Severe acute respiratory distress syndrome caused by Otsujito
Abstract
Background
Kampo prescriptions can cause drug-induced lung injury (DLI) and acute respiratory distress syndrome (ARDS). However, severe respiratory failure induced by Otsujito (OJT) is extremely rare. High-dose steroid pulse therapy is generally given to patients with severe DLI.
Case Presentation
A 63-year-old man with respiratory distress was admitted to our hospital. The patient was diagnosed with severe ARDS caused by OJT, which had been prescribed 4 weeks prior to admission. Thus, OJT was discontinued, and intensive care for ARDS, including ventilation and prone positioning, was implemented. His respiratory condition rapidly improved after treatment with an initial methylprednisolone dose (1.5 mg/kg/day). He was extubated on day 4 and discharged on day 16. The steroid dose was gradually reduced and discontinued by day 116.
Conclusion
A severe case of ARDS caused by OJT was successfully treated with low-dose steroids and specialized intensive care.
BACKGROUND
Kampo prescriptions are one of the causes of drug-induced lung injury (DLI). In particular, Scutellaria root is a Kampo prescription known to cause DLI. Reports have shown that Sho-saiko-to and Saireito, which also contain Scutellaria root, caused severe DLI and acute respiratory distress syndrome (ARDS), leading to death.1 Otsujito (OJT), used to relieve the symptoms of anal fissures and hemorrhoids, is made up of Japanese Angelica, Bupleurum, Scutellaria roots, Cimicifuga and Rhubarb rhizomes, and Glycyrrhiza. Cases of DLI caused by OJT have been reported, although there have been no reports of severe ARDS caused by OJT. Although high-dose steroid pulse therapy is recommended for severe DLI in Japan,2 the appropriate steroid dosage is still unknown.3 Herein, we report a case of ARDS caused by OJT successfully treated with low-dose steroid therapy and specialized intensive care, including prone positioning.
CASE PRESENTATION
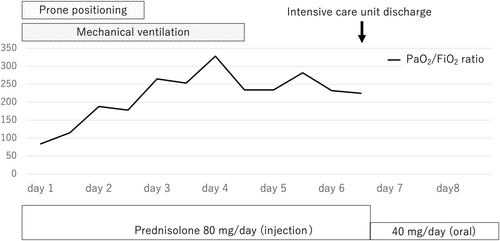
A 63-year-old man presented to a local hospital with fever and hypoxia. The patient experienced respiratory distress and dizziness without cough for 1 day, prior to the first visit. He had a history of hypertension and subarachnoid hemorrhage, and was allergic to penicillin. He had been prescribed OJT 6.0 g/day (Kracie Holdings, Ltd) for the past 4 weeks. He was an ex-smoker and had no episodes of resumption of smoking. His bodyweight was 55 kg. His initial vital signs were as follows: Glasgow Coma Scale score, 15 (E4V5M6); blood pressure, 114/86 mmHg; heart rate, 100 b.p.m.; respiratory rate, 42 breaths/min; oxygen saturation, 65% while breathing ambient air; and body temperature, 38.7°C. He was transferred to our hospital on the same day, intubated, and placed on a ventilator. The initial arterial blood gas showed pH 7.40, PaCO2 52 mmHg, PaO2 63 mmHg, HCO3− 32.2 mmol/L, and lactate 10 mg/dL at FIO2 0.75. Blood tests showed an elevated inflammatory response, with a white blood cell count of 9700/mm3, eosinophil count of 0.0/mm3, and serum C-reactive protein level of 18.5 mg/L. The following autoantibody screening was negative; antinuclear antibody, rheumatoid factor, myeloperoxidase-antineutrophil cytoplasmic antibody, and proteinase-3-antineutrophil cytoplasmic antibody tests were negative. Bacteriological and virological tests did not detect any infectious pathogens, including Legionella pneumoniae, Mycoplasma pneumoniae, Chlamydia pneumoniae, cytomegalovirus, and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Echocardiography revealed a normal ejection fraction of 60%. Chest radiography and computed tomography revealed bilateral ground-glass opacity with air bronchograms and pleural effusion (Figure 1A,B). In view of the clinical presentation, mild hydrostatic pulmonary edema might be possible, however, the most plausible diagnoses were drug-induced interstitial lung disease and severe ARDS due to OJT. He was admitted to the intensive care unit and started on meropenem and azithromycin, intravenous methylprednisolone (80 mg/day), and prone positioning (16 h/day). He was deeply sedated to suppress breathing efforts without neuromuscular blockade. In the ventilator setting, the tidal volume was limited to ≤8 mL/kg, and positive end-expiratory pressure was maintained above 10 cmH2O. All oral medications were discontinued.
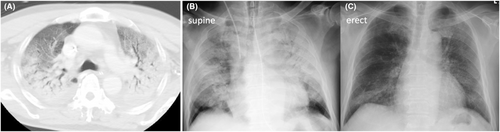
On day 3, the patient's respiratory condition improved. The PaO2/FIO2 ratio was 238 at FIO2 0.40 and brain natriuretic peptide level was 35.2 pg/mL. Prone positioning and antimicrobial treatment were terminated, ventilator settings were weaned, and deep sedation was switched to light sedation. The patient was extubated on day 4. On day 7, his oxygen saturation was 97% on 1 L/min oxygen by nasal cannula, and the ground-glass opacity was reduced (Figure 1C). Methylprednisolone was switched to oral prednisolone and the dose was reduced to 40 mg/day. The clinical course in the intensive care unit is described in Figure 2. On day 12, the Krebs von den Lungen-6 (KL-6) level was 798 U/mL. The patient was discharged on day 16. The dose of prednisolone was reduced based on clinical course indicators of interstitial lung disease such as KL-6 and chest radiographs: 40 mg on day 7, 20 mg on day 10, 15 mg on day 20, 10 mg on day 26, 7.5 mg on day 40, 5 mg on day 61, 2.5 mg on day 89, and discontinued on day 116.
DISCUSSION
Two points are noteworthy: first, ARDS caused by OJT can be lethal, and second, Kampo-induced ARDS was successfully treated with low-dose steroids and intensive care including prone positioning.
Kampo medicines can cause DLI and ARDS; however, this case is rare in that it was severe. In previous reports, the causative Kampo contained Scutellaria root in approximately 90% of the cases. The typical latent period of Kampo-induced DLI is generally 1–12 weeks.1 In this case, both the diagnostic criteria for DLI2 and the Berlin definition for severe ARDS4 were met. Otsujito was discontinued on day 1; on day 3, infection, autoimmune disease, and other causes were ruled out, and antimicrobial therapy was discontinued. Nevertheless, the patient's condition improved. We diagnosed DLI caused by OJT based on the clinical course. Eosinophilic pneumonia cannot be ruled out completely, however, there were no triggering episodes, such as the start of smoking. The resumption of OJT should have contributed to the diagnosis of DLI; however, it was not done due to the detriment of the patient. There are several types of DLI, with interstitial pneumonia being the most common. Three cases of DLI with interstitial pneumonia, due to OJT, have been reported previously, two of which were suspected to be ARDS. All cases showed good prognosis and ventilators were not required (Table 1).5-7 In our case, severe ARDS occurred rapidly within 1 day of the onset of subjective symptoms of dyspnea. Although OJT is widely prescribed in Japan, attention should be paid to its adverse effects, such as severe DLI and its rapid progression.
| No. | Age (years) | Computed tomography | Latent period (weeks) | Mechanical ventilation | Initial steroid | Prognosis |
|---|---|---|---|---|---|---|
| 1 (ref. 5) | 80 | Bilateral GGO | 8 | No | High-dose pulse | Survived |
| Pleural effusion | ||||||
| 2 (ref. 6) | 53 | Bilateral GGO | 4 | No | No | Survived |
| 3 (ref. 7) | 53 | Bilateral GGO | 2 | No | High-dose pulse | Survived |
| Pleural effusion | ||||||
| 4 (2022) | 69 | Bilateral GGO | 4 | Yes | 1.5 mg/kg | Survived |
| Pleural effusion |
- Abbreviation: GGO, ground grass opacity.
Steroids are commonly used in treating DLI. The appropriate steroid dosage and dose-reduction timing remain controversial. Japanese guidelines for DLI recommend that initial treatment of drug-induced ARDS should include 500–1000 mg/day of methylprednisolone for 3 days, continued at a prednisolone equivalent of 0.5–1.0 mg/kg/day, and tapered off.2 However, the benefits of high-dose steroid pulse therapy have not been established yet. However, guidelines for ARDS recommend a methylprednisolone dose of 1–2 mg/kg/day initially.4 Recent clinical studies suggest that early and prolonged use of low-dose steroids can improve outcomes for patients with ARDS.8 Conversely, high-dose steroids could be harmful and increase mortality and ventilator-free days.9 It is unclear how the steroid dose can be reduced, and there is variability among studies. Short-term reduction or discontinuation of steroids could elevate reintubation; therefore, even if ARDS improves and the patient can be weaned from the ventilator, it is better to taper the dose off gradually.8
In our case, the patient's condition improved substantially after discontinuation of the causative agent and initial methylprednisolone treatment (1.5 mg/kg) with intensive care, including prone positioning. Compared to previous reports,8 the initial steroid dose period was short and the time to completion was long. It is possible that the initial steroid dose period should have been prolonged. The reason it took 116 days to complete steroids was due to residual findings of drug-induced interstitial pneumonia.
This case suggests that high-dose steroids are not necessary for treating Kampo-induced ARDS, even in severe cases. However, it is difficult to determine which treatment was successful and the extent of success. The appropriate steroid dose for DLI types other than ARDS is not clear yet. Therefore, further studies are needed to determine the appropriate steroid dose for DLI.
CONCLUSION
Otsujito can cause severe ARDS. A patient with severe ARDS caused by OJT was successfully treated with low-dose steroid and intensive care, including prone positioning.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
Approval of the research protocol: N/A.
Informed consent: Written informed consent was obtained from the patient.
Registry and the registration no. of the study/trial: N/A.
Animal studies: N/A.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this paper.