Continuous positive airway pressure treatment from the prehospital field in a Japanese regional Doctor Car system
Abstract
Background
Continuous positive airway pressure (CPAP) therapy is an effective treatment for patients with severe heart failure, and certain guidelines recommend its early initiation. However, the current Japanese law strictly prohibits paramedics from administering this treatment. To demonstrate the efficacy and safety of prehospital administration of CPAP therapy, this study was conducted by the Yokohama Medical Control Council (Yokohama MC).
Methods
The Yokohama MC established a protocol for CPAP treatment and dispatched Doctor Cars to attend to patients with severe respiratory failure. The Boussignac CPAP system was installed in all Yokohama Doctor Cars, including Workstation-type Doctor Cars and Hospital-type Doctor Cars. Data from this study were collected and recorded in the Yokohama City Doctor Car Registry system from October 2020 to January 2022.
Results
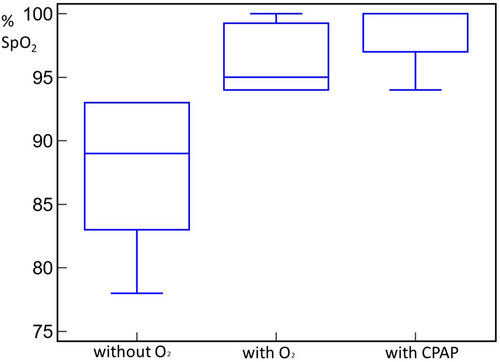
The Doctor Car was dispatched 661 times, and CPAP therapy was administered to 13 patients in the prehospital field. It is important to note that the number of CPAP cases was lower than anticipated due to the coronavirus disease 2019 (COVID-19) pandemic, given concerns about aerosol production. When assessing changes over time in oxygen saturation (SpO2), the median (interquartile range), excluding missing values, was 89% (83%–93%) without oxygen, 95% (94%–99.3%) with oxygen, and 100% (97%–100%) with CPAP. The differences between these groups were statistically significant with a p-value of <0.0001. Respiratory distress was primarily attributed to heart failure in 10 patients (91%) and pneumothorax in 1 patient (9%). Notably, none of the patients’ conditions worsened after the use of CPAP.
Conclusion
We have detailed the administration of CPAP therapy in the prehospital field within a local city in Japan. To the best of our knowledge, this represents the inaugural report of a prospective observational study on the prehospital administration of CPAP therapy originating from Japan.
INTRODUCTION
The incidence of end-stage heart failure has risen due to the aging population in Japan. The total number of 119 calls in Yokohama has experienced a rapid increase, reaching approximately 200,000 cases annually. In Yokohama, about 4% of these cases are diagnosed with heart failure. If the current situation persists, more elderly patients with heart failure will be transported to the emergency center, even as end-stage heart failure (Stage D) cases and hospital bed capacity become increasingly strained. This could potentially lead to the collapse of the entire regional health care system.
In December 2019, the Japanese government implemented the Stroke and Cardiovascular Disease Control Act. This legislation underscores the pressing necessity to establish a new treatment system for elderly patients with heart failure.
The Yokohama Medical Control Council (Yokohama MC) has discussed strategies to protect against the potential collapse of the health care system in the future, given the aging population in Yokohama, which currently stands at 3.76 million people.
Continuous positive airway pressure (CPAP) therapy is one of the treatments available for heart failure. The “Acute/Chronic Heart Failure Clinical Practice Guidelines” published by The Japanese Circulation Society1 emphasize the importance of early treatment for patients with heart failure, as it can help prevent aggravation of the condition. However, the benefits of early CPAP administration in prehospital emergency care settings in Japan have not yet been established. Currently, in Japan, the only way to administer early CPAP in the field is through a doctor's medical treatment. Consequently, the Yokohama MC has established dispatch criteria for Doctor Cars and developed a CPAP flowchart.
In Western countries, the National Association of EMS Physicians (2022) issued a statement recommending noninvasive ventilation, including prehospital CPAP therapy administration.2 Besides, a systematic review conducted in 2015 by the National Institutes of Health reported that prehospital administration of CPAP therapy was associated with reduced mortality and intubation.3, 4 By contrast, there are no findings from Japan regarding the prehospital administration of CPAP therapy, with only case reports available for the postoperative administration of CPAP therapy.5, 6
The aim of this study is therefore to describe the prehospital use of CPAP, which is already established as the first-line care in the emergency room for patients with heart failure but is being applied to patients transported by regional Doctor Cars (in Yokohama, utilizing the City 3–type Doctor Car system). However, currently in Japan, the law strictly prohibits paramedics from administering treatment. Therefore, the findings of this study could potentially contribute to the future consideration of granting fire station paramedics permission to administer such treatment.
METHODS
Study design
This study was a prospective observational case series supported by the Yokohama MC and the Foundation for Ambulance Service Development. The study was conducted between October 1, 2020, and January 24, 2022.
This study was approved by the Institutional Review Board of Yokohama City University Medical Center (approval number B201100014).
The regional Doctor Car system and CPAP equipment
In Yokohama City, with a population of 3.7 million, there are 2 types of Doctor Car systems (as of 2020). One was the All Yokohama Work-Station–type Doctor Car, and the other was the normal-type Doctor Car system, which included the Yokohama City University Medical Center Doctor Car and the National Hospital Organization Yokohama Medical Center Doctor Car. All Yokohama Work-Station–type Doctor Car's dispatch comprised one emergency doctor (from each emergency hospital in Yokohama), one nurse, and two or three fire station paramedics.
The Yokohama MC developed dispatch criteria for the Yokohama Doctor Car system (Table 1), which included patients with severe heart failure, and created a flowchart for the administration of CPAP in the field (Figure 1). We chose the Boussignac CPAP system (Figure 2A,B) due to its suitability for field use and safety features. The positive end-expiratory pressure can be monitored using a manometer within the Boussignac CPAP system (Figure 2D), which enhances patient safety and reduces the risk of pneumothorax.
|
- Note: The Yokohama MC established dispatch criteria for the Doctor Car system. Doctor Car dispatch is employed for patients with severe trauma, similar to other Doctor Car and Doctor-Heli systems. In Yokohama, Doctor Car dispatch is also utilized for patients with severe dyspnea.
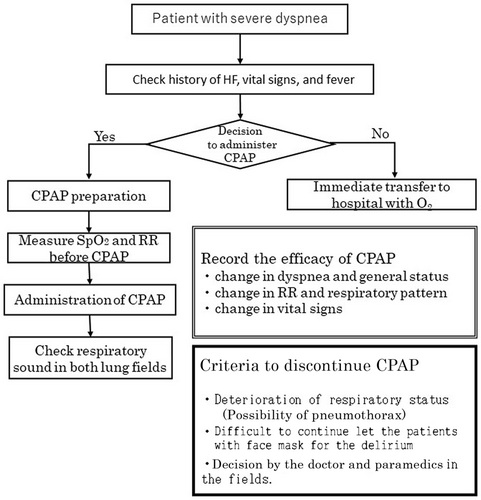
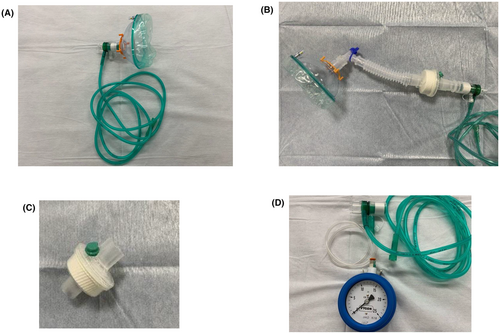
The Yokohama MC provided training to fire station paramedics on the use of CPAP in the field (Figure 3). To mitigate the potential spread of aerosols to the Doctor Car's cabin, we incorporated a virus filter into the Boussignac system as a preventive measure against coronavirus disease 2019 (COVID-19; Figure 2C).

Measurements
- demographic characteristics, such as sex, age, and occupation;
- clinical information, such as previous medical history (brain disease, heart disease, respiratory disease, cardiovascular disease, gastrointestinal disease, malignant neoplasm, psychiatric disease, etc.); degree of injury or illness (mild, moderate, severe, and serious) based on a domestic regulation and as determined by emergency medical services staff before hospital arrival; International Classification of Diseases 10th Revision (ICD-10) code; and initial electrocardiogram waveform;
- transport and prehospital information, including time of command, time of departure, time of arrival, time of contact, time of carry-out start, time of car entry, time of transport start, time of hospital arrival, time of patient accommodation, time of withdrawal, time of return, patient's condition on arrival/contact at the site (manual input), remarks and changes in condition (manual input), facial expression (normal, anguish, expressionless), complexion (normal, pale), skin (normal, cold sensation), position at contact (standing, sitting, semisitting, supine), bleeding (yes or no), other findings (manual input), and time of implementation (multiple entries allowed);
- patient's condition at the time of observation (multiple entries allowed), consciousness (multiple entries allowed), Japan Coma Scale (JCS) (multiple entries allowed), respiratory rate (multiple entries allowed), respiratory condition (multiple entries allowed), laterality in respiratory sound (multiple entries allowed), pulse rate (multiple entries allowed), and pulse condition (multiple entries allowed);
- presence of blood pressure measurement (multiple entries allowed), systolic blood pressure (multiple entries allowed), diastolic blood pressure (multiple entries allowed), oxygen saturation (SpO2) levels (multiple entries allowed), oxygen dose (multiple entries allowed), body temperature (multiple entries allowed), electrocardiogram waveform (multiple entries allowed), first aid (oxygen administration, heat retention, blood pressure measurement, SpO2 measurement, electrocardiogram monitor, body temperature measurement, pupillary reaction observation, auscultation [respiratory auscultation], auscultation [cardiac auscultation]); and
- utilized equipment (sphygmomanometer, stethoscope, thermometer, pulse oximeter, 12-lead electrocardiograph, monitor electrocardiograph, penlight, oxygen mask with reservoir, nasal cannula, oxygen inhaler, stretcher, emergency stretcher, blanket, restraining belt, others).
Descriptive statistics included calculating the median and interquartile ranges for continuous variables and determining the frequency and proportion for categorical variables. Furthermore, changes in SpO2 at three points, namely, without oxygen, with oxygen, and with CPAP, were plotted. Data aggregation was performed using IBM SPSS Statistics for Windows, version 25.0 (IBM Corp., Armonk, NY).
RESULTS
Between October 1, 2020, and January 23, 2022, a total of 661 Doctor Car dispatches were recorded. Among these, CPAP therapy was administered on-site in 13 cases. The median age (interquartile range) was 87 (79–94) years. Overall, 13 patients (92%) had a relevant previous medical history, including 1 (8%) with brain disease, 5 (38%) with heart disease, 4 (31%) with respiratory disease, 4 (31%) with cardiovascular disease, 1 (8%) with gastrointestinal disease, and 3 (23%) with other diseases such as diabetes mellitus. One additional patient (8%) was transferred from another institute due to the need for advanced treatment for carbon monoxide intoxication. Notably, there were no patients with psychiatric diseases.
In terms of the degree of illness, as documented in the medical records, 1 case (9%) was classified as mild, 5 cases (45%) as moderate, 4 cases (36%) as severe, and 1 case (9%) as serious. The median respiratory rate at contact (interquartile range) was 34% (30%–36%), heart rate was 99 (91–142) beats/min, systolic blood pressure was 148 (105–192) mmHg, and the body temperature was 36.6°C (36.2°C–36.7°C).
Regarding changes in SpO2 over time, the median (interquartile range), excluding missing values, was 89% (83%–93%) without oxygen, 95% (94%–99.3%) with oxygen, and 100% (97%–100%) with CPAP (Table 2; Figure 4). The median on-site stay time (interquartile range) was 11 (9–24) min, and the arrival time from dispatch command to the hospital was 28 (16–36) min. Respiratory distress was caused by heart failure in 10 patients (91%) and pneumothorax in 1 patient (9%). Importantly, none of the patients’ conditions worsened after the use of CPAP.
| Change | SpO2 (%), median (interquartile range) |
|---|---|
| Without O2 | 89 (83–93) |
| With O2 | 95 (94–99.3) |
| With CPAP | 100 (97–100) |
- Note: In Japan, medical treatment by paramedics is strictly prohibited by the law. Thus, CPAP therapy in this study was administered by Doctor Car personnel, including doctors, nurses, and fire station paramedics. This table shows the changes in SpO2 without O2, with O2, and with CPAP. Prehospital CPAP administration was found to be significantly effective.
- Abbreviations: CPAP, continuous positive airway pressure; SpO2, oxygen saturation.
DISCUSSION
The Yokohama MC engaged in discussions regarding the establishment of a new system in compliance with the Japanese law “Stroke and Cardiovascular Disease Control” within Yokohama City. As in other Japanese cities, the population aged over 70 years is increasing rapidly in this city; therefore, there is an urgent need to develop a novel and unique system for managing heart failure in an aging society. In response to the challenges posed by an aging society, the Yokohama MC determined that equipping CPAP attachments in the field represents one of the essential solutions for addressing heart failure.
We described the prehospital use of CPAP, a treatment modality already established as first-line care in emergency rooms for patients with heart failure, but now extended to patients transported via regional Doctor Cars. Currently, fire paramedics are strictly prohibited from performing medical treatments in Japan. As CPAP therapy falls under the category of medical treatment, fire station paramedics are not allowed to employ this procedure. In this study, CPAP therapy was administered by Doctor Car personnel, including doctors and fire station paramedics. The findings of this study are based on an uncontrolled analysis and a relatively small sample size. Although CPAP therapy was safely applied to our limited sample group, caution should be exercised when interpreting the findings. We anticipate that in the future, paramedics will gain the capability to utilize CPAP therapy in the field, potentially playing a crucial role in preventing health care system strain in our aging society.
The study was conducted during the COVID-19 pandemic in Japan. As CPAP therapy has the potential to generate aerosols that may be related to the transmission of the coronavirus, we decided to exclude patients with fever from the CPAP protocol as a precautionary measure. Because of the impact of the COVID-19 pandemic, the total number of cases included in the study was limited to 13.
CPAP is a positive airway pressure treatment that has the potential to promote or worsen pneumothorax, particularly in elderly patients. In this study, where the median patient age was 87 years, only one case was diagnosed with pneumothorax. However, no adverse events were observed during transportation to the hospital. The Boussignac CPAP system is equipped with a manometer to monitor the positive end-expiratory pressure levels, which enhances patient safety.
In this study, we conducted an examination based on a case series; nevertheless, parameters included in our research registry have the potential to be valuable for future large-scale observational studies. These parameters encompass variables such as sex, respiratory rate, and SpO2, which are considered covariates or confounding factors in patient prognosis, as emphasized in the literature.3 However, partial pressure of oxygen (PaO2) and partial pressure of carbon dioxide (PaCO2) have also been identified as confounding factors.3 In the future, the quality of examinations can be significantly enhanced by integrating this information with data collected during hospitalization following transportation. According to the most recent randomized controlled trial conducted with inpatients with COVID-19 in the United States, the administration of CPAP therapy resulted in a significantly lower intubation rate (33.4% vs. 41.3%, p = 0.03) compared with the group receiving standard oxygen therapy. In addition, the mortality rate decreased; however, there was no significant difference between the groups (16.7% vs. 19.2%, p = 0.37).7 Conducting large-scale multicenter collaborative research on CPAP therapy administration in Japan will underscore the importance of combining background variables and confounding factors.
There are some limitations to our study. This was an observational study limited to cases in Yokohama City. Thus, it is necessary to perform further studies by accumulating more cases in the future.
CONCLUSION
The study, supported by a regional MC council (Yokohama MC), described the prehospital use of CPAP, a treatment modality already established as first-line care in emergency rooms for patients with heart failure, but now extended to patients transported via regional Doctor Cars. Because of the impact of the COVID-19 pandemic, the total number of cases included in the study was limited to 13. Thus, we were not able to draw firm conclusions regarding the safety and effectiveness of CPAP. To the best of our knowledge, this is the first report of a prospective observational study of prehospital CPAP therapy originating from Japan, making our attempt both clinically and academically significant. However, it is necessary to conduct large-scale multicenter cohort studies, accumulate cases, and control confounding factors identified in previous findings to achieve increased safety and effectiveness verification.
ACKNOWLEDGMENTS
This study was supported by the Foundation for Ambulance Service Development.
CONFLICT OF INTEREST STATEMENT
The authors have declared that there is no conflict of interest.
ETHICS STATEMENT
Approval of the Research Protocol: The Institutional Review Board of the Yokohama City University Medical Center reviewed and approved the study protocol.
Informed Consent: The IRB waived a requirement to obtain informed consent.
Registry and the Registration No. of the Study/Trial: Not applicable.
Animal Studies: Not applicable.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.