Traumatic internal carotid artery aneurysm distant from facial bone fractures treated with a flow diverter stent: A case report
Abstract
Background
Traumatic intracranial aneurysms (TICAs) can be fatal if ruptured. We report a case of a TICA, distant from facial bone fractures, successfully treated with flow diverter (FD) before rupture.
Case Presentation
A 20-year-old woman was admitted following a car accident. Initial contrast-enhanced computed tomography revealed traumatic subarachnoid hemorrhage, a 5-mm internal carotid artery aneurysm, LeFort type I + II, and mandibular fracture. On Day 8, she developed oculomotor palsy, and digital subtraction angiography revealed the aneurysm had increased to 12 mm. She started dual antiplatelet therapy (DAPT) following facial fracture repair. On Day 17, FD was placed, resulting in contrast agent stagnation within the aneurysm. Three months postinjury, her neurological symptoms improved.
Conclusion
Screening for cerebrovascular injury is crucial several days following severe head trauma, even without skull base fractures. Unruptured TICA can be safely treated with FD following DAPT administration.
INTRODUCTION
Traumatic intracranial aneurysms (TICAs) are rare, accounting for <1% of all intracranial aneurysms.1 TICAs frequently occur in individuals under 20 years and young adults.2 Ruptured TICAs have a mortality rate of 32%–54%3; therefore, preemptive occlusion is recommended. Flow diverter (FD) has recently gained popularity for treating nontraumatic aneurysms, and their efficacy for TICA is being explored. We report a case of a TICA distant from facial bone fractures, successfully treated with FD before rupture, leading to a favorable outcome.
CASE REPORT
A 20-year-old woman with no significant medical history was admitted following a car accident. The following were her vital signs on arrival: Glasgow Coma Scale score: E4V4M6; blood pressure: 127/62 mmHg; pulse rate: 110 beats/min; respiratory rate: 29 breaths/min; SpO2: 100% (under reservoir oxygen mask at 10 L/min); and body temperature: 36.2°C. Physical examination using a pupilometer revealed reactive pupils measuring 4.1 mm/3.8 mm, nosebleed, intraoral hemorrhage, limited mouth opening (0.5 lateral fingers), and multiple facial contusions.
Using the expanded Denver screening criteria,4 we performed contrast-enhanced computed tomography (CT) of the head and neck vessels to screen for blunt cerebrovascular injury (BCVI). Contrast-enhanced CT revealed subarachnoid hemorrhage in the right Sylvian fissure (Figure 1A), a 5-mm wide-necked aneurysm in the cavernous portion of the right internal carotid artery (ICA) (Figure 1B), LeFort I + II maxillary fractures, and a mandibular fracture (Figure 1C,D). The aneurysm was distant from the subarachnoid hemorrhage in the right Sylvian fissure. No fractures were observed around the right ICA (Figure 1E,F). Additional fractures included an open right humeral fracture and a left clavicular fracture.
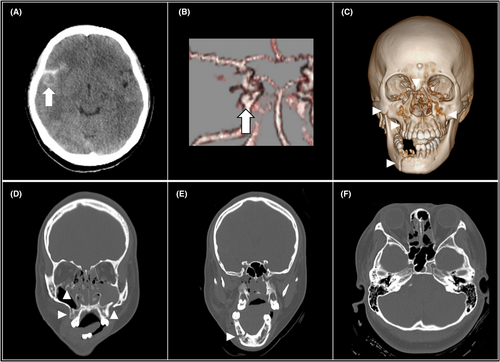
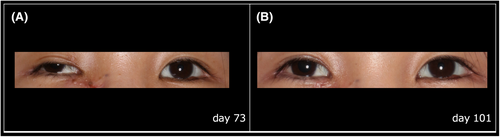
She was intubated and underwent debridement and external fixation of the right humerus. On Day 4, follow-up CT revealed the aneurysm had increased to 7 mm (Figure 2A). On Day 5, intramaxillary fixation was performed. On Day 7, right humeral and left clavicular open reduction and internal fixation along with tracheotomy were performed. On Day 8, she developed severe ptosis, exotropia, a dilated pupil, and impaired eye adduction on the right side. On Day 10, digital subtraction angiography revealed the aneurysm had enlarged to 12 mm (Figure 2B). On Day 11, facial bone open reduction and internal fixation was completed. On Day 12, she started dual antiplatelet therapy (DAPT, aspirin 100 mg and prasugrel 3.75 mg) for FD stenting.
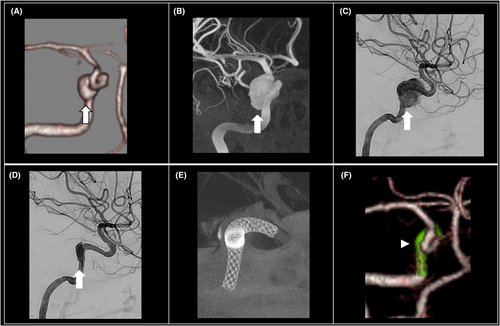
On Day 17, endovascular treatment was performed under general anesthesia. A 6-Fr 90-cm FUBUKI catheter (Asahi Intec Co., Ltd., Aichi, Japan) was placed in the proximal right ICA through the right common femoral artery. To maintain an activated clotting time of >250 s, systemic heparin was administered. Phenom Plus (Medtronic, Minneapolis, MN, USA) was navigated over a Phenom 27 microcatheter (Medtronic, Minneapolis, MN, USA), into the petrous segment of the right ICA. The microcatheter was navigated over Synchro Select microwire (Stryker, Fremont, CA, USA) into the M1 segment of the right middle cerebral artery. A 3.75 × 18-mm Pipeline embolization device (Medtronic/Covidien, Irvine, CA, USA) was partially unsheathed within the M1 and subsequently pulled into the ICA and deployed across the aneurysm neck. Angiography revealed a widely patent stent, apposition against the vessel wall, complete aneurysm neck coverage, and a reduction and stagnation of contrast agent flow into the aneurysm (Figure 2C–E). Three months postinjury, CT angiography revealed complete aneurysm occlusion and confirmed the patency of the stented segment of the ICA (Figure 2F). Her neurological symptoms partially improved, achieving Glasgow Outcome Scale score of 4 (Figure 3).
DISCUSSION
TICA, frequently lacking vascular intima, pose a high risk of rupture due to their instability. Even small aneurysms can rapidly enlarge, with the highest rupture risk occurring 2–3 weeks postinjury.5 It is essential to recognize that TICAs can form or enlarge even without immediate neurological symptoms, necessitating follow-up imaging in high risk for BCVI.4 Early recognition and intervention can prevent life-threatening complications, such as carotid-cavernous fistula or aneurysmal rupture. Risk factors for BCVI include excessive neck extension, cervical soft tissue injury, skull base fractures, and LeFort II and III facial fractures.4 TICAs can form from direct vessel injuries or indirect injuries from vessel stretching. ICA transitions from fixed structures in the skull base and cavernous sinus to relatively mobile structures in the cisternal spaces. Movement against the foramen lacerum or the anterior clinoid process, or ICA stretching at this transition zone can lead to aneurysm formation.5 In our case, the TICA was distant from facial bone fractures. External forces from the foramen lacerum likely caused direct damage or stretching of the ICA, leading to the formation of the TICA. The TICA increased from 5 to 7 mm by Day 4 and reached 12 mm by Day 10, extending into the cavernous sinus. Its location suggests that rupture would likely have resulted in carotid-cavernous fistula rather than subarachnoid hemorrhage. CT images on Day 4 prompted careful follow-up and early FD stenting for the unruptured cerebral aneurysm.
TICAs are often treated surgically, but fragile vessel walls, difficult access, and poor collateral circulation result in high mortality rates (18%–29%).1, 6 FD offer a safer alternative, reducing rupture risk and preserving circulation, with lower mortality (0%–11%).7, 8 However, FD causes delayed occlusion due to slow thrombus formation and is less effective for high-pressure or ruptured aneurysms. FD placement requires DAPT (Supplement Table),2, 7-9 increasing bleeding risk in trauma patients. Timing of FD stenting is critical, especially with multiple surgeries. In our case, DAPT started on Day 12, after all surgeries were completed. While long-term outcomes for FD in TICA are unclear, complete occlusion rates for nontraumatic aneurysms reach 84.5% at 2 years and 96% at 5 years.10 Most complications occur early, with few events beyond 2 years.10 Therefore, careful follow-up for at least 2 years seems to be essential.
CONCLUSION
TICAs can be fatal if ruptured. Screening for BCVI is essential several days following severe head trauma, even without skull base fractures. Unruptured traumatic cerebral aneurysms can be safely treated with FD following DAPT administration.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
Approval of the Research Protocol: None.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Registry and the Registration No. of the study/trial: None.
Animal Studies: None.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.