportion of women being exposed early in pregnancy. In addition, cases in the China data were uniformly identified by second trimester prenatal ultrasound while those in the U.S. data were identified by a combination of prenatal and postnatal diagnostic findings. And, while SARS-CoV-2 infection in China was primarily due to the omicron variant, infections in the U.S. resulted from different variants circulating at different times.
Our analysis has some specific limitations. Information about SARS-CoV-2 infections among individual pregnancies was not available from all participating birth defects surveillance programs. Therefore, a direct association with maternal infection could not be assessed. In addition, the participating birth defects surveillance programs varied in their inclusion of non-live births and the gestational age at which they were included. This might have resulted in an underestimate of the true prevalence of situs inversus. However, only one program did not include non-live births at all and only 6.8% of situs inversus deliveries were non-live births. We do not expect the partial exclusion of non-live births to have substantially affected the prevalence estimates. Finally, while pregnancy care in the U.S. shifted to increased use of telemedicine during the pandemic, it has been documented that use of critical in-person services, such as mid-trimester fetal anatomical ultrasound, continued at frequencies comparable to before the pandemic (Kern-Goldberger et al. 2023). However, instances of asymptomatic total situs inversus that were not prenatally diagnosed may have been missed both before and during the pandemic.
Our analysis also has some specific strengths. Our data are from population-based surveillance programs which likely limits the potential for referral or other reporting bias. In addition, the majority of situs inversus diagnoses in our data were confirmed postnatally among liveborn infants which likely limits potential misclassification of the outcome. And, while data collection by the programs was somewhat delayed during the SARS-CoV-2 pandemic, there was limited reassignment of surveillance staff to other duties. The data sources and access to case information did not change for these programs. We do not feel these factors resulted in substantial under-ascertainment of situs inversus cases compared to before the pandemic.
Multiple genetic and environmental factors have been associated with situs abnormalities in humans, but a full understanding of the underlying cellular and molecular processes that result in asymmetry is lacking (Eitler et al. 2022). Although infrequently identified, transplacental transmission of SARS-CoV-2 from mother to fetus during pregnancy has been documented (Vivanti et al. 2020; Allotey et al. 2024); however, situs determination occurs in the early embryo prior to establishment of a fully functioning placenta (Turco and Moffett 2019). The report of a temporal association between SARS-CoV2 infection in early pregnancy and situs inversus in offspring by Guo et al. would benefit from replication and further exploration of the possible mechanisms. Our data from four population-based surveillance programs from the time period of the SARS-CoV2 pandemic as it occurred in the United States with multiple variants over a longer period of time make it unlikely that U.S. data can be used to conduct that replication.
Author Contributions
Janet D. Cragan: conceptualization, formal analysis, methodology, writing – original draft. Sook-Ja Cho: data curation, formal analysis, writing – review and editing. Nina Forestieri: data curation, formal analysis, writing – review and editing. Michele Hort: data curation, formal analysis, writing – review and editing. Eirini Nestoridi: data curation, formal analysis, writing – review and editing. Cynthia A. Moore: conceptualization, methodology, writing – review and editing. Erin Stallings: validation, writing – review and editing. Elizabeth B. Gray: conceptualization, methodology, writing – review and editing. Jennita Reefhuis: conceptualization, methodology, visualization, writing – review and editing.
Open Research
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.