Diagnostic utility of point of care ultrasound in identifying cervical spine injury in emergency settings
Abstract
Introduction
The evaluation of cervical-spine in a major trauma patient needs a bedside efficient tool to rule out cervical spine injury as the role of X-ray and Computed Tomography (CT) in this setting is limited. Point of care ultrasonography (POCUS) is being used as an adjunct during trauma resuscitation. The aim of this study was to evaluate the use of POCUS for identifying cervical spine injuries.
Methods
We recruited 84 cases with cervical spine injury based on CT scan after taking consent. POCUS was used as per the operational definition of study methods while maintaining manual in-line stabilisation. Statistical analysis was done by using STATA version 14.
Results
Normal cervical anatomy was visible through anterior approach in POCUS except for the 1st and 2nd cervical vertebrae. The sensitivity and specificity of POCUS vs CT scan for vertebral body listhesis were 84.52% (95% CI of 0.65–0.95) and 89.66% (95% CI 0.78–0.96) with p-value <0.0001. Sensitivity and specificity of POCUS vs CT for vertebral body fracture were 40.91% (95% CI of 0.20–0.63) and 96.77% (95% CI of 0.88–0.99) with p-value <0.0001. The overall sensitivity and specificity of POCUS were 45.83% and 83.33% (p = 0.06) and excluding isolated posterior column injuries, sensitivity and specificity were 70.21% and 83.33% (p < 0.05).
Conclusion
POCUS identified injuries such as fracture and listhesis. Because of high rate of missed injuries, ultrasound at present cannot be used as a screening or diagnostic tool for decision-making in cervical spine injury.
Introduction
Cervical spine injury (C-spine injury) is the most common debilitating injury among spinal cord injuries. Of all patients with traumatic brain injuries, 5–10% have associated C-spine injury.1 There are various clinical decision-making tools such as NEXUS criteria2 and Canadian C-spine rule3 for evaluation of patients with a suspected C-spine injury with variable accuracy. A considerable amount of variation exists with radiological evaluation. X-ray was used for decades and consisted of a 3-view cervical spine series. However, this conventional series of X-rays reported up to 35% of missed C-spine injuries.4, 5
CT scan has emerged as a good screening tool in C-spine injury due to its high negative predictive value.6, 7 Many clinical guidelines do not recommend CT in a haemodynamically unstable trauma patient.8, 9 This results in delayed clearance of C-spine in unstable patients. Prolonged immobilisation of C-spine is associated with an increased risk of pressure sores and raised intracranial pressure (ICP).10, 11 Recent evidence suggests the application of a rigid cervical collar for a short period results in a change of optic nerve sheath diameter in healthy volunteers.12 So the ideal C-spine clearance protocols must balance the risk of missed injury against the potential for increased morbidity from prolonged spinal immobilisation.
Evaluation of C-spine in an unstable patient warrants a portable, but an efficient tool in ruling out C-spine injury. Portable ultrasound has been used as an adjunct in trauma resuscitation protocols.13, 14 The aim of this study was to evaluate the use of POCUS for identifying cervical spine injuries.
Methodology
It was a single-centre, cross-sectional study conducted at a level 1 trauma centre over 18 months. The primary objective was determining the ability of POCUS to detect c-spine injuries in proven cases of c-spine injury. The secondary objective was to study the normal anatomy of the c-spine in patients without c-spine injury and user-friendliness of probes (curvilinear vs. linear) in terms of image acquisition, optimisation and interpretation.
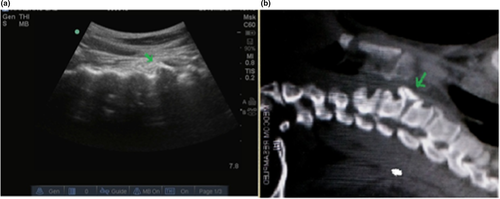
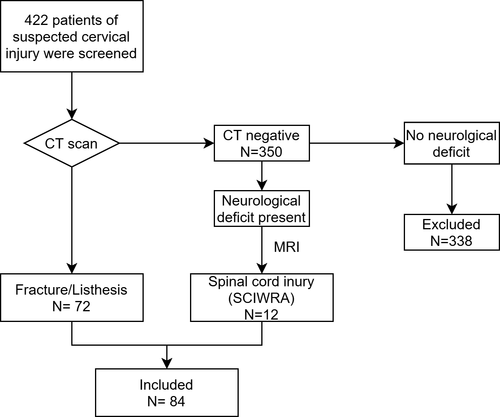
The study was conducted in two phases. The recruitment team consisted of two emergency physicians (EPs) posted in the level 1 trauma centre. In phase one, they were trained in the POCUS algorithm to identify c-spine injury under the supervision of an emergency medicine consultant who is an expert in emergency ultrasound to standardise the technique. Each of the EPs performed POCUS in 20 normal and 10 abnormal cases. The image/videos were assessed by the emergency medicine consultant for image acquisition, optimisation and interpretation by the performer. Phase one was done over 3 months. Then in the second phase, all patients over the age of 18 months, who had a suspicion of cervical injury based on NEXUS2 criteria, were screened and a cervical CT was performed. The patients with cervical spine injury were triaged as red and observed in the Emergency department (ED) for admission. The EPs performing the ultrasound were not part of the trauma resuscitation team. The ultrasound images were recorded independently by the recruitment team. Patients with a focal neurological deficit but a normal CT scan underwent magnetic resonance imaging (MRI) (Figure 1). CT findings were interpreted separately by the radiologist. The EPs performing the POCUS were blinded to the finding of the CT/MRI. Those with positive CT findings were included in the study. The patients with no neurological deficit and normal CT scan were excluded. After every 5 scans, the images were verified by the consultant for image acquisition, optimisation and interpretation.
All patients were managed by Advanced Trauma Life Support protocol (ATLS) and POCUS was performed independently without affecting the management of the patient. All haemodynamically unstable patients, patients with previous cervical injuries, operated cases of C-spine and paediatric cases (age < 14 years) were excluded. Informed consent was taken from each patient who was enrolled in the study. In patients with altered consciousness, the consent was taken from the legally accepted representative. Ethical clearance was granted by the institution's review board (IESC/T-40/20.01.2015, RT-13/01.04.2015).
POCUS Technique
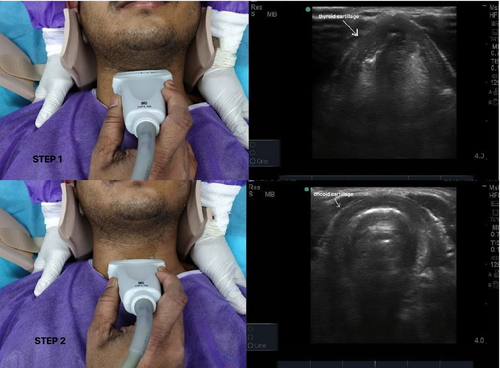
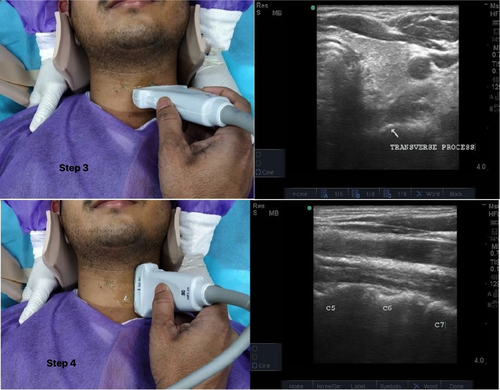
A portable ultrasound machine (SonoSite MicroMaxx, Bothell, WA 98021, USA) with adult linear (7–15 MHz,) and curvilinear (3–5 MHz) probes was used sequentially. The anterior part of the cervical collar was removed for the ultrasound examination while the posterior part of the cervical collar was in place while maintaining manual in-line stabilisation. The probe was first placed transversely over the anterior part of the neck to identify the thyroid cartilage. Then the probe was moved caudally to identify cricoid. After identifying cricoid, the probe was slid laterally until the vertebrae became visible in the ultrasound image as they created a hyperechoic line and posterior acoustic shadow. Sixth cervical vertebra corresponds to cricoid.15 The probe was then placed longitudinally with probe pointer directed cranially. The carotid artery and internal jugular vein were identified first, and then the probe was fanned medially until the hyperechoic shadow of the bony structure of the cervical spine was visualised. The vertebral body was again identified as a hyperechoic structure with posterior acoustic shadow. Steps 1 to 4 described in Figures 2, 3. The bony cortical integrity, alignment of vertebral bodies and extent of visibility of cervical vertebra were assessed in both the groups. After the examination, the anterior part of the cervical collar was again put back followed by releasing the manual in-line stabilisation.
A fracture was defined as a cortical break or reduction in the longitudinal length of vertebral body and listhesis was seen as the distorted alignment of vertebral bodies, loss of cervical lordosis or acute kyphotic angulation at the level of injury. Images were saved in the machine and sent to the supervisor for verification after every five scans. With anticipated identification rate of about 70% with ultrasound and absolute precision of ±10 %, a sample size of 84 was deemed adequate. Demographic, clinical details and POCUS findings of the patients were noted in a pre-designed proforma and saved in Microsoft excel. All statistical analysis was performed using STATA version 14.
Results
Cervical ultrasound was done in 84 patients with CT/MRI-confirmed C-spine injury. The average age in C-spine injury (group II) was 37.2 ± 14 years with 72 males (85.7%) and 12 females (14.3%). Road traffic injury (52.4%) and fall from height (38.1%) were the commonest modes of injury. Head injury (14%) was the most common associated injury. Fifty-seven (57.8%) patients had neurological deficits out of the total patients. The commonest vertebral fracture (including body and posterior elements) observed by CT scan was C6 (C6 = 24; C5 = 23; C7 = 19; C4 = 10, C2 = 8, C3 = 3; C1 = 1). Based on CT scan, 51% (43/84) had injury involving more than one vertebra. There were nine (11%) cases of upper cervical spine injury (C1 and C2) and 63(76%) cases of lower cervical spine injuries. Twelve patients (14%) had spinal cord injury without radiographic abnormalities (SCIWRA). Neurologic deficits and cord signal changes in MRI were present in all cases with SCIWRA (Table 1).
| Characteristics | |
| Age | 37.19 ± 14 |
| Gender | |
| Male | 72 (85.7%) |
| Mode of injury | |
| Road traffic injury | 44 (52.4%) |
| Fall from height | 32 (38.1%) |
| Other mechanisms | 8 (10%) |
| Associated injuries | |
| Head injury | 12 (14%) |
| Multiple spinal level injury | 4 (4.7%) |
| Long bone fracture | 4 (4.7%) |
| Blunt trauma abdomen | 3 (3.5%) |
| Neurologic findings | |
| Quadriplegia | 18 (21.4%) |
| Incomplete quadriplegia | 27 (32.1%) |
| Quadriperisis | 9 (10.7%) |
| UL weakness > LL | 3 (3.6%) |
| No neurologic deficits | 20 (23.8%) |
| Status could not be assessed | 7 (8.3%) |
| Level of cervical spine injury | |
| Lower cervical spine injury | 63 (75%) |
| Upper cervical spine injury | 9 (10.7%) |
| SCIWRA | 12 (14.2%) |
- Data are mean ± SD or N (%).
- Abbreviations: LL, Lower Limb; SCIWRA, Spinal Cord Injury without radiological abnormality; UL, Upper limb.
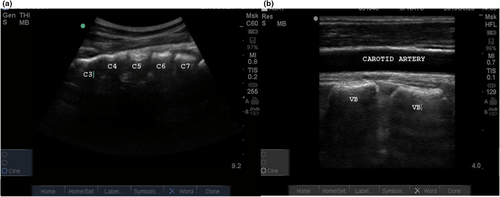
Normal anatomy on POCUS
Vertebral bodies were seen as blocks with a concave anterior surface in the anterior longitudinal axial scan. Maximum visibility was from C3 to C7-T1 junction. POCUS could also visualise cervical lordosis, intervertebral disc spaces and anterior longitudinal ligament (ALL).
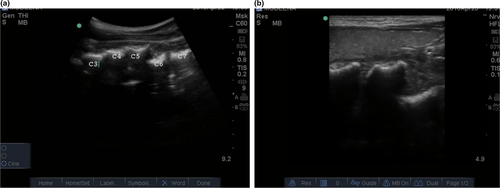
The optimal images were acquired between 7.8 cm and 9.2 cm of depth with the curvilinear probe. The alignment of vertebral bodies was seen with curvilinear probe (Figure A1a). The quality of images was better with the linear probe (Figure A1b) when compared to the curvilinear probe. However, only two vertebrae were seen in a single window and the alignment was not visualised. The optimal image was obtained by adjusting the depth of the linear probe to 4 cm and directing the plane through the carotid artery or internal jugular vein (Figure A1b).
C3 vertebra was visible in 25% (21/84), C4 in 92% (78/84), C5-C7 in 100% and C7-T1 junction was visible in 52% (44/84).
Upper cervical vertebra (C1 & C2), transverse processes and elements of the posterior column (articular process and facet joints, pedicle, lamina and spinous process) were not visible by the anterior approach.
Injury patterns identified by POCUS
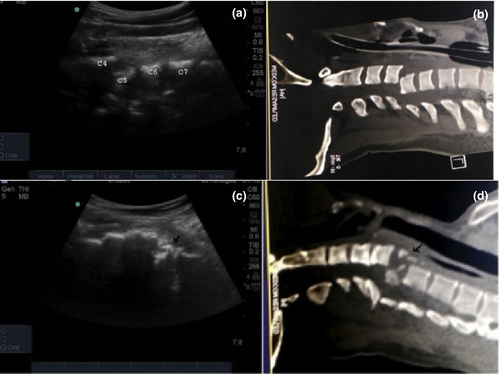
Vertebral body listhesis
POCUS identified 22/26 (84%) cases of listhesis. Out of 26 cases of listhesis, one had hangman’s fracture with C2-C3 listhesis which was not visible on POCUS. POCUS identified six out of seven cases of C4-C5 listhesis and eight out of nine cases with C5-C6 listhesis. POCUS detected all 8 cases of C6-C7 listhesis and missed one case of C7-T1 listhesis (Figure 4a,b).
There were 6 cases of false-positive listhesis. Three had vertebral body fractures in CT scan. Three had osteophytes and diffuse idiopathic skeletal hyperosteosis which was mimicking listhesis (Figure A2). These cases had presented after trauma and had neurologic deficits. The CT scan was negative for bony injury and listhesis. MRI revealed cord signal changes and prolapsed intervertebral disc and needed surgical intervention in those three patients.
The overall sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of POCUS vs CT scan for vertebral body listhesis are depicted in Table 2.
| Sensitivity | Specificity | PPV | NPV | |
|---|---|---|---|---|
| Vertebral body listhesis | 84.5% (65-95) | 89.7% (78-96) | 78.6% (62-88) | 92.9% (84-96) |
| Vertebral body fracture | 40.9% (20-63) | 96.8% (88-99) | 81.8% (51-95) | 82.2% (76-86) |
| Overall injuries | 45.8% (34-58) | 83.3% (51-97) | 94.3% (81-98) | 20.4% (15-26) |
| Excluding isolated posterior column injuries | 70.2% (55-82) | 83.3% (51-98) | 94.3% (82-98) | 41.7% (30-54) |
Vertebral body fractures
Out of 84 patients, 22 had vertebral body fractures diagnosed on CT. Of these, 9 cases were identified by POCUS. Most commonly involved vertebra in CT scan was C5 (n = 8) followed by C6 (n = 7), C2 (n = 6, odontoid fractures), C7 (n = 4), C4 (n = 4) and one case of C3 and C1. There were two false-positive cases in ultrasound where the vertebral body longitudinal length was reduced but CT showed no evidence of fracture (Figure 4c,d).
Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of POCUS vs CT scan for vertebral body fracture are depicted in Table 2.
Injuries not visible by POCUS
Injuries of the posterior column, transverse process fractures, pedicle fractures, upper cervical spine injury were not visible by POCUS but were identified by CT.
Performer feedback on image optimisation and quality
Likert scale analysis was done to correlate the quality of images acquired by the curvilinear probe and the linear probe. Quality of image was better with linear probe; however, the extent of visualisation of the vertebra was better with curvilinear probe (Table S1). Curvilinear had an advantage compared to the linear probe in assessing the alignment of vertebrae and providing a larger longitudinal plane of visualisation (Figure A3).
Discussion
C-spine injury with or without traumatic brain injury is an important health problem16 Early identification or clearance by using clinical decision rules and imaging like CT and MRI are key to management of C-spine injury.17 Emergency care providers use POCUS to make critical treatment decisions for acutely ill or injured patient in prehospital and ED settings. Airway manoeuvres in such patients may cause worsening of a hidden or undiagnosed cervical spine injury. Patients with a lesion above C5 level can present with respiratory distress due to involvement of diaphragm in which early intubation is necessary.
Previous case series from our centre assessed the feasibility of ultrasound in C-spine injury in the paediatric age group. C-spine fracture and dislocation were identified in a small sample size of 10 patients using the paediatric linear probe with an anterior approach.18 A recent study showed 74% sensitivity and 97% specificity of ultrasound in identifying cervical spine injury through anterior window.19 However, they did not define the normal anatomical landmarks of C-spine on ultrasound, the extent of visualisation through anterior window.20
Studies described the ultrasound anatomy of C-spine in ultrasound-guided facet joint injections. They used posterior and postero-lateral approach to delineate the bony landmarks and anatomy of C-spine. Sqarcia et al described the anterior sonographic window but the clinical utility through this approach was not described.21 Van Eard et al. described anterior window to be clinically irrelevant.22 We used only the anterior window to assess the cervical spine and found it reliable in assessing the alignment and anterior column injuries. We chose cricoid cartilage and C6 vertebra as a landmark for identification.
Visualisation of the extent and alignment of the vertebra was better with the curvilinear probe than the linear probe. Image quality was better with the linear probe compared to the curvilinear probe. The curvilinear probe has low frequency, high penetration and wider field of view makeing it suitable for a wider visual survey of C-spine in the anterior window approach. The previous study used only the linear probe and did not address the utility of curvilinear probe on image acquisition, optimisation and interpretation.18
The mean age and a predominantly male population of C-spine injuries in our study were comparable to other studies.23, 24 Injury level of C6 and C7 was predominant in our study. The association of traumatic brain injury with C-spine injury ranged from 10 to 30%.25-28 In our study, 14% was associated with traumatic brain injury and 8% with severe traumatic brain injury. Injury patterns visible by POCUS were body listhesis, vertebral body fractures, acute kyphotic angulation at the level of injury. Agrawal et al described a similar finding by POCUS in a case series of cervical spine injuries in the paediatric age group.18 Ojaghihaghighi et al. found high sensitivity and negative predictive value of ultrasonography in identifying fractured or dislocated C-spine.19
C4 vertebral body was visualised in 92% of patients compared to C5-C7 in 100%. Patient factors like obesity, oedema of the neck, and negotiating the probe cranially were the cause of non-visualisation of C4 in 8% of patients. C1 was not visualised in our study as we used only the anterior approach. Other studies reported the mastoid process as a landmark of C1 and it was only visualised in a Gelatin embedded model study and human studies have not mentioned about the visualisation of C1.22
POCUS identified 84% of body listhesis with high concordance rate compared to CT scan (p < 0.0001). Missed cases were one retrolisthesis, and two others had facet joint subluxation and grade I anterolisthesis which was visible in CT scan. One case of hangman fracture with C2-C3 listhesis was missed because the area was not visualised with POCUS. There were six false-positive cases of listhesis. Three had vertebral body fractures with the detached segment lying anteriorly which had an impression of vertebral body listhesis by ultrasound. The other three false-positive cases had multiple osteophytes and diffuse idiopathic skeletal hyperosteosis (DISH). POCUS showed distorted alignment and step up deformity in these patients. In these patients, CT scan was negative for injury and MRI showed cord signal changes and prolapsed intervertebral disc. Osteophytes and DISH were the potential confounding factors leading to a false-positive diagnosis of listhesis by ultrasound.
Out of 22 cases with vertebral body fractures, POCUS diagnosed nine cases. Three vertebral body fractures were diagnosed by POCUS as listhesis due to detached segment lying anteriorly. Two false-positive cases were diagnosed because of reduced longitudinal length of the vertebral body with age-related changes in CT scan.
The overall sensitivity of POCUS compared to CT scan was only 45.8% and specificity 83.3% with a positive predictive value of 94.3% (p = 0.06). After excluding isolated posterior column injuries, sensitivity was 70.2% (p = <0.05). Because of the high rate of missed injuries, POCUS at present cannot be used as a screening or diagnostic tool for decision-making in cervical spine injury.
However, the present study described a good positive predictive value of POCUS (92–100%) in identifying vertebral body fracture and listhesis between C4 and C7. The utility of identifying an unstable C-spine by POCUS during resuscitation as an adjunct may mandate the physician to take critical treatment decision in early intubation and use more advanced techniques like fibro-optic intubation or video-laryngoscope.
Limitations
Our study was only a feasibility study which was done in proven cases of cervical spine injury with small sample size. We used only the anterior approach of POCUS because the posterior window was not available for examination in acutely injured patients. Moreover, worsening of cervical injury by any manipulation of the neck was our outmost concern so the posterior window was not used and all patients were given manual in-line stabilisation during the study. We could not visualise injuries of the posterior column, transverse process fractures, pedicle fractures and injuries of C1 & C2. Future studies may focus on the inclusion of cervical spine assessment by POCUS as a part of the primary survey for trauma patients to validate the findings of study prospectively with large sample size.
Conclusion
This study described normal sonographic appearances of cervical spine and techniques of visualisation through anterior window. Injuries such as fracture and listhesis can be identified using this method. Curvilinear probe with wider field of view and better penetration makes it suitable to survey the C-spine from the anterior approach. However, the high rate of missed injuries makes POCUS an ineffective diagnostic tool for cervical spine injury and with the current limitations unlikely to change management or prevent progression to more advanced imaging modalities.
Funding
No funding information is provided.
Conflict of Interest
None declared.
Author Contributions
Vishnu VK: Conceptualisation (equal); Data curation (equal); Formal analysis (equal); Investigation (equal); Methodology (equal); Validation (equal); Writing-original draft (equal); Writing-review & editing (equal). Sanjeev Kumar Bhoi: Conceptualisation (equal); Data curation (equal); Methodology (equal); Visualisation (equal); Writing-review & editing (equal). Praveen Aggarwal: Methodology (equal); Validation (equal); Writing-review & editing (equal). L R Murmu: Writing-original draft (equal); Writing-review & editing (equal). Deepak Agrawal: Conceptualisation (equal); Formal analysis (equal); Methodology (equal); Supervision (equal); Visualisation (equal); Writing-review & editing (equal). Atin Kumar: Formal analysis (equal); Resources (equal); Supervision (equal); Writing-review & editing (equal). Tej Prakash Sinha: Conceptualisation (equal); Formal analysis (equal); Resources (equal); Supervision (equal). Sagar Galwankar: Supervision (equal).
APPENDIX