Using teeth as tools: Investigating the mother–infant dyad and developmental origins of health and disease hypothesis using vitamin D deficiency
Funding information: Ontario Research Fund Research Infrastructure (ORF-RI), Grant/Award Number: #29497; Canada Foundation for Innovation John R. Evans Leaders Fund (CFI-JELF); Ontario Graduate Scholarship, Grant/Award Number: N/A; SSHRC-CGS, Grant/Award Number: 767-2013-2678; The Canada Research Chairs program, Grant/Award Number: 231563; McMaster University; Canada Foundation for Innovation; Canada Research Chairs; SSHRC
Abstract
Objectives
With a growing interest in the mother–infant dyad and the Developmental Origins of Health and Disease hypothesis among biological and medical anthropologists, this study set out to provide all the information required to evaluate if mineralization defects in dentine might be caused by vitamin D deficiency in the critical first 1000 days of life.
Materials and Methods
Information was compiled on dentine formation in utero to approximately 18 years, and a method for determining the location of the neonatal line in dentine was devised, allowing the assessment of the prenatal and early life period. Re-evaluation of previously analyzed teeth (n = 61) was undertaken with detailed examination of n = 5/22 first permanent molars forming in the prenatal and critical early life periods.
Results
First permanent molars and all deciduous teeth give information on intrauterine development and on the first 1000 days postnatally providing a direct window on maternal and fetal health. Three archaeological individuals had interglobular dentine that formed prenatally suggesting that their mothers experienced vitamin D deficiency at the time dentine was forming and all other individuals had a deficiency during the first 1000 days of life. Conditions that could cause systemic mineralization defects were determined, and in each, case they were found to be consistent with vitamin D deficiency.
Discussion
The neonatal line serves as a clear baseline for determining prenatal and postnatal events, particularly those related to vitamin D, calcium, and phosphate metabolism, and can be used to investigate the maternal–infant dyad for both past and present communities.
1 INTRODUCTION
Teeth provide a permanent biological marker of metabolic stressors that disrupt mineralization in utero and early childhood. This is significant for both medical and biological anthropologists interested in the mother–infant dyad and the Developmental Origins of Health and Disease hypothesis (DOHaD), offering insights into maternal health and a means by which theoretical approaches linked to early life conditions that affect development can be tested and developed. DOHaD is a paradigm that explores how early life environments, particularly the intrauterine, affect the health and disease of individuals in later stages of the life course. Fetal programming is thought to be an adaptive process of the fetus to adverse environmental cues during gestation, which have long-term effects on physiology and metabolism and subsequent health status in later life (Barker, 1997; Pawley & Bishop, 2004). Early post-natal environment is equally important for disease in adulthood and the first 1000 days after conception are now widely recognized as a critical window (Elmadfa & Meyer, 2012).
The importance of DOHaD has been recognized by biological anthropologists. DeWitte and Stojanowski (2015) advocated consideration of fetal programming concepts in interpretations, and Gowland (2015) provides a theoretical overview for the application of this research to bioarchaeological problems. There has been growing recognition of the importance of the mother–infant dyad for understanding health in an immediate and evolutionary framework (Halcrow & Gowland, in press). Temple (2014) discusses conceptual frameworks and approaches that will enable bioarchaeological research to use early life stress events, and maternal–infant life histories to contribute discussions surrounding DOHaD. Medical anthropologists investigating the mother–infant dyad and DOHaD have considered how poor maternal nutrition and stress have long-term effects that increase the risk of disease in adulthood, and in recent years, there has been an appreciation for the use of teeth for such studies as evidenced by use of deciduous teeth in biobanks for biomedical research (e.g., Arora et al., 2017; Tvinnereim, Lygre, Haug, Schreuder, & Klock, 2012).
It is widely recognized that metabolic conditions, such as vitamin D deficiency, have an important role in bone and non-bone health (Lockau & Atkinson, 2018). Bioarchaeological researchers have sought to interpret the meaning of dental developmental stress markers in relation to the DOHaD concept using enamel defects (e.g., Temple, 2019), but knowledge about the impact of vitamin D deficiency on dentine during specific developmental periods is still limited. Recent developments in bioarchaeology and collaborations with those engaged in current health research prompted the authors to apply a “biological approach” to interpretation of dental lesions. Traditionally, the main conceptual approach to lesion identification in paleopathology has been comparative, where examples of known cases in a reference collection or published studies are compared with the cases under investigation (Mays, 2018a). This has clear strengths, but for conditions lacking known comparative samples, and those that are not well documented in the clinical science literature, the biological approach can offer a useful supplement. The biological approach involves, “Careful observation of the morphology and location of the lesions encountered in skeletal remains, coupled with a detailed reading of the biomedical literature whilst paying close attention to relationships between hard and soft tissue anatomical structures at the sites in the skeleton where lesions were characteristically seen” (Mays, 2018a, p. 18). As discussed by Mays in relation to the late Don Ortner, this approach was already used by some anthropologists. The explicit presentation of the approach as a clear framework marked a significant development for understanding conditions lacking clear comparative material.
Mineralization defects known as interglobular dentine (IGD) were first described in 1850 and experiments undertaken by Mellanby (1929) demonstrated that IGD formed in the teeth of puppies (Canis lupus familiaris) with experimental rickets (see Brickley et al., 2017). Recent work by D'Ortenzio et al. (2016) has shown that a range of conditions result in defects in the mineralization of dentine producing IGD, but the most common is vitamin D deficiency of nutritional origin (limited ultraviolet B [UVB] and/or dietary sources). D'Ortenzio and colleagues were able to demonstrate that IGD forms along incremental lines in dentine in those with skeletal evidence of an episode of rickets and also in living individuals with serum vitamin D (25-hydroxyvitamin D or 25(OH)D) levels below recommended levels (D'Ortenzio et al., 2018). Dentine in healthy individuals appears homogeneous with complete fusion of calcospherites (round spheres containing calcium salts), but in conditions with resultant mineralization defects, primarily vitamin D deficiency, some calcospherites fail to completely fuse leaving a poorly mineralized band of spherical or hemispheric-shaped spaces (Mishima & Kozawa, 1998). Systemic disturbances during tooth formation that affect mineralization may result in IGD located at the same developmental stage across contemporaneously forming teeth.
Given the importance of research into the DOHaD/first 1000 days hypotheses, better understanding the mother–infant pairing has become crucial. Investigations of dentine in deciduous teeth have provided significant information for bioarchaeologists (e.g., Beaumont et al., 2018) and biobanks are an excellent resource for modern groups. To expand potential research, a means of looking back at early life using adult dentition is needed. This article provides a framework through which those engaged in research on both past and present communities can integrate consideration of maternal and perinatal health, and questions affiliated to DOHaD, into their work. The aims of this study are threefold: (a) to provide a comprehensive re-assessment of conditions associated with IGD utilizing a biological approach for diagnosing disease; (b) to provide the first scheme that sets out clear information on the timing of dentine formation for the full dentition, enabling estimation of the chronological age at which IGD occurred; and (c) to present a method for use of IGD in conjunction with the neonatal line, providing a simple new way to identify individuals who experienced deficiency in the prenatal period.
2 MATERIALS AND METHODS
While clinicians have the advantage of conducting tests on living individuals to obtain a diagnosis of vitamin D deficiency, the same advantage is not available for those working with archaeological individuals, and such tests cannot be conducted retrospectively in clinical settings. One approach is to use IGD in tooth dentine, which forms incrementally and does not remodel, providing a permanent record of the quality of mineralization. We re-evaluated work undertaken by the team to date (D'Ortenzio et al., 2016; D'Ortenzio, Kahlon, Peacock, Salahuddin, & Brickley, 2018; D'Ortenzio, Ribot, et al., 2018) to address the paper's three aims.
2.1 Re-evaluation of available data
To date, our laboratory has published analysis of permanent teeth from 31 living and 30 archaeological individuals. Following Saunders, Chan, Kahlon, and Kluge (2007) procedures, teeth were embedded in resin (Epo-Thin) and sectioned using a Buehler IsoMet 1000 saw. The thin-sections were lapped and polished with a Buehler MiniMet grinder-polisher using graded grit paper and finished with diamond polish on a microcloth pad. Thin-sections were analyzed using polarizing microscopy, and images obtained using Keyence VHX1000 and Olympus BX51 microscopes. From the total group sampled, 18/61 individuals had IGD. We re-evaluated thin-sections of first permanent molars with IGD (n = 5/22), with the aim of now using the neonatal line as a marker for prenatal deficiency in one modern (M11) (HiREB ethics 2246), and four archaeological individuals from Saint-Matthews (n = 1) and Saint-Marie (n = 1), Quebec City, Canada (1771–1860), St. Antoine (n = 1), Quebec City, Canada (1799–1854), and St. Jacques (n = 1), France (1225–1798). The archaeological individuals had been identified as cases of past (healed) vitamin D deficiency (D'Ortenzio et al., 2016; D'Ortenzio, Kahlon, et al., 2018) on the basis of clear skeletal lesions and IGD. Age at which past episodes of deficiency occurred was approximated by assessing the location of IGD.
2.2 A biological approach to interglobular dentine
Utilizing a biological framework, the authors reexamined the available evidence relating to conditions that might cause IGD (factors that affect vitamin D, calcium, or phosphate metabolism, and the formation of mineralized tissues). We focused our research on conditions that could affect a pregnant woman and/or their offspring.
2.3 Chronology of dentine formation
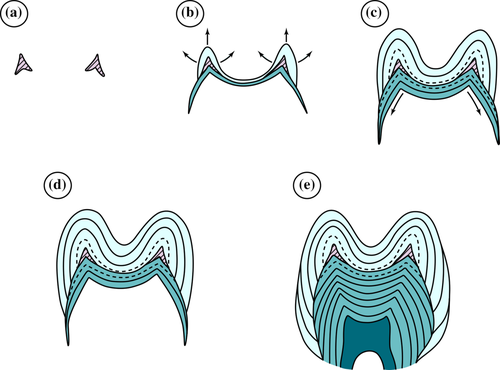
Chronological age can be estimated in the developing fetus and the postnatal period due to the regular incremental manner in which dentine is deposited. Similar to enamel, dentine follows a circadian rhythm. Growth of enamel and dentine is appositional, whereby dentine formation precedes enamel formation, and in permanent first molars, the cuspal portion of dentine, the horn, forms in utero (~30 weeks gestation) (see Figure 1a), (Schour, 1936) allowing prenatal vitamin D deficiency to be detected in adults. Dentine cells (odontoblasts) move inward, laying down dentine in an incremental pattern beginning at the tooth cusps in the crown that continue downwards until the tooth is fully formed (see Figure 1). Individual teeth have differing rates of growth and the incremental lines in dentine represent each time the rate of growth decreases or increases (Dean & Cole, 2014).
To date much of the work undertaken by dental anthropologists has focused on enamel. We undertook a review of information on dental development using data on incremental dentine growth in conjunction with well documented sources of initiation times for tooth mineralization and drew up the first diagrammatic scheme on incremental dentine development for all teeth in both the permanent and deciduous dentition. Sources used are listed in the caption of the resulting figure (see Section 3). Limited published data are available on the third permanent molar, which would be valuable for those wishing to explore a longer portion of the life course, and for this tooth we added data from our research. An average of all sources was taken to provide the estimated age when there was variation in original sources with respect to when a specific developmental stage is reached.
2.4 Locating the neonatal line in dentine
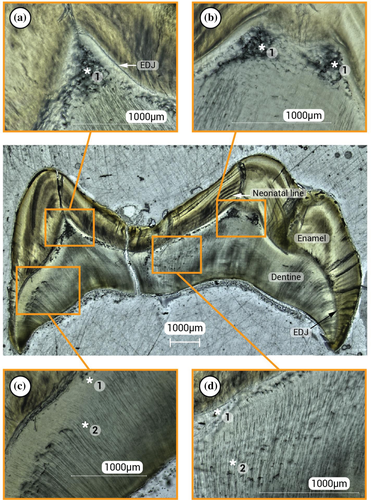
The birthing process leaves its mark in enamel and dentine observed as an accentuated incremental line called the neonatal line (Schour, 1936). This prominent microstructure separates enamel and dentine formed during intrauterine life from that formed after leaving the womb. Teeth developing prior to birth (portions of all deciduous teeth and the first permanent molars) exhibit a neonatal line which is visible in enamel as a dark, sharp band that is larger than the rest of the striae of Retzius (incremental growth lines or bands observed in enamel) (Eli, Sarnat, & Talmi, 1989). In dentine the neonatal line is observed as a narrow white line equidistant from the dentino–enamel junction (DEJ) and the neonatal line in enamel (Figure 2). The neonatal line is not always clearly visible in dentine, sometimes due to the thickness of the slide prepared (which can be dictated by tissue preservation) and in cases where IGD obliterates the neonatal line. Use of the new method described below aids in locating the neonatal line in dentine and the prenatal zone, a roughly triangular region of the dentine horn that is formed in utero in all teeth with a neonatal line.
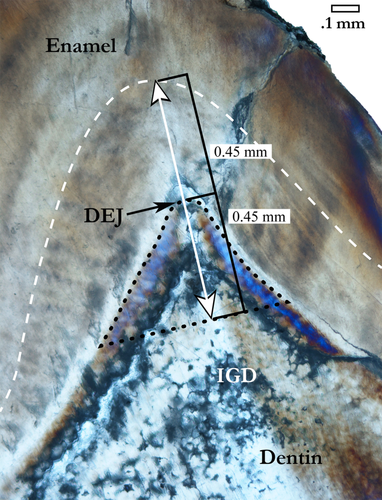
Images of sectioned teeth were uploaded into an ImageJ processing program. Using the Straight Line Tool each image was calibrated to the microscopic scale. As shown in Figure 2, a measurement was then taken from the neonatal line in the enamel to the DEJ. Next an equal distance was measured from the DEJ down into the dentine to create a reference point. For example, individual 15A-S36, had residual rickets and suffered from multiple episodes of deficiency during dental development and exhibited IGD that obliterated the neonatal line in his dentine. The measurement was 0.45 mm from the enamel neonatal line to the DEJ, so a reference point was set in the dentine at 0.45 mm from the DEJ, establishing the baseline for the prenatal zone of dentine.
3 RESULTS
3.1 Conditions causing interglobular dentine
Any condition that causes systemic mineralisation defects during dental development has the potential to cause IGD, and use of a biological approach to supplement any comparative material would enable researchers to establish if IGD might result from medical treatments or conditions not covered in Table 1. The framework presented by Mays (2018a) enabled the authors to see that some slight defects in dentine were merely developmental. Advice on differentiating normal dentine structures and slight mineralisation defects that can form during development was provided by D'Ortenzio, Kahlon, et al. (2018). The summary of conditions associated with mineralization defects provided by D'Ortenzio et al., 2016, (Table 1) provides a solid foundation for considering potential causes of IGD. However, our comprehensive re-assessment produced a fuller list and also factors in how relevant conditions are for living and archaeological individuals during dentine development (in utero to approximately 18 years) (Table 1).
| Condition | Description of condition | Relevance to past and modern groups |
|---|---|---|
| Nutritional rickets | Pathological changes to bone and teeth that occur due to metabolic imbalance in calcium, phosphate, and vitamin D. Results from an input insufficiency. Inadequate UVB exposure primary cause. | Commona in both groups; individuals survive and can recover if vitamin D reserves are restored. |
| Vitamin-D-dependent rickets, Type I, Type II, and Type III combined | Hereditary condition with low levels of calcium and phosphate; vitamin D cannot be absorbed adequately due to a metabolic defect. | Very rarea with no recovery. Potentially would not survive in the past. |
| Vitamin-D-resistant rickets (VDRR) | Different genetic disorders of phosphate and vitamin D metabolism that are resistant to treatments used for vitamin D deficiency. |
Very rarea with no recovery. Potentially would not survive in the past. |
| Autosomal-dominant hypophosphatemic rickets; X-linked hypophosphatemic rickets | Hereditary conditions characterized by defective intestinal absorption of calcium; is unresponsive to vitamin D. | Very rarea with no recovery. Potentially would not survive in the past. |
| Prader–Willi syndrome | Genetic disorder due to loss of function of specific genes is characterized by hypothalamic-pituitary abnormalities and growth hormone (GH) deficiency. Extreme erosive wear on teeth likely initiates growth of reparative dentine. | Very rarea genetic disorder. No recovery and obesity is a major factor influencing morbidity and mortality. High mortality rate without medical intervention. |
Fibroblast growth factor 23 (FGF23) |
Hereditary condition in which there is a malfunction in phosphate regulation. Phosphate is absorbed by the intestines and plays a role in regulating calcium and vitamin D. | Very rare.a Potentially would not survive in the past; can recover if phosphate levels are normalized with medical intervention. |
| Renal disorders | The kidneys regulate calcium levels by metabolizing vitamin D. The kidneys convert vitamin D to an active form and release into the gastrointestinal system to facilitate calcium absorption into the blood. Dysfunctional kidneys hinder this conversion. | Very rarea and recovery is dependent on severity of renal malfunction. Could live with it in the past, but children with severe renal failure require medical intervention (e.g., kidney transplant) not available in the past. |
| Celiac disease | Autoimmune disorder that occurs in genetically predisposed people where the ingestion of gluten leads to damage in the small intestine. Associated with malabsorption of calcium and vitamin D. | Commona with no recovery and could live with it in the past, but leads to a twofold increased risk of all-cause mortality even with medical intervention. |
| Crohn's disease | Chronic inflammatory bowel disease, primarily involving the small and large intestine; associated with malabsorption of vitamin D and calcium. | Relatively common.a No recovery and could live with it in the past, but if left untreated leads to complications (i.e., colorectal cancer, loss of weight and muscle mass, and nutrient deficiency). |
| Fluorosis | Chronic condition caused by excessive intake of fluorine. Risk factors associated with genetic susceptibility. Characterized by discoloration (brown staining). In severe cases pitting of the enamel and IGD form. | Commona in regions with high levels of naturally occurring fluoride. Found in both groups; can live with fluorosis and recover as long as toxic exposure removed. |
| Antibiotics | Toxic exposure to some antibiotics (e.g., amoxicillin) in experimental animal studies. | Use is common in modern groups; not applicable for past groups. |
- Note: Sources: Nutritional rickets and hereditary conditions (Brickley & Ives, 2008:88); FGF23 (Wolf, 2012); renal disorders (Ardissino et al., 2003; Hill et al., 2016); celiac disease (Peters, Askling, Gridley, Ekbom, & Linet, 2003; Al-Sharafi, Al-Imad, Shamshair, & Al-Faqeeh, 2014); Crohn's disease (Kalla, Ventham, Satsangi, & Arnott, 2014; Muhvić-Urek, Tomac-Stojmenović, & Mijandrušić-Sinčić, 2016); Prader–Willi syndrome (Saeves, Klinge, & Risnes, 2016); Fluorosis (Fejerskov, Yaeger, & Thylstrup, 1979; Littleton, 1999); Antibiotics (Laisi et al., 2009; Kumazawa, Sawada, Yanagisawa, & Shintani, 2012).
- Abbreviations: IGD, interglobular dentine; UVB, ultraviolet B.
- a Common represents >1/100; Relatively common represents >1/1000; Rare represents ~1/2000; Very rare represents ~1/25,000+ (based on prevalence rates) (NIH, 2017).
All conditions in Table 1 involve disruption of mineralization of tissues, normally either a deficiency in vitamin D or calcium, and/or phosphorus imbalance. Conditions affecting nutritional factors have been well studied. It is now clear for example that vitamin A is not the antirachitic factor in cod liver oil (Jones, 2012). Our review highlighted that celiac disease had been incorrectly included in the conditions not associated with IGD in D'Ortenzio et al. (2016, supplemental data), due to limited biomedical work. Childhood celiac disease has the potential to affect the intestinal absorption of calcium and vitamin D, which may result in IGD in developing teeth. Fluorosis was also listed with a note that globular dentine might form, which is potentially confusing. In the case of fluorosis, the key factor is the markedly increased lag time for mineralization of tissues due to toxic effects of fluoride on osteoblasts/odontoblasts (Boivin, Chavassieux, Chapuy, Baud, & Meunier, 1989). It is only in the cases of chronic fluorosis during dental development that IGD develops (Avery & El Nesr, 2001; Kuijpers, Van De Kooij, & Slootweg, 1996).
3.2 The chronology of dentine formation
Charts to facilitate the estimations of ages at which IGD formed in both the deciduous and permanent dentition were compiled (Figure 3a,b). In particular, we utilize the fact that a portion of human tooth dentine is laid down prior to birth (Avery, 2002) and indicated the approximate location of the neonatal line in all teeth where this would be present.
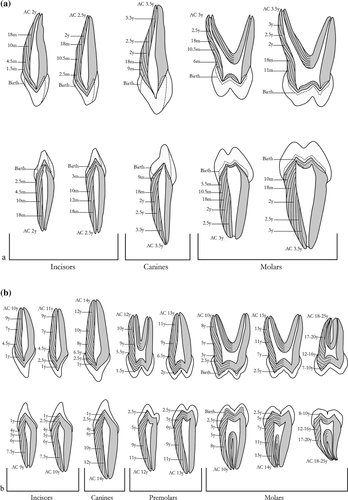
When utilizing deciduous teeth available in biobanks, one must be aware that tooth root resorption prior to natural exfoliation removes much of the dentine formed postnatally. As shown in Figure 3a, all deciduous teeth provide data on the intrauterine and post-natal environment with the canine tooth offering the greatest timescale of post-natal development once naturally exfoliated (Daito et al., 1991).
3.3 The neonatal line and re-evaluation of data using a biological framework
Results of the re-evaluation of the five first permanent molars with IGD using the new evaluation of neonatal line location are summarized Table 2. Ingestion of fluoride is the one condition that could resolve in archaeological individuals, but fluorosis is not present in any of the individuals' geographical regions (and no skeletal evidence has been identified at archaeological sites). All individuals had clear bands of IGD that resolved and normal dentine formation resumed. Thus, we propose that these cases of IGD represent the effects of nutritional vitamin D deficiency. The modern (M11) and one archaeological individual (STA18K55) had IGD, the location of which indicated deficiency occurred at ages ~1.4–2 (within the first 1000 days), and at 3 years, respectively. Three archaeological individuals (15A-S36, 2E4, SJ 970) had IGD in the prenatal zone of the dentine horns of the first permanent molars indicating that IGD developed in utero (Figure 3). The mothers of these individuals had a condition, mostly likely vitamin D deficiency, that caused IGD during pregnancy.
| Identifier | Tooth type | Initial evaluation of age of IGD (years) | New evaluation of IGD using neonatal line |
|---|---|---|---|
M11 (modern) |
LM1 | 1 episode at 1.4–2 yearsa | 1 episode: at 1.4–2 years |
2E4 (Saint-Marie, Quebec City, 1771–1860) |
RM1 | 1 episode at ~2 yearsa | 2 episodes: 1 Prenatal episode and 1 episode at ~2.5 years |
15A-S36 (St. Matthews, Quebec City, 1771–1860) |
RM1 | 2 episodes: 1.5–2 and 5.5 yearsb |
3 episodes: 1 Prenatal episode and 2 episodes at 1.5–2 and 5.5 years |
STA18K55 (St. Antoine, Quebec, 1799–1854) |
LM1 | 3 yearsa | 1 episode: at 3 years |
| SJ 970 (St. Jacques, France, A.D. 1225–1798) | LM1 | 1 episode at 1.5 yearsb | 2 episodes: 1 Prenatal episode and 1 episode at 1.5 years |
4 DISCUSSION
The DOHaD hypothesis proposes that the pre- and postnatal periods are a time when adverse environments can initiate long-term consequences for health from chronic non-communicable disease (Baird et al., 2017). The fetus adjusts its developmental trajectory in response to environmental cues. For example, in response to maternal vitamin D deficiency, a fetus may re-allocate resources to critical organs such as the brain by diverting them from organs or tissues with less critical metabolic needs (Gluckman, Hanson, & Buklijas, 2010). While doing so may be protective for the short-term, there are potential long-term negative consequences due to alteration in the structure and function of other important systems. Vitamin D plays a vital role during pregnancy as neonates are heavily dependent on maternal vitamin D due to its role in placental development and calcium transport (Lockau & Atkinson, 2018). In females with low 25(OH)D levels, the fetus is unable to obtain sufficient vitamin D for normal mineralization processes in utero, and shorter gestation duration affecting growth has been reported (Morley, Carlin, Pasco, & Wark, 2006).
4.1 Developing a biological framework
As can be seen in Table 1, most conditions that might lead to the formation of IGD are very rare. By far the most common condition associated with IGD is nutritional vitamin D deficiency. It has been estimated that over a billion people worldwide currently have vitamin D deficiency (Robinowitz, 2009) and prevalence rates were certainly higher among those living in cities in the Industrial Revolution when up to 90% of children were reported to have had rickets in some cities (Mays, 2018b). Recent work demonstrated that rickets was widespread at least 2000 years prior to the Industrial Revolution (Mays, Prowse, George, & Brickley, 2018) and it has been suggested that rapid human migrations and changes in lifeways have produced mismatches between the environment and skin pigmentation levels (Jablonski & Chaplin, 2018). Vitamin D deficiency has likely always been present in human societies.
Current health researchers and medical anthropologists studying vitamin D can ask living individuals about the following conditions: celiac disease, Crohn's disease, inflammatory bowel disease/ulcerative colitis, kidney disease, and genetic (inherited) causes of rickets. This questioning would be a simple way of excluding individuals that might have IGD caused by a condition other than nutritional deficiency. Information on local fluoride levels could be established with cases of fluorosis used as an exclusionary criterion.
While use of antibiotics is not a concern for archaeological individuals, they have been used to treat infections in modern pregnant women and infants. Acute doses of antibiotics in rats are thought to disrupt the normal maturation of the enamel resulting in mineralization defects (Muñoz et al., 2018), and have been shown to elicit a small but temporary reduction in osteoblast proliferation in bone (Philp, Raja, Philp, Newton Ede, & Jones, 2017). Further work is required but it is unlikely that temporary antibiotic use in a pregnant woman would cause IGD to develop in the fetus as the maternal immune system plays a critical role in shielding the fetal environment (Morelli, Mandal, Goldsmith, Kashani, & Ponzio, 2015). Infants would not receive levels required to produce IGD.
Non-nutritional causes of rickets, such as genetic conditions and other conditions in Table 1, will have an absence of resumption of normal dentine formation unless an effective treatment can be initiated. For the bioarchaeologist, if IGD is observed, the only two conditions that individuals would “recover” from are nutritional rickets and fluorosis. Skeletal fluorosis, in which there is increased density and ossification of sites of attachment of ligaments and tendons, occurs in the cases of prolonged exposure to high fluoride levels (Brickley & Mays, 2019). During tooth formation, alterations in enamel are greater than those occurring in dentine; IGD tends not to occur until fluorosis reaches a higher level of toxicity (Fejerskov et al., 1979). If skeletal changes are present, there would be less difficulty in deciding that fluorosis was the cause (Littleton, 1999). However, using only teeth, it is more difficult. Care should be taken in regions where fluoride levels are high.
Past individuals would not return to normal mineralization with the other conditions in Table 1. For example, if an individual developed celiac disease during tooth formation, one would expect IGD to coincide with the timing of the reduction in absorption of nutrients from the intestines which inhibit dental mineralization, and there would be an absence of incremental bands indicating recovery. In cases where there is a co-occurrence of nutritional rickets with another condition (i.e., fluorosis and celiac disease), dental evidence specific to vitamin D deficiency may be impossible to differentiate; assessment of skeletal lesions will assist in considering such cases. Cases with a clear return to normal mineralization are straightforward as with those examined using thin sections in the current study, or via Micro-CT analysis in the case of Veselka et al. (2019). In both studies, it was clear from the skeletal lesions that the rickets had healed prior to death. Assessment of possible causative factors will be more complex in non-adult individuals who died with active IGD/rickets.
4.2 Use of both deciduous and permanent dentitions
The focus on deciduous teeth in current health research (e.g., see Arora et al., 2017; Tvinnereim et al., 2012) has led medical and biological anthropologists to overlook the fact that both dentine and enamel in the permanent first molar begins to form in utero. Utero initiation of the first permanent molar is reported in the dental literature (e.g., Avery, 2002; Butler, 1967), but this basic piece of information is not readily available in sources commonly used by medical and biological anthropologists (e.g., Beaumont & Montgomery, 2015). As a result, deciduous teeth alone are commonly used to investigate in utero matters (e.g., Czermak, Schermelleh, & Lee-Thorp, 2018; Skinner & Dupras, 1993).
Cuspal denine in the first permanent molars will only fail to start forming in utero in exceptional circumstance (e.g., genetic disorders affecting dental development, see Seow, 2014). Evaluation of the neonatal line will allow the status of the individual to be elucidated. No line would indicate stillbirth or rapid death (Janardhanan, Umadethan, Biniraj, Kumar, & Rakesh, 2011) and patterns of IGD in relation to a neonatal line, if present, enables detailed consideration of the mother–infant dyad. Inclusion of the first permanent molar opens the possibility of retrospective study to current health researchers, and for those working with archaeological material greatly expands the potential for work on the mother-child pairing, through identification of maternal vitamin D deficiency.
4.3 Applications in research into the mother–infant dyad and DOHaD
This case study illustrates how the charts developed (Fig. 3a,b) will assist researchers to determine if IGD occurred within the first 1000 days, an important consideration in studies involving early life metabolic stressors. Clearly establishing the neonatal line and being able to determine if IGD occurred pre- or postnatally provides a window into the experiences of women in past communities, and will facilitate the posing of retrospective questions on in current groups. Vitamin D deficiency is produced from a confluence of biological and cultural factors, and the primary source is exposure of skin to sunlight. Latitude affects the UVB available, but cultural practices will influence variables such as clothing and time spent outdoors (Brickley, Moffat, & Watamaniuk, 2014). For example, crowded housing to accommodate the growing community developed in Quebec City in the 18th century, as people took advantage of the economic benefits of shipbuilding and the export of agricultural produce (Library and Archives Canada, 2016). Higher levels of UVB would have been available in summer; however, women covered themselves fully with clothing for modesty and to follow socially accepted norms associated with pregnancy and childbirth (Trakas, 2009). Figure 4 presents the re-evaluation of the first permanent molar of a child that died at three years having experienced vitamin D deficiency. Skeletal evaluation indicated that the rickets was healed at the time of death (D'Ortenzio et al., 2016), but the current investigation provides clear information that the individual experienced two episodes of deficiency, the first in utero (see Table 2), giving a basis for considering the mother–infant dyad in this community. Temple (2019) reviews ways in which bioarchaeologists could use evidence of adaptive plasticity through analysis of enamel defects such as linear enamel hypoplasia, to contribute to questions affiliated with DOHaD, and IGD could be approached in the same way. For most investigations a minimum of 400 individuals would be required. Choice of margin of error and level of confidence will determine the sample number required for a two group comparison (e.g., those with and without deficiency) with consideration of variables such as age-of-occurrence, age-at-death, or measures of growth and maturation. Statistical methods are available for investigations with different parameters (e.g., see Desu & Raghavarao, 1990).
Vitamin D deficiency is identified as a public health concern (Mulligan, Felton, Riek, & Bernal-Mizrachi, 2010). Use of the neonatal line, and tools set out in the paper, provide a unique opportunity to explore pregnancy, fetal health, and critical information on the mother-child pairing and questions affiliated with DOHaD in both past and present communities, opening avenues of research on those living prior to current health initiatives aimed at pregnant women (W.H.O., 2012). The approaches set out in this paper pave the way for generation of data that can be shared between the different fields of anthropology and also with biomedical and clinical researchers. Information on vitamin D deficiency can be integrated into debates surrounding the intimate relationship between perinatal and maternal health and used to examine the influence of early life deficiency on later health consequences.
ACKNOWLEDGMENTS
Sincere thanks to Isabelle Ribot from the University of Montreal, Quebec, Canada, and Benoit Bertrand from Lille University, Unité de Taphonomie Médico-Légale, Université, France, for supplying tooth samples for this project. We would also like to thank the living people who kindly donated their teeth and Professor Balakrishnan who gave advice on sample size estimation and Dr. Rebecca Gilmour who assisted in preparing Figs. 1–3. Thanks are owed to Victoria Lavallee who assisted with formatting references and Madeleine Mant who provided editorial assistance, and the editorial team and reviewers at AJPA who provided constructive comments on the initial draft of this paper. The research was funded by SSHRC-CGS (767-2013-2678), OGS, and the Canada Research Chairs program (231563), Canada Foundation for Innovation John R. Evans Leaders Fund (CFI-JELF), Ontario Research Fund Research Infrastructure (ORF-RI), and Institutional Support from McMaster University (#29497).
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.