Conducting clinical genomics research during the COVID-19 pandemic: Lessons learned from the CSER consortium experience
Funding information: National Human Genome Research Institute
Abstract
Clinical research studies have navigated many changes throughout the COVID-19 pandemic. We sought to describe the pandemic′s impact on research operations in the context of a clinical genomics research consortium that aimed to enroll a majority of participants from underrepresented populations. We interviewed (July to November 2020) and surveyed (May to August 2021) representatives of six projects in the Clinical Sequencing Evidence-Generating Research (CSER) consortium, which studies the implementation of genome sequencing in the clinical care of patients from populations that are underrepresented in genomics research or are medically underserved. Questions focused on COVID′s impact on participant recruitment, enrollment, and engagement, and the transition to teleresearch. Responses were combined and thematically analyzed. Projects described factors at the project, institutional, and community levels that affected their experiences. Project factors included the project′s progress at the pandemic′s onset, the urgency of in-person clinical care for the disease being studied, and the degree to which teleresearch procedures were already incorporated. Institutional and community factors included institutional guidance for research and clinical care and the burden of COVID on the local community. Overall, being responsive to community experiences and values was essential to how CSER navigated evolving challenges during the COVID-19 pandemic.
1 INTRODUCTION
The COVID-19 pandemic has led to significant changes across society and throughout the healthcare system. Shifting healthcare practices and priorities throughout the pandemic have had a major impact on clinical research and have affected every stage of the research process, from recruitment and consent through results disclosure and clinical follow-up.
Beginning in March 2020, many clinical studies were paused due to the pandemic for the safety of participants and research staff (Ledford, 2020; Waterhouse et al., 2020; Weinberg et al., 2020). Researchers who sought to continue recruitment needed to consider how to conduct their studies remotely. Many revised their protocols to allow teleresearch procedures such as video conferencing for participant interactions and e-signatures for informed consent (Rothwell et al., 2021; Stiles-Shields et al., 2020). In doing so, some had to navigate institutional policies and concerns about participant security and privacy when using online platforms (Loucks et al., 2021). Those that transitioned to remote procedures had mixed experiences with participant retention. While some participants found it easier to access and engage with researchers virtually, others found it difficult due to external stressors and other commitments. (Melvin et al., 2021 ) Study staff likewise needed to balance clinical and research priorities alongside home life and caretaking responsibilities exacerbated by the pandemic (Gilmartin et al., 2020). Furthermore, participants and researchers both experienced a learning curve adapting to virtual approaches that were sometimes novel (Loucks et al., 2021). These experiences throughout the pandemic have highlighted the importance of collaboration in research to facilitate the successful transition to remote procedures and the timely and widespread communication of clinical findings (Eke et al., 2021).
While a growing number of reports regarding the impact of COVID-19 on clinical research studies highlight the challenges and benefits of transitioning to teleresearch procedures, to date few have examined the unique features of consortium research—an increasingly common model of research in which multiple independent projects collaborate to address a shared set of questions—particularly in a clinical genomics setting. Here, we describe the experience of six genomic medicine studies conducted across 10 US states within the Clinical Sequencing Evidence-Generating Research (CSER) consortium throughout the COVID-19 pandemic. The CSER projects collectively aim to study the implementation of genomic medicine among marginalized, minoritized, and medically underserved populations (Amendola et al., 2018). We sought to understand what challenges these consortium projects faced, how they navigated them, and what lessons they have learned that may inform future genomics research, consortium research, and research in medically underserved settings. We give particular attention to two areas: (1) participant recruitment, enrollment, and engagement, and (2) the transition to telehealth and other remote research procedures.
2 METHODS
2.1 Editorial policies and ethical considerations
This study′s interviews and surveys were both determined not to be human subjects research by the institutional review boards at each institution involved in that portion of the project.
2.2 Study setting: The CSER consortium
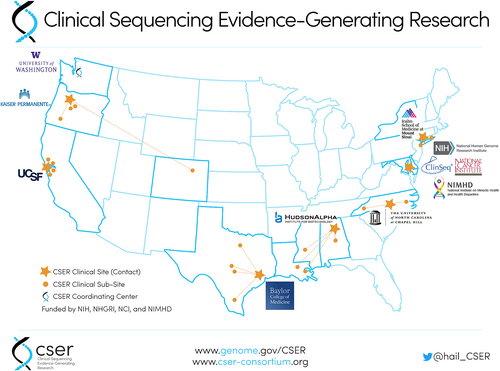
CSER is a multi-site research consortium funded by the National Human Genome Research Institute (NHGRI), the National Cancer Institute (NCI) and the National Institute on Minority Health and Health Disparities (NIMHD) (Amendola et al., 2018). The second phase of CSER, launched in 2017, includes six extramural projects that were ongoing at the start of the COVID-19 pandemic in March 2020. Each project studies the integration of genome sequencing into clinical care, prioritizing inclusion of individuals from populations that are traditionally underrepresented in genomics research or are medically underserved. Table 1 shows an overview of each project. Figure 1 illustrates the geographic location of each project and its sub-sites.
| Project | Lead site (location) | Population | Recruitment setting: Clinic type(s) | Recruitment setting: State(s) | Originally planned recruitment/enrollment strategies (prior to march 2020) | Additional recruitment/enrollment strategies (after march 2020) |
|---|---|---|---|---|---|---|
| CHARM | Kaiser Permanente Northwest (Portland, OR) | Adults at risk for hereditary cancer | Outpatient clinics | Oregon; Colorado | Email with text follow-up; in-person booth at select clinics; postcard with phone follow-up; provider referral (Mittendorf et al., 2021) | n/a (recruitment ended March 2020) |
| KidsCanSeq | Baylor College of Medicine (Houston, TX) | Children with cancer | Academic and non-academic medical centers and outpatient clinics | Texas | In-person recruitment by study staff for in-patients and during clinic visits | Phone recruitment by study staff |
| NCGENES 2 | University of North Carolina at Chapel Hill (Chapel Hill, NC) | Children with suspected genetic conditions | Outpatient pediatric genetic and neurology clinics at academic medical centers and community hospitals | North Carolina | Introductory letter mailing with phone follow-up; in-person enrollment following clinic visit | Remote research visits via phone/video with mailed signed consent/HIPAA documents |
| NYCKidSeq | Icahn School of Medicine at Mount Sinai (New York, NY) | Children with suspected neurologic, immunologic, and cardiac genetic conditions | Academic and non-academic medical centers | New York | Provider referral during in-person clinic visits; some in-person study staff recruitment; all study appointments scheduled by study staff by phone | Provider referral during in-person or telehealth visits; no study staff recruitment; all study appointments scheduled by study staff by phone |
| P3EGS | University of California, San Francisco (San Francisco, CA) | Pregnancies with abnormal ultrasound findings and children with suspected genetic conditions | Academic medical center, outpatient clinics, NICUs, PICUs, community hospital | California | Provider referral at in-person clinic visits followed by in-person enrollment visit with study staff | Telehealth enrollment for pediatric patients with enrollment materials sent in advance by postal mail; some prenatal patients enrolled at in-person clinic visits; additional information collected by phone |
| SouthSeq | HudsonAlpha Institute for Biotechnology (Huntsville, AL) | Newborns with suspected genetic conditions | Academic and non-academic medical centers, women′s hospital, children′s hospitals, NICUs, prenatal clinical, and pediatric unit | Alabama; Kentucky; Louisiana; Mississippi | Provider referral to research nurses who contacted parents in NICU with phone or videoconference follow up by research team; enrollment and initial data collection conducted remotely via custom online platform | Increased use of video conferencing and telehealth visits |
2.3 Data collection and analysis
We used a mixed methods approach including semi-structured interviews and surveys to collect information about projects′ experiences.
We first interviewed principal investigators and project managers from each project about their projects′ experiences implementing their research projects, including their experiences during COVID. Project investigators and managers were nominated for the interview by other members of their project and interviewed by a trained interviewer from a different CSER project. The primary purpose of these interviews was to explore the challenges and successes associated with starting multi-institutional projects recruiting underserved and underrepresented populations. At the end of each interview, we asked about “experiences running your project as the COVID pandemic evolved,” with prompts for changing or ending a part of their project, an explanation of essential research activities, and differences between the multiple institutions participating in their project. Interviews were conducted via video conferencing and were recorded and transcribed verbatim (otter.ai, Mountainview, CA). Interview transcripts were thematically analyzed using an iterative, consensus approach including development of a thematic dictionary, dual coding of transcripts, and deliberation and consensus-building around discrepancies (Patton, 2002). Any interview responses related to the pandemic were excerpted and analyzed as part of this study; other responses were not included in this analysis.
To better understand the experiences of each project with respect to key issues raised in the interviews, we also administered a follow-up survey to each project. The survey format allowed project teams to develop collaborative responses that reflected multiple team members′ perspectives. Representatives from each of the six extramural CSER projects and the NIH developed initial domains for survey questions based on review of projects′ responses to Quarterly Project Reports submitted to the NIH between March and December 2020 as well as an internal consortium list of questions about the impact of COVID-19 on projects in April 2020. We then reviewed preliminary analyses of the interviews described above and narrowed our survey domains to two key areas for further exploration: (1) the impact of the pandemic on participant recruitment, enrollment, and engagement, and (2) the transition to telehealth and other remote research procedures. We drafted summaries of projects′ prior responses within each of these domains and developed targeted, primarily open-ended survey questions about additional impacts and future plans in these domains (see Appendix S1).
Each project representative facilitated the completion of their project′s survey responses through a combination of targeted emails to key project staff or principal investigators, general team emails, and presentation/discussion on project team calls. Completed surveys were submitted by email to our small team. Two authors (SAK, KR) sorted interview and survey responses according to the thematic categories identified by the interview team to facilitate review for cross-cutting themes. Our team then discussed the data to further refine the categories and identify general lessons learned across projects as well as unique experiences reported by specific projects.
3 RESULTS
We interviewed six principal investigators and seven project managers, collectively representing all six extramural CSER projects, between July and November 2020, and surveyed representatives of all six projects between May and August 2021. Through these interviews and surveys, we identified factors at the project level as well as at the institutional and community levels that affected projects′ experiences of the COVID-19 pandemic. Exemplar quotes are shown in Table 2.
| Factor | Exemplar quote(s) |
|---|---|
| Project factors | |
| Progress at onset of pandemic | “So we have started enrollment in February, or January [of 2020]. We then subsequently had [a] four week hiatus, scheduled a patient and promptly COVID happened. And we, and the patient did not come and we stopped research. And here we are six months later, starting enrollment again.” (Project C, interview) |
| Urgency of in-person clinical care | “We had permission to enroll only if it was a patient where the tumor results were felt to be particularly important. But because we are on this clinical research interface, we were one of the first studies to be reopened.” (Project B, interview) “[Our project] was not ‘essential research’ for the most part; with the exception of prenatal patients who needed to continue with in-patient visits for clinical care and/or labor and delivery. We had to do everything remotely for the non-essential research part.” (Project E, survey) |
| Prior incorporation of remote research procedures | “Our study was designed from the beginning to be very virtual. So the consent, the risk assessment, all the surveys, everything is online. We were using saliva kits already. The counseling is done by phone. … Participants never need to come in for any reason, and so we did not have to do any adaptation for those reasons.” (Project A, interview) |
| Institutional and community factors | |
| Institutional guidance for research and clinical care | “[P]hone consent was IRB approved prior to the pandemic, but it was only for the secondary parent and after initial discussion with the primary parent in person. The IRB was amended to allow the initial discussion with primary parent to occur via phone if needed.” (Project B, survey) “The nurses, some of them just could not get into the unit, because they are solely research nurses. And they had kind of stopped all research for a while. And then some of the nurses who have both clinical and research duties were able to get in.” (Project F, interview) |
| Burden of COVID on local community | “We are seeing more disconnected phones, you know. Potentially people cannot pay their bills, people have moved in with relatives, people who are no longer where they were, you know, it′s a challenge.” (Project C, interview) “We had a couple of cases where the primary parent involved in the beginning and answering the surveys, you know, wasn′t there anymore on when comes returning result, because they were intubated at a hospital because of COVID. Right. So like, I think that we have heavily, you know, our population has been heavily impacted by COVID.” (Project D, Interview) |
3.1 Project factors
Project-level factors included the progress of the project at the onset of the pandemic, the urgency of in-person clinical care for the disease being studied, and the degree to which the project had previously incorporated remote research procedures.
First, the impact of the pandemic on enrollment varied across projects depending on how recently recruitment had begun. Although all projects were funded via CSER at the same time, each project had a distinct patient population and design that impacted recruitment prior to the pandemic. One project that met their recruitment goals prior to the pandemic noted that “we were incredibly fortunate that we ended recruitment two weeks after our lockdown notice from our state” (Project A, interview) whereas others were in the middle or early stages of recruitment. Two projects had initial recruitment delays before the pandemic and indicated that COVID caused further slow-downs. The other three projects reported that they were able to navigate the impacts of COVID, for example, by having individual sites decide whether to continue enrollment or bringing on additional sites as planned before the pandemic.
Second, the impact on research activities was affected by the perceived clinical urgency of the disease being studied. Several projects noted that recruitment during the pandemic was dependent on whether patients′ conditions were deemed to be “urgent” or “essential” enough to warrant in-person care, although these terms were not clearly defined. For example, enrollment was made available to prenatal care patients, babies in the neonatal intensive care unit, and pediatric cancer patients with “particularly important” tumor results. One project stated that theirs was among the first in their institution to restart recruitment after an initial pause due to their integration with routine clinical care. However, projects that relied on recruitment of patients attending outpatient visits were more limited; one project reported that patients who fit their phenotypic eligibility criteria were often defined as non-urgent thus these visits were rescheduled or postponed during the early months of the pandemic, and another commented that patients with chronic conditions were not coming into the hospital or health center and were “uncomfortable to do that in COVID times” (Project D, interview). Similarly, a project conducting population screening on healthy adults noted that their cost and utilization analyses might be affected as a consequence of patients avoiding non-urgent clinic visits, raising more general concerns about access to downstream care after a positive genetic result.
Third, the degree to which the project was conducted in-person or remotely prior to the pandemic affected the project′s response. All projects had to navigate moving participant-facing procedures and/or the underlying workflows to incorporate remote research. Prior use of remote research procedures simplified the projects′ ability to transition quickly to the need to be primarily remote. For example, one project that already used remote consent, emailed surveys, and disclosed results by telehealth reported a mostly smooth transition, but identified challenges for the project team regarding remote access to protected health information (PHI) and distribution of participant incentives. Other types of remote procedures that were commonly already in place included telehealth services and mailed letters for non-significant genetic test results. Several projects reported that, early in the pandemic, they quickly added an option to obtain consent by phone, and several sent materials (e.g., consent forms, saliva kits, surveys) by postal mail, though projects reported varying success with responses to mailed materials. A project in the pediatric setting noted that limits on how many parents could attend a visit meant that follow-up discussions with a second parent needed to take place by phone.
Most projects noted some increased efficiencies from using remote procedures and one commented that the widespread use of video conferencing platforms for school and other activities meant that participants were increasingly familiar with this technology. However, they also noted challenges including increased logistical burdens on project team members, lack of participant access to necessary technologies (e.g., computers, broadband), increased time and effort for follow-ups with non-responders, and distractions or other difficulties with engagement during virtual recruitment visits as compared to in-clinic recruitment. Finally, upon the transition to teleresearch, one project needed to revise its planned trial of an in-person results delivery intervention that was no longer feasible in an entirely remote environment, replacing it with a pilot study to improve delivery of genomic results via telehealth.
3.2 Institutional and community factors
Institutional and community factors reflected the decisions and policies of the healthcare institution as well as its local context. Factors included institutional guidance for research and clinical care and the burden of COVID on the local community.
First, guidance from various institutional human subjects research and clinical sources affected projects′ responses to the pandemic. Several project Institutional Review Boards (IRBs) facilitated rapid transitions to teleresearch procedures and “quickly approv[ed] changes that would keep our studies going” (Project D, interview), particularly for results disclosure and study enrollment. However, at times some projects had to undergo lengthy review processes, for example when a community-based site was under separate IRB oversight from the project′s lead institution, or when a standardized COVID information sheet that had been globally approved for all studies at the lead institution needed to be revised to reflect the COVID precautions at the project′s partner institution. One project had to halt recruitment of children who were capable of assent for several months due to a pre-existing IRB requirement for in-person assent, which precluded phone consent for this group of parents and children. Ultimately the team was able to receive approval for a remote assent protocol as an amendment to their IRB protocol.
Institutional rules implemented in response to COVID-19 at the clinical study sites also affected recruitment in some cases. Many clinical sites had a temporary pause on research; one project representative noted, “I think that was just so they could catch their breath and figure out what is appropriate and what is not” (Project F, interview). At one project, recruitment was closed for several months in response to the significant impact on the region early in the pandemic. Reductions in non-urgent outpatient visits, reassigning clinicians and staff to COVID wards, and minimizing presence of non-essential personnel (i.e., recruiters) in clinical settings for infection prevention purposes also impacted enrollment. For example, a project in the inpatient setting reported that their research nurses were not allowed into the hospital for a period of time unless they also had clinical duties. As research opened back up, institutions continued to play a role. One project noted a variable pace of reopening and staffing capacity across clinics, resulting in reevaluation of recruitment resources in each clinic. A project in the outpatient pediatric setting identified visitor limits at clinical appointments as a source of increased canceled visits or no-shows, as some families who needed to arrange childcare for other children during clinic visits were unable to do so. Another project reported being required to implement a research-specific COVID screening protocol for all participant visits. Finally, general rules around handling and storing PHI at one project′s lead institution created challenges for team members to access PHI at home, make participant phone calls outside of the office, and print out reports to mail to participants.
Beyond institutional policies, projects′ experiences were also shaped by the broader context and burden of COVID in their local communities and on their participants. Some sites noted differences in enrollment across their clinical sites because of the variable impact of COVID; for example, one project reported that their lead institution closed enrollment for a time but that their partner sites did not. Projects also noted changes in participants′ priorities. One project noted an increase in disconnected phone lines among their participants and described financial and childcare challenges that for at least some participants took priority over research participation. In some cases, priorities evolved over time; one project reported an uptick in survey responses initially when participants had more time, but that it was harder to get people to come in later on, which they hypothesized might be due to fatigue or fear of the hospital. The New York City-based project stated that “our population has been heavily impacted by COVID,” with some participants and their families directly affected by a COVID diagnosis. Beyond COVID itself, they also discussed the impact of the Black Lives Matter movement on their participants, stating that for some families “they just were overwhelmed and not really willing or wanting to receive [results] in this moment. And we had to respect that.” The team subsequently published a statement on their project website in support of underrepresented and minoritized communities (https://nyckidseq.org/).
4 DISCUSSION
The experiences of these six CSER consortium projects during the COVID pandemic illustrate several key challenges that clinical genomics research studies have faced during this time and offer insights into how research projects can promote ethical and equitable research as they move forward from the pandemic. Lessons learned relate to the use of telehealth and remote research approaches, the impact of institutional guidance and research oversight on research at the clinical-research boundary, and the need to be responsive to community experiences and values.
First, the transition to teleresearch created logistical burdens for many projects, but once up and running, remote procedures created some efficiencies and allowed most projects to continue with recruitment. However, while many participants gained comfort with video conferencing technologies during the pandemic, access barriers remain that illustrate the importance of in-person recruitment in certain settings, such as in the case of child–parent dyads or for populations who lack reliable internet access. These experiences mirror the transition to telehealth genetic counseling more generally during the COVID pandemic (Mills et al., 2021) and align with prior work showing that telehealth genetic counseling increases efficiencies but may also be difficult for some patients to access (Danylchuk et al., 2021; Gorrie et al., 2021). For example, in one survey study, patients reported that virtual genetic counseling visits were generally satisfactory, but a majority of those surveyed still preferred a hybrid telehealth/in-person approach moving forward (Dratch et al., 2021). The experiences of CSER, considered alongside the broader genetic counseling literature, suggest that teleresearch procedures can be valuable tools to facilitate access to clinical genomics research and minimize disruption in case of emergencies that prevent participants from accessing clinical sites in person, research team members from working in an office setting, or both. However, maintaining the ability to offer in-person approaches is still important to ensure equitable research access for those who lack the technology and/or ability to use telehealth. As researchers plan future projects, they should consider what types of options for virtual or remote processes will best meet the needs of their target populations in the context of their clinical settings. Individual projects as well as research consortia should also consider creating contingency plans upfront to minimize logistical changes and approvals should the need arise to change approaches after a project is already underway, building on existing recommendations and examples such as the National Academy of Science′s recommendations for disaster resilience for biomedical research (National Academies of Sciences, Engineering, and Medicine, Division on Earth and Life Studies, Health and Medicine Division, Institute for Laboratory Animal Research, Board on Earth Sciences and Resources, Board on Health Sciences Policy, Committee on Strengthening the Disaster Resilience of Academic Research Communities, 2017) or the emergency response standard operating procedures developed by one consortium of biobanks (Schmelz et al., 2021). To further support equitable access to research, future research should examine the benefits and limitations of different in-person and remote approaches (e.g., audio-only phone calls vs. video calls). For example, in recognition of the value of telehealth both during and beyond the pandemic, one CSER study modified its research aims to compare the impact of telehealth delivery models in genetic counseling. Ongoing work like this will be needed to optimize the delivery of telehealth methods in both clinical care and research, including in what circumstances teleresearch is appropriate as either a standalone or hybrid approach. Additionally, funders should provide resources to ensure research teams and institutions can build appropriate infrastructure and tools to support equitable access.
Second, it is not surprising that institutions varied in their responses to the conduct of research during this unprecedented event, and the variability across institutions was particularly noticeable in the setting of a nationwide research consortium. Institutional guidance about both research and clinical care, and sometimes variations across sites and/or lack of clarity around definitions, greatly influenced how CSER projects experienced the pandemic. The implementation of IRB processes to facilitate a rapid transition to remote procedures was one approach that many projects identified as helpful. A study of research protocols reviewed by IRBs early in the pandemic showed that many IRBs achieved relatively rapid review by adjusting administrative workflows and adding extra meetings (Taylor et al., 2021). In anticipation of future emergencies, IRBs should review the impacts of their processes and identify opportunities to further develop and improve guidance that is flexible, responsive, and clear for researchers.
Additionally, the pandemic amplified the complexities of conducting research at the clinical-research boundary (Halverson et al., 2020; Wolf et al., 2018). Projects′ experiences raised questions about what research activities do, or should, count as essential. A study of clinical research units across the US reported a general definition of essential research as “research that is essential to a participant′s health and/or well-being,” (Subramain et al., 2021) but the experience of the CSER projects suggests that this definition was not always straightforward to apply in practice, particularly in the setting of a nationwide research consortium. Projects took place in a range of clinical contexts, and recruitment during COVID was affected by changes in which patients were able to attend clinical visits as well as decisions about whether the research itself should continue. Even when research was allowed to continue, projects′ experiences highlighted the new barriers that some participants faced in accessing research, for example, visitor limitation policies, on top of pre-existing access barriers to both genomic medicine and research (Gutierrez et al., 2021). CSER project representatives discussed their observations of how these policies affected participants′ experiences, raising important questions for analysis as to whether these types of access barriers disproportionately impacted participants from underrepresented or underserved populations or recruitment of individuals from these groups. These observations also raise important questions about the downstream impacts on access to care and services stemming from delays in genomic testing.
Finally, our projects′ experiences show the importance of prioritizing and responding to the evolving needs of their participants and broader communities. The CSER projects′ experiences provide six examples of studies enrolling distinct, often underserved clinical populations and adjusting processes, procedures, and goals according to the specific needs of those populations, facilitated in some cases through engagement with local patient and community partners. The pandemic highlighted, and sometimes worsened, many long-standing issues in research, for example, access barriers related to technology and childcare. It also imposed new burdens and barriers on individuals and communities that amplified significant existing disparities in research, healthcare, and society. To advance genomic medicine research that produces equitable benefits, researchers will need to understand the long-lasting impacts of the pandemic on the patient populations they intend to work with, proactively address known barriers that have been highlighted or exacerbated during the pandemic, and be attuned to barriers that may arise in the future. Investing in community stakeholder engagement will be a critical component of understanding key issues and developing potential solutions.
5 LIMITATIONS
This article describes the experiences of six genomic medicine studies during the COVID pandemic and highlights several critical operational issues for clinical research. While not generalizable to all research, it offers an illustrative example of how projects within one research consortium responded and are navigating moving forward. Because projects were at varying points in recruitment and each had multiple factors unrelated to the pandemic that also affected their enrollment rates, we do not report the impact of the pandemic on enrollment. This article also does not examine the perspectives of participants, which will be invaluable in considering the full picture of the impact of COVID on research and should be the subject of future analyses by CSER projects and others.
6 CONCLUSION
The experiences of these six CSER projects illustrate a range of factors that have affected clinical genomics research studies throughout the COVID-19 pandemic, highlighting the importance of recognizing the unique clinical setting, institutional context, and local community in which each project within a research consortium takes place. Our findings related to the implementation of teleresearch procedures, impact of institutional guidance, and responsiveness to community needs offer insight into some of the challenges that have arisen or been amplified during the pandemic. They also offer opportunities to anticipate and address potential issues as we strive to conduct ethical and equitable genomics research moving forward.
ACKNOWLEDGMENTS
The Clinical Sequencing Evidence-Generating Research (CSER) consortium is funded by the National Human Genome Research Institute (NHGRI) with co-funding from the National Institute on Minority Health and Health Disparities (NIMHD) and the National Cancer Institute (NCI), supported by U01HG006487 (UNC, supporting JTB and MW), U01HG007292 (KPNW, supporting SAK and JMZ), U01HG009610 (Mt Sinai, supporting KEB and CRH), U01HG006485 (BCM, supporting HR and JOR), U01HG009599 (UCSF, supporting NS-H), U01HG007301 (HudsonAlpha, supporting SJK), and U24HG007307 (Coordinating Center). The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. KR, LAH, and DK are members of the NIH Staff Team, responsible for scientific management of the CSER program. The CSER consortium thanks the staff and participants of all CSER studies for their important contributions and the community stakeholders who provide guidance. In particular, the authors thank Hadley Stevens Smith for contributions to interview analysis. More information about CSER can be found at https://cser-consortium.org/. CSER Diversity and Inclusion Statement: In CSER, we aim to improve the use of genetic information in medicine and reduce barriers to genetic services among underserved groups. Our research seeks to better understand connections between genes, other drivers of health and disease, and health outcomes. We have worked with study participants and community partners to help make our research more inclusive. We still have much more work to do to ensure that our findings are applied in fair and just ways. We also acknowledge the need for more diversity among our own researchers. As we publish the results of CSER, we commit to carrying efforts forward to make sure people of all backgrounds benefit from genomics research and medicine.
CONFLICT OF INTEREST
The authors declare no conflicts of interest related to this work.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.