Association between comorbid mental illness and preceding emergency department visits in unplanned admissions
Abstract
Aim
To investigate the association between comorbid mental illness and preceding emergency department (ED) visits in patients with unplanned admission.
Methods
This is a retrospective observational study using data from the EDs of three large tertiary medical facilities in Japan. We included adult patients who were admitted to these hospitals via the ED from 2017 to 2020. To investigate whether patients with mental illness were more likely to have preceding ED visits within 30 days prior to unplanned admissions compared with those without, we used univariate and multivariable logistic regression models. In the multivariable model, we adjusted for age category, gender, facility, year, and ambulance use.
Results
Out of 15,429 total admissions, 766 (5.0%) cases had documented comorbid mental illness and 14,663 (95.0%) did not. The prevalence of preceding ED visits among patients with mental illness was significantly higher than in those without (17.1% vs 8.8%; unadjusted odds ratio 2.15, 95% confidence interval [CI] 1.76–2.61; P < 0.001). This association was more prominent in the multivariable regression model (adjusted odds ratio 2.40, 95% CI 1.97–2.94; P < 0.001).
Conclusions
The presence of mental illness was significantly associated with a higher prevalence of preceding ED visits within 30 days prior to the unplanned admission. The result suggests that physicians should be more cautious in discharging patients with mental illness from the EDs and in providing care after ED discharge.
Abbreviations
-
- CI
-
- confidence interval
-
- COVID-19
-
- coronavirus disease 2019
-
- ED
-
- emergency department
-
- ICD-10
-
- International Classification of Diseases, 10th Revision
-
- IQR
-
- interquartile range
INTRODUCTION
Treatment of physical illness in patients with comorbid mental illness is a persistent existential issue that has gathered widespread attention across broad geographies in recent years. The life expectancy of patients with mental illness is 10–15 years shorter than patients without mental issues.1-4 Most premature deaths of the patients with mental illness are not a result of suicide, but instead attributed to physical illnesses.3, 5 Multiple studies have contributed to the general consensus that mental illness is a risk factor for lifestyle-related diseases.6-8
Further fueling this complexity, patients with mental illness have been challenged with apparent inequalities in the standard of care granted when compared with patients without mental issues.6, 8, 9 For example, patients with mental illness tend to receive fewer opportunities to undergo invasive coronary procedures after cardiac events.8 The emergency department (ED) is an essential common ground for patients presenting with a variety of physical manifestations of disease regardless of the presence or absence of underlying mental illness. Given the previously reported disparities in the quality of care granted to patients with comorbid mental illness,7, 9 patients with mental illness who visit the ED may be inadequately assessed; however, inequalities in the emergency and urgent care setting remain poorly documented. Therefore, the present study aimed to investigate the association between comorbid mental illness and prevalence of preceding ED visits in patients with unplanned hospital admissions.
MATERIALS AND METHODS
Study design and data collection
This is a retrospective observational study using data derived from the EDs of three healthcare facilities in Japan between January 1, 2017, and October 30, 2020. Participating hospitals were Hitachi General Hospital, Saiseikai Utsunomiya Hospital, and the Japanese Red Cross Society Kyoto Daiichi Hospital. These facilities are tertiary care centers situated in different regions of Japan. These data were entered as medical charts into a designated system by the treating doctor or nurse at the time of the patients’ visit to the EDs. The medical charts were structured using the Next Stage ER system (TXP Medical Co. Ltd., Tokyo, Japan). This system allows for efficient retrieval of reliable and structured data.10-12 The data include personal identification number, date and time of visit, age, sex, method of visit (ambulance use), chief complaints, medical history, history of the present illness, vital signs (body temperature, heart rate, systolic blood pressure, diastolic blood pressure and respiratory rate), oxygen saturation, findings on physical examination, diagnosis, and subsequent events (hospitalization or not). The diagnosis and medical histories are recorded as Japanese text according to the International Classification of Diseases, 10th Revision (ICD-10) codes.
Participants
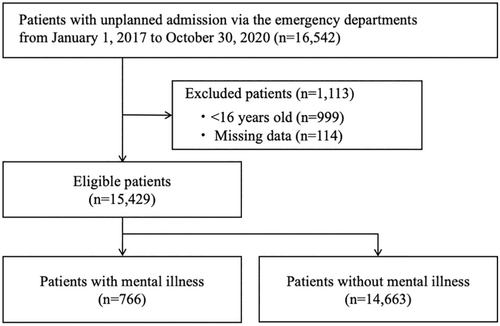
We included all adult patients (aged ≥16 years) with unplanned admission via the ED during the study period. We excluded patients with missing information about age, sex, and ambulance use.
Exposure and outcome
We divided the patients into two groups according to whether they had comorbid mental illness (mental illness group) or not (non-mental illness group). Comorbid mental illness was defined using the following ICD-10 codes: F00–09 and F20–99. We did not include substance use disorder (F10–F19) according to previous studies.13, 14 The outcome of the present study was the prevalence of preceding ED visit within 30 days prior to the unplanned admission. The 30-day interval is a metric often adopted in similar studies investigating readmissions and ED revisits.15-17
Statistical analysis
We described the patients' characteristics using median and interquartile range for continuous variables and number and percentage (%) for categorical variables. Percentage was compared using chi-square test.
We fit univariate and multivariable logistic regression models to examine associations between the presence of comorbid mental illness and the prevalence of preceding ED visits within 30 days prior to the unplanned admission. In the multivariable model, we adjusted for age, sex, facility, pre- or current COVID-19 (coronavirus disease 2019) pandemic (before or after March 1, 2020, respectively)18 and ambulance use. As a sensitivity analysis, we performed a subgroup analysis excluding unplanned admissions with psychiatric chief complaints. We also examined the prevalence of preceding ED visits within 7 days prior to the unplanned admission. We considered a 2-sided P < 0.05 to be statistically significant. All analyses were performed with STATA BE 17 (College Station, TX, USA).
Ethics
The study protocol was approved by the Ethics Committee of TXP Medical Co. Ltd (approval number: TXPREC-002). The requirements for informed consent were waved due to the retrospective nature of the study. Only anonymized data were collected from each participating institution.
RESULTS
Patient flow
During the study period, the database recorded 16,542 patients with unplanned admissions. Of these, we identified 15,429 patients including 766 (5%) in the mental illness group and 14,663 in the non-mental illness group (Fig. 1).
Patient characteristics
The characteristics of the eligible patients are presented in Table 1. The mental illness group had a significantly lower median age than the non-mental illness group (70 vs 76 years of age, respectively). In comparison with the non-mental illness group, the mental illness group had a lower proportion of males (51.3% in the mental illness group vs 58.4% in the non-mental illness group) and a higher proportion of ambulance use (80.7% in the non-mental illness group vs 74.6% in the mental illness group). Circulatory disease, digestive disease, respiratory disease, and injury were the most frequent diagnoses in both groups.
| Variables | Patients with mental illness (n = 766) | Patients without mental illness (n = 14,663) | P-value | |
|---|---|---|---|---|
| Age (years), median (IQR) | 70 (51–81) | 76 (64–83) | <0.001 | |
| Sex, male | 393 (51.3) | 8,564 (58.4) | ||
| Study period, current COVID-19 pandemic | 178 (23.2) | 4,661 (31.8) | <0.001 | |
| Facility | ||||
| Hitachi General Hospital | 55 (7.2) | 1,649 (11.2) | ||
| Saiseikai Utsunomiya Hospital | 63 (8.2) | 789 (5.4) | ||
| Japanese Red Cross Kyoto Daiichi Hospital | 648 (84.6) | 12,225 (83.4) | <0.001 | |
| Ambulance use | 618 (80.7) | 10,945 (74.6) | <0.001 | |
| Diagnosis at emergency department | ||||
| Infectious and parasitic diseases [A, B] | 17 (2.2) | 347 (2.4) | <0.001 | |
| Neoplasms [C, D] | 30 (3.9) | 753 (5.1) | ||
| Endocrine, nutritional, and metabolic diseases [E] | 36 (4.7) | 400 (2.7) | ||
| Mental and behavioral disorders [F] | 61 (8.0) | 6 (0.0) | ||
| Diseases of the nervous system [G] | 22 (2.9) | 307 (2.1) | ||
| Diseases of the eye, adnexa, ear, and mastoid process [H] | 2 (0.3) | 68 (0.5) | ||
| Diseases of the circulatory system [I] | 176 (23.0) | 4,023 (27.4) | ||
| Diseases of the respiratory system [J] | 71 (9.3) | 1,505 (10.3) | ||
| Diseases of the digestive system [K] | 86 (11.2) | 2,537 (17.3) | ||
| Diseases of the skin and subcutaneous tissue [L] | 7 (0.9) | 121 (0.8) | ||
| Diseases of the musculoskeletal system and connective tissue [M] | 6 (0.8) | 146 (1.0) | ||
| Diseases of the genitourinary system [N] | 39 (5.1) | 714 (4.9) | ||
| Pregnancy, childbirth, puerperium, and perinatal condition [O, P] | 0 (0.0) | 159 (1.1) | ||
| Symptoms, signs, and abnormal clinical and laboratory findings [R] | 63 (8.2) | 831 (5.7) | ||
| Injury, poisoning, and certain other consequences of external causes [S, T] | 113 (14.8) | 1,578 (10.8) | ||
| Others [X, Z, Q] | 1 (0.1) | 18 (0.1) | ||
| Missing | 36 (4.7) | 1,150 (7.8) | ||
- Note: Data are presented as n (%) unless indicated otherwise. Abbreviations: COVID-19, coronavirus disease 2019; ICD, International Classification of Diseases; IQR, interquartile range.
Outcomes
The results of regression analyses are shown in Table 2. The prevalence of preceding ED visits within 30 days prior to the unplanned admissions among the patients in the mental illness group was significantly higher than those in the non-mental illness group (17.1% vs 8.8%; unadjusted odds ratio 2.15, 95% confidence interval [CI] 1.76–2.61; P < 0.001). Likewise, in the multivariable logistic regression model, having mental illness was significantly associated with a higher prevalence of preceding ED visits within 30 days prior to the unplanned admissions (adjusted odds ratio 2.40, 95% CI 1.97–2.94; P < 0.001). The median intervals between preceding ED visit and unplanned admission were similar between the two groups (6 days vs 5 days; P = 0.20).
| Variable | Odds ratio (95% CI) | P-value |
|---|---|---|
| Univariate analysis | ||
| Presence of mental illness | 2.15 (1.76–2.61) | <0.001 |
| Multivariable analysis | ||
| Presence of mental illness | 2.40 (1.97–2.94) | <0.001 |
| Age, 10 years | 1.05 (1.02–1.08) | 0.004 |
| Sex, male | ||
| Female | Reference = 1 | |
| Male | 1.02 (0.92–1.15) | 0.68 |
| Study period | ||
| Pre-COVID-19 pandemic | Reference = 1 | |
| Current COVID-19 pandemic | 1.25 (1.07–1.45) | 0.004 |
| Facility | ||
| Japanese Red Cross Kyoto Daiichi Hospital | Reference = 1 | |
| Hitachi General Hospital | 1.37 (1.11–1.71) | 0.004 |
| Saiseikai Utsunomiya Hospital | 1.47 (1.12–1.93) | 0.005 |
| Ambulance | ||
| No ambulance use (walk-in) | Reference = 1 | |
| Ambulance use | 0.40 (0.36–0.45) | <0.001 |
- Note: The prevalence of preceding ED visits within 30 days prior to the unplanned admissions was 17.1% (131/766) and 8.8% (1,285/14,663) among patients in the mental illness group and non-mental illness group, respectively.
- Abbreviations: CI, confidence interval; COVID-19, coronavirus disease 2019; ED, emergency department.
The results of the sensitivity analysis were consistent with the main analysis. Unplanned admissions with psychiatric chief complaints were excluded from this sensitivity analysis. The adjusted odds ratio was 1.69 (95% CI 1.27–2.25; P < 0.001; Tables S1 and S2). In the analysis examining the prevalence of preceding ED visits within 7 days prior to the unplanned admission, the adjusted odds ratio was 2.14 (95% CI 1.65–2.77; P < 0.001; Table S3).
DISCUSSION
The present study investigated the association between comorbid mental illness and preceding ED visits in patients with unplanned hospital admissions. The presence of comorbid mental illness was significantly associated with a higher prevalence of preceding ED visits within 30 days prior to the unplanned admission.
Several studies have reported on the inequality of physical treatment for patients with mental illness in outpatient and inpatient settings.6-8, 19 For example, patients with mental illness were less likely to be prescribed statins for dyslipidemia than those without and receive invasive coronary procedures after cardiac events.8, 19 Assessments of the mental condition of patients with mental illness presenting to the ED have been previously reported.20-22 However, studies focusing on the assessment of the physical illness in patients with mental illness in ED settings are limited. We investigated the association between comorbid mental illness and preceding ED visits in patients with unplanned hospital admissions in a multicenter setting.
The underlying mechanisms of our findings are likely multifactorial. First, physicians in the EDs may tend to underestimate the physical condition of patients with comorbid mental illness.23 Second, patients with mental illness could not be hospitalized at the timing of the preceding ED visit for reasons such as social, financial, and psychiatric problems regardless of the recommendations of physicians in the EDs.24 Lastly, physical illness of patients with mental illness may deteriorate more rapidly than expected due to daily habits and the problems of adherence.5, 25, 26
The present study suggests the likelihood of an opportunity to intervene in the physical illness of patients with comorbid mental illness prior to unplanned admissions. The unplanned admission is not entirely due to the underestimation of ED physicians. Introducing social services such as connecting patients with mental illness to the local public welfare office might be efficient to mitigate unplanned admissions in this subset of patients. A lower threshold for initiating objective testing and examinations should also be considered for patients with mental illness because it may be difficult to obtain an accurate and comprehensive history from these patients. When discharging these patients to their home environments from the ED, we suggest that social resources be checked and scrutinized to ensure that appropriate medical and psychiatric continuity of care can be provided.
Our study has several potential limitations. First, the diagnosis at the ED and medical history were manually recorded by ED physicians. Because the definition of comorbid mental illness of this study was based on medical records, misclassification of the exposure would influence the results. Second, our data do not include the information on whether the patients refused to be hospitalized at the first ED visit regardless of the recommendation for hospitalization by ED physicians. Third, we identified only revisits to the EDs in the same facility. Therefore, the patients who revisit or were hospitalized at other facilities after the preceding ED visit could not be identified. This might be a potential source of selection bias. Fourth, the threshold for ED visits may be lower among patients with mental illness. This is inferred from the higher prevalence of ambulance use among patients with mental illness. Because ambulance use was adopted as a surrogate marker for assessing patient severity, the differences in clinical severity between the two groups may not have been sufficiently adjusted for. Finally, the present study was performed in Japan and the results might not be applicable to other countries with different emergency medical systems. While the multicenter design could, at least partially enhance the generalizability, further investigation on the potential influence of having mental conditions on the screening process currently undertaken at the preceding ED visits is warranted.
CONCLUSION
Among the patients with unplanned admission via EDs, the presence of mental illness was significantly associated with a higher prevalence of preceding ED visits within 30 days prior to the unplanned admission. ED physicians should grant extra attention to patients with comorbid mental illness so as not to miss the opportunity to treat them on their initial ED visits. Our findings warrant further investigation on the potential influence of having mental conditions on the screening process currently undertaken at the preceding ED visits.
ACKNOWLEDGEMENTS
The authors thank Ms Honoka Ito for data cleaning. We are also grateful to Dr Richard H. Kaszynski for his support on English proofreading and advice on academic writing.
FUNDING INFORMATION
TS is the SIP AI hospital research project chief researcher funded by the Japanese Cabinet Office.
DISCLOSURE
Approval of the Research Protocol with Approval No. and Committee Name: The present study was approved by the Institutional Review Board at TXP Medical Co. Ltd. (approval number: TXPREC-002).
Informed Consent: Because of the anonymous nature of the data, the requirement for patient informed consent was waived.
Registry and the Registration No. of the Study/Trial: N/A.
Animal Studies: N/A.
Conflict of Interest: AO and MN are part-time employees of TXP Medical Co. Ltd. TG is the Chief Scientific Officer, TXP Medical Co. Ltd. TS is the Chief Executive Officer, TXP Medical Co. Ltd. None of the authors received any financial incentives for this work from TXP Medical Co. Ltd. TXP Medical Co. Ltd. may gain potential profit from the manuscript acceptance, such as the use of results to introduce the NEXT Stage ER system.