Broadening the phenotypic spectrum of EVEN-PLUS syndrome through identification of HSPA9 pathogenic variants in the original EVE dysplasia family and two sibs with milder facial phenotype
Funding information: Raregenomics network, Grant/Award Number: S2017/BMD-3721; Proyecto Piloto para la mejora del diagnóstico genético en personas y familias afectadas o con sospecha de padecer enfermedades raras de base genética, Grant/Award Number: BOCM-20181126-24; AES, ISCIII, Grant/Award Number: PI19/01681; Whole Exome Sequencing protocol inpediatric patients admitted to critical or highly complex units
Abstract
EVEN-PLUS syndrome is a rare autosomal recessive disorder caused by biallelic pathogenic variants in the mitochondrial chaperone called mortalin, encoded by HSPA9. This genetic disorder, presenting with several overlapping features with CODAS syndrome, is characterized by the involvement of the Epiphyses, Vertebrae, Ears, and Nose (EVEN), PLUS associated findings. Only five individuals presenting with the EVEN-PLUS phenotype and biallelic variants in HSPA9 have been published. Here, we expand the phenotypic and molecular spectrum associated with this disorder, reporting two sibs with a milder phenotype and compound heterozygous pathogenic variants (a recurrent variant and a novel one). Also, we confirm a homozygous pathogenic variant in the family originally reported as EVE dysplasia.
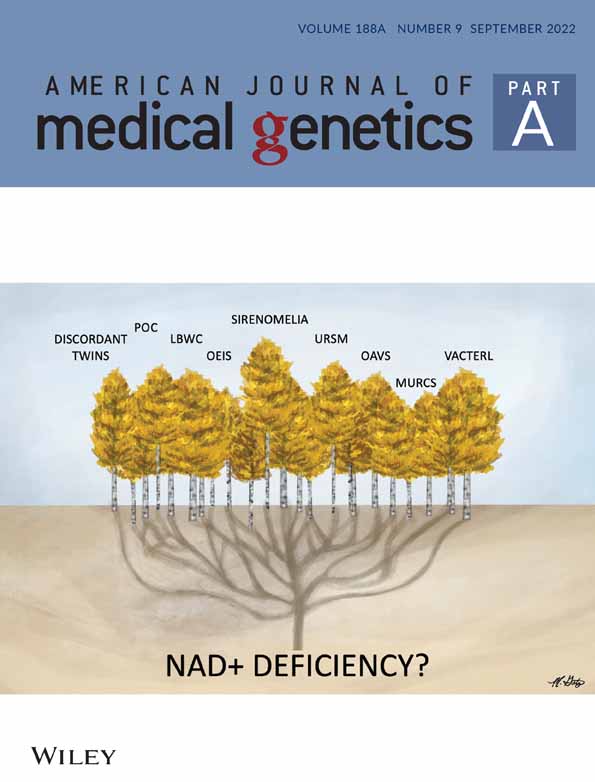
1 INTRODUCTION
EVEN-PLUS syndrome (MIM 616854) is a rare autosomal recessive disorder characterized by the involvement of the Epiphyses, Vertebrae, Ears, and Nose (EVEN), PLUS associated findings.
Amiel et al. (1999) reported two sisters with an unusual combination of malformations including epiphyseal, vertebral dysplasia, and ear anomalies. They pointed out the similarity with CODAS syndrome (Cerebral, Ocular, Dental, Auricular, and Skeletal findings; MIM 600373), particularly the bone anomalies such as delayed bone age, epiphyseal dysplasia, and vertebral clefts. However, the absence of additional features related to CODAS syndrome, namely neonatal hypotonia, postnatal growth retardation, intellectual disability, and eye and dental anomalies led them to consider it a distinctive condition and proposed the name “EVE (Epiphyseal, Vertebral, and Ear) dysplasia.”
Subsequently, Royer-Bertrand et al. (2015) reported three individuals with a CODAS syndrome-related phenotype without pathogenic variants in LONP1, responsible for this disorder. Instead, they identified biallelic alterations in HSPA9 in the three affected cases. These authors also noticed the similarity of the skeletal findings between these patients and those with CODAS syndrome. However, they remarked a very distinct craniofacial phenotype with microtia, a flat facial profile with flat nose and triangular nares as well as other findings such as congenital heart defects, anorectal anomalies, hypodontia, and aplasia cutis and suggested the name of “EVEN-PLUS syndrome” to include the nose and the other associated findings.
Further on, Nagrani et al. (2018) and Younger et al. (2020) described two additional patients with EVEN-PLUS syndrome and biallelic variants in HSPA9, helping to delineate and expand the phenotype associated with this rare disorder and confirming the involvement of HSPA9.
HSPA9 encodes a highly conserved mitochondrial chaperone called mHSP70/mortalin, essential for mitochondrial protein import from the cytosol to the mitochondrial matrix, as well as for their folding and degradation, preventing accumulation of unfolded dysfunctional proteins.
So far, five individuals have been described in the scientific literature with EVEN-PLUS syndrome and biallelic pathogenic variants in HSPA9. The aim of the present work is to report two additional sibs showing the distinctive radiological findings of EVEN-PLUS syndrome, but with milder facial features. We report biallelic variants in HSPA9 in these individuals, and in the original EVE dysplasia family. In addition, we review the clinical features of these cases and those described in the literature to refine the phenotype associated with this rare disorder, and we provide in silico 3D modeling data to support the pathogenicity of the unreported variants.
2 CASE REPORTS
2.1 Family one
Patient 1 is a female, second child of non-consanguineous healthy Caucasian parents, who had a similarly affected older brother (see Patient 2 below). She was born at term (41 weeks) following an uneventful pregnancy by repeat cesarean section. Apgar scores were 7 and 10 at 1 and 5 min, respectively. Her birth weight was 4240 g (27th centile), length 52 cm (65th centile), and head circumference 36.5 cm (49th centile). Neonatal examination showed an imperforate anus and bilateral microtia with a patent external auditory canal. Abdominal and lumbar ultrasound (US) showed no associated renal or sacral anomalies. A diverting colostomy was performed in the first 24 h of life. She passed the neonatal screening hearing test. Initial investigations included a customized 60K array-CGH (KaryoArray v3.0, Agilent) with normal results. The diagnostic possibility of Townes-Brocks syndrome was considered. A customized 1387 gene NGS panel for neurodevelopmental disorders and other common genetic disorders including SALL1 was performed, showing no alterations in the genes analyzed. Her development was normal. A posterior anorectoplasty was performed at the age of 7 months, followed by colostomy closure at the age of 12 months. She was reviewed in clinic at the age of 18 months. Her development and growth parameters were normal. Her hearing was normal and brainstem auditory evoked potential (BSAEP) were normal. On examination, she showed midface hypoplasia with a flat nasal root and poorly developed nasal bridge with anteverted nares and bilateral dysplastic ears with hypoplastic helices and antehelices (Figure 1a, b). Her limbs were normal, only showing bilateral 5th finger clinodactyly. At the age of 5 years and 11 months her height was 117 cm (55th centile), weight 21.4 kg (47th centile) and head circumference 50.5 cm (35th centile). Development, hearing, and dentition were normal. She had achieved fecal continence.

Patient 2 is the older brother of Patient 1. He was born at term (39 + 6 weeks) following an uneventful pregnancy by cesarean section because of suspected fetal distress. Apgar scores were 8 and 9 at 1 and 5 min, respectively. His birth weight was 3540 g (65th centile), length 52 cm (84th centile), and head circumference 36.5 cm (85th centile). Neonatal examination showed bilateral microtia with a patent external auditory canal. Abdominal and cerebral US were normal. Echocardiography was normal. He failed to pass the neonatal screening hearing test, but a subsequent ENT assessment and BSAEP were normal. He was reviewed in clinic with his sister at the age of 6 years. His development and growth parameters were normal. His hearing was normal. BSAEP, audiometry and computed tomography of temporal bone were all normal. On examination, he showed midface hypoplasia with a flat nasal root and poorly developed nasal bridge with anteverted nares and bilateral dysplastic ears with hypoplastic helices and antehelices (Figure 1c, d). His limbs were normal, with bilateral fifth finger and toe clinodactyly. At the age of 10 years and 5 months, his height was 148 cm (78th centile), weight 38.5 kg (50th centile), and head circumference 55.5 cm (84th centile). Development, hearing, and dentition were normal.
2.2 Family 2
Two sisters born to consanguineous parents were reported with a possible new syndrome named EVE dysplasia (Amiel et al., 1999). No further clinical information has been available since that publication.
3 RESULTS
An exome sequencing (ES) study identified compound heterozygous variants in HSPA9 in patient 1 at the age of 4 (NM_004134.7) c.371T>C (p.Ile124Thr) and c.376C>T (p.Arg126Trp), both located in trans at exon 4 of the gene. Sanger sequencing confirmed the presence of both variants in trans in the affected brother. The p.Ile124Thr variant was inherited from the father and the p.Arg126Trp variant from the mother. Both variants are located on the surface of the Nucleotide Binding Domain (NBD) of the protein. The p.Arg126Trp variant was described in the two sibs reported by Royer-Bertrand et al. (2015) and has been shown to disrupt ATP hydrolysis, interdomain linker binding and thermostability, and increase propensity for aggregation (Moseng et al., 2019). The p.Ile124Thr variant, on the other hand, is a previously unreported variant classified as a VUS according to ACMG recommendations (Richards et al., 2015), with an allele count of 2 out of 282,882 alleles in the GnomAD database. This variant affects a highly evolutionary conserved nucleotide and amino acid across HSPA9 orthologs and HSP70 family members. In silico 3D modeling of the human HSPA9 structure revealed that residues Ile124 and Arg126 were both located next to each other on the surface of the protein, lying on a single loop close to the predicted interface between NBD and the Substrate Binding Domain (SBD). Change of the wildtype Ile124 residue to threonine disrupts the canonical hydrogen bonding, and may disturb HSPA9 activity and stability (Figure S1).
A radiological skeletal survey, following the identification of bilallelic HSPA9 alterations in both sibs, was requested for each. Patient 2 showed hypoplastic nasal bones and mild flattened vertebral bodies, with irregular endplates, especially in the dorsal area, and mild dorsal kyphosis. No coronal clefts were identified. Femoral heads were flattened. Distal femoral epiphyses were dysplastic, with hypoplastic lateral condyle and deep intercondylar notches resembling bifid femora. Other epiphyses were also mildly flattened and irregular. There were striations in the metaphysis of the distal femora in both patients. Carpal bones were mildly small and irregular. Bone age was mildly delayed (Figure 1g–i). His sister showed similar but milder findings, possibly due to her younger age (Figure 1e, f).
Concerning Family 2, ES identified another previously unreported variant (NM_004134.6; c.1085 C>T, p.Thr362Ile), homozygous in the affected sisters while both parents were heterozygous. The equivalent of Thr362 in HSPA9 is highly conserved in HSP70 family members. Analysis of the 3D structure of HSPA9 indicates that Thr362 falls in an alpha-helix of the NBD, and the change to isoleucine is predicted to disrupt hydrogen bonding that normally exists between the wildtype threonine and the backbone of the alpha-helix, potentially destabilizing the protein (Supplemental Figure S1).
4 DISCUSSION
Here, we show that EVE and EVEN-PLUS syndromes are allelic conditions and describe two sibs with EVEN-PLUS syndrome, showing the distinctive radiological findings but milder facial features. The clinical features reviewed in nine subjects with EVE/EVEN-PLUS syndrome give evidence for a variable clinical spectrum (Table 1). We further provide in silico data supporting the impact of the newly described variants on HSPA9 function (Figure S1).
| Proband | This study | Amiel et al. (1999) | Royer-Bertrand et al. (2015) | Nagrani et al. (2018) | Younger et al. (2020) | Total | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient 1 | Patient 2 | Patient 1 | Patient 2 | Patient 1 | Patient 2 | Patient 3 | Patient 1 | Patient 1 | |||
| Sex | F | M | F | F | F | F | F | F | M | 7F/2M | |
| Birth measurements | Length 52 cm, weight 4.2 kg OFC 36.5 cm (week 41) | Length 50 cm, weight 3.5 kg, OFC 37 cm (week 39 + 6) | Length 46.5 cm, weight 2.6 kg, OFC 33.5 cm | Length 43 cm, weight 2.5 kg, OFC 32 cm | Length 38 cm, weight 2.2 kg (week 39) | Length 39 cm, weight 2.8 kg (week 38) | Length 39 cm, weight 2.7 kg (week 38) | Length 49 cm, weight 3.3 kg (week 38) | Length 43 cm, weight 2.7 kg (week 38) | ||
| Origin | Spanish | Spanish | Algerian | Algerian | Korean | Chilean | Chilean | Indonesian | Cherokee Caucasian | ||
| Body system | Features | ||||||||||
| Head/face | Brachycephaly | − | − | Unk | Unk | − | − | + | − | + | 2 |
| Eyes | Synophris and/or arched eyebrows | + | + | ? | ? | + | + | + | + | + | 7 |
| Ears | Hypoplastic/dysplastic external ears | + | + | + | + | + | + | + | + | + | 9 |
| Nose | Nasal bone hypoplasia | + | + | + | + | + | + | + | + | + | 9 |
| Anomaly of the nares (triangular) | − | − | + | + | + | + | + | + | + | 7 | |
| Mouth | Hypodontia | − | − | − | − | − | − | + | − | − | 1 |
| Chest | Short thorax and sternum | − | − | − | − | − | − | − | − | + | 1 |
| Widely spaced nipples | − | − | − | − | − | − | − | − | + | 1 | |
| Cardiovascular | Congenital heart defect | − | − | − | − | + | + | + | − | + | 4 |
| Abdomen | Hypoplastic Kidney | − | − | − | − | − | − | + | + | − | 2 |
| Hydronephrosis/vesico-ureteral reflux | − | − | − | − | − | − | + | − | + | 2 | |
| Genitalia/anus | Anorectal anomaly | + | − | − | − | + | − | + | − | + | 4 |
| Unilateral chryptorchidism | N/A | − | N/A | N/A | N/A | N/A | N/A | N/A | + | 1 | |
| Extremities | Single palmar crease | − | − | + | − | − | − | − | − | + | 1 |
| Bilateral clubfoot | − | − | − | − | − | − | − | − | + | 1 | |
| Skin/hair | Aplasia cutis | − | − | − | + | − | + | + | − | − | 3 |
| Two hair whorls | − | − | Unk | Unk | − | + | − | + | − | 2 | |
| Sparse hair | − | − | Unk | Unk | + | − | − | − | − | 1 | |
| Skeletal | Dysplastic femoral head | + | + | + | + | + | + | + | + | + | 9 |
| Bifid femur | + | + | + | + | + | + | + | + | + | 9 | |
| Dysplastic epiphyses at the knee | + | + | + | + | + | + | + | + | − | 8 | |
| Dysplastic acetabula | − | − | + | + | + | + | + | − | + | 6 | |
| Vertebral clefting | − | − | + | + | + | − | + | + | + | 6 | |
| Delayed ossification | + | + | + | + | − | + | + | − | + | 7 | |
| Short stature | − | − | − | − | + | + | + | − | + | 4 | |
| Scoliosis and/or Kyphosis | − | + | − | − | − | − | − | + | + | 3 | |
| Hip dislocation | − | − | − | − | − | + | + | − | + | 3 | |
| Dislocated patellae | − | − | − | − | − | + | + | + | − | 3 | |
| 13 pairs of ribs | − | − | − | − | − | − | − | − | + | 1 | |
| Hemivertebra | − | − | − | − | − | − | − | − | + | 1 | |
| Agenesis of the coccyx | − | − | − | − | − | − | + | − | − | 1 | |
| Abnormal and torn meniscus | − | − | − | − | − | − | − | + | − | 1 | |
| Abnormal gait | − | − | − | − | − | − | − | + | − | 1 | |
| Neurologic | Agenesis of the corpus callosum | − | − | − | − | − | − | + | − | + | 2 |
| Developmental delay | − | − | − | − | − | − | + | − | + | 2 | |
| Agenesis of the septum pellucidum | − | − | − | − | − | − | − | − | + | 1 | |
| Hypotonia | − | − | − | − | − | − | − | − | + | 1 | |
| Genetic | Biallelic HSPA9 variants | p.Arg126Trp | p.Arg126Trp | p.Thr362Ile | p.Thr362Ile | p. Val296Ter | p.Arg126Trp | p.Arg126Trp | p.Lys563Ter | p. Leu273Ter | |
| p.Ile124Thr | p.Ile124Thr | p.Thr362Ile | p.Thr362Ile | p.Tyr128Cys | p.Arg126Trp | p.Arg126Trp | p.Asn149Ile | p.Leu319Phe | |||
- Abbreviations: N/a, not applicable; Unk, unknown.
Individuals reported with EVEN-PLUS syndrome show a very distinct craniofacial phenotype with an extremely underdeveloped nose and distinctive narrow and triangular nares (Nagrani et al., 2018; Royer-Bertrand et al., 2015; Younger et al., 2020). The sisters reported by Amiel et al. (1999) presented with milder facial features, but still showed an underdeveloped nose with triangular nares. In contrast, the two previously undescribed sibs in this article have facial features that are common in EVEN-PLUS syndrome, such as a flat facial profile, midface hypoplasia, dysplastic/hypoplastic ears, and nasal bone hypoplasia, but normal nose and nares. These sibs provide evidence that there is clinical variability of facial features associated with biallelic variants in HSPA9, including subtle facial features and bilateral microtia. Due to the scarce number of patients described in the scientific literature, future description of new cases will be necessary in order to identify the underlying cause for this phenotypic variability. As previously outlined, skeletal findings are characteristic and consistent in virtually all subjects and consist mainly of dysplastic femoral heads, bifid distal femurs, and dysplastic epiphyses at the knee. Other frequently observed skeletal findings include dysplastic acetabula, vertebral clefting, delayed ossification, and short stature. Congenital heart defects, such as atrial and ventricular septal defects, persistent foramen ovale, and septal aneurysm, were described in four of the nine patients with a formal cardiac evaluation. Renal alterations were observed in three of the nine patients with renal ultrasound. One subject presented vesicoureteral reflux, two had hypoplastic kidneys with normal kidney function and one had hydronephrosis which subsequently resolved. Aplasia cutis and anorectal anomalies are infrequent features but are also part of the phenotypic spectrum associated with HSPA9; their occurrence is probably influenced by the genetic background, and they show incomplete penetrance. Development was normal in most of the subjects reviewed.
Given the association with other malformations, we suggest that specific examinations should be performed to rule out cardiovascular, urogenital, and gastrointestinal defects in addition to radiological skeletal surveys in patients with pathogenic biallelic variants in HSPA9. All these findings help us to refine the phenotypic spectrum associated with EVEN-PLUS syndrome, allowing distinguishing it from other mitochondrial skeletal disorders and clinically overlapping conditions with different molecular etiology (Table S1).
The new sibs described in this article present the previously unreported variant p.Ile124Thr in trans with the p.Arg126Trp variant, while another novel homozygous variant, p.Thr362Ile, was identified in the original EVE dysplasia sisters. Both previously unreported variants (p.Ile124Thr and p.Thr362Ile) are expected to present a deleterious effect, as predicted by in silico analysis and 3D modeling. Therefore, we assume that these two substitutions probably disturb normal HSPA9 activity and stability.
This report shows the phenotypic variability of EVEN-PLUS syndrome. We suggest that this diagnosis should be considered in patients with bilateral microtia with or without associated findings such as anorectal anomalies and aplasia cutis. Radiological investigations would help to confirm or exclude this diagnostic possibility. We suggest that further examinations should be conducted for early detection of additional anomalies.
AUTHOR CONTRIBUTIONS
Fernando Santos-Simarro, Sixto García-Miñaúr, Jeanne Amiel, and Manuel Parrón Pajares made the clinical follow-up of the family in the clinic, neurological evaluations and phenotypic description of the siblings. Manuel Parrón Pajares, Sixto García-Miñaúr, and Christopher Gordon contributed to the writing of the manuscript and made important comments for its improvement. Carmen Jiménez Rodríguez coordinates the NGS unit, supported by the technicians Victoria Eugenia Fernandez and Inmaculada Rueda. Rocío Mena coordinates the Sanger sequencing unit, supported by the technician María Fernandez. Ángela del Pozo and Mario Solís carried out the bioinformatics analysis and quality reports of the samples and Marta Pacio Miguez performed the filtering and interpretation of the variants. Marta Pacio Miguez worked on the manuscript. María Palomares-Bralo has coordinated and reviewed the NGS studies carried out in this family as well as the writing of the manuscript. All authors discussed the results and commented on the manuscript.
ACKNOWLEDGMENTS
We want to express our deep and sincere gratitude to the family members and staff from all the units that participated in the study.
FUNDING INFORMATION
Marta Pacio Miguez is supported by a grant of the Raregenomics network, financed by the Dirección de General de Universidades e Investigación de la Comunidad de Madrid (S2017/ BMD-3721). This study was supported by fundings from the AES, ISCIII (PI19/01681):Whole exome sequencing protocol in pediatric pacients admitted to critical or highly complex units; “Proyecto Piloto para la mejora del diagnóstico genético en personas y familias afectadas o con sospecha de padecer enfermedades raras de base genética” of the Ministry of Health, under the grant BOCM-20181126-24 provided by the Consejería de Sanidad de la Comunidad de Madrid.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are openly available athttps://doi.org/10.1136/jmg.36.7.561;https://doi.org/10.4172/1747-0862.1000350;https://doi.org/10.1021/acs.jpcb.9b00071;https://doi.org/10.1038/srep17154;https://doi.org/10.1002/ajmg.a.61808;https://www.rcsb.org/structure/6NHK.