Craniocervical junction issues after infancy in achondroplasia
Abstract
More information is available concerning risks of craniocervical junction issues in infancy than at later ages. Therefore, we elected to quantify the risks at greater than 1 year of age through a retrospective analysis of 477 individuals with achondroplasia using a REDCap database. Evaluation of these 477 individuals revealed 77 (16.1%) who had pathologic neurologic manifestations after 1 year of age related to the craniocervical junction. Within this subpopulation of 77 individuals, 43 (55.8%) underwent craniocervical decompression surgery, or 9.0% of the total population. Whether decompressed or not, most individuals with craniocervical junction issues after infancy had a normal outcome, without long-term neurological sequelae (57/77, 74.0%). The remaining 20 had various long-term neurological issues. This is the first cohort based estimate of risks related to the upper cervical spine in individuals with achondroplasia specifically beyond infancy.
1 INTRODUCTION
It is widely recognized that infants with achondroplasia are at an increased risk to develop life and health threatening complications related to constriction at the craniocervical junction (Aryanpur, Hurko, Francomano, Wang, & Carson, 1990; Pauli et al., 1984; Pauli, Horton, Glinski, & Reiser, 1995; Yang, Corbett, Brough, Heidelberger, & Bernstein, 1979). Due to an abnormally small and/or “key-hole” shaped foramen magnum, compression of the upper cervical spine and brainstem may arise, resulting in both direct damage to the upper cervical spinal cord and hypoxic damage to central respiratory control centers (Hecht, Francomano, Horton, & Annegers, 1987; Pauli, 2019; Pauli et al., 1995). This damage can manifest clinically as central sleep apnea, features of high cervical myelopathy, and infant death (Pauli et al., 1995). In those in whom clinical, polysomnographic, and imaging (Sanders, Sheldon, & Charrow, 2019) concerns arise in infancy, suboccipital decompressive surgery can prevent life threatening events (Pauli et al., 1995) and result in a positive long-term outcome (Ho et al., 2004).
The reported overall prevalence of children with achondroplasia of all ages undergoing suboccipital decompression is highly variable, ranging from 3 to 45% (Bagley, Pindrik, Bookland, Camara-Quintana, & Carson, 2006; Danielpour, Wilcox, Alanay, Pressman, & Rimoin, 2007; Francomano et al., 1993; Hunter, Bankier, Rogers, Sillence, & Scott, 1998; Pauli, 2019; Reid et al., 1987). Although risks of craniocervical complications, and particularly risks for sudden unexpected death, are greatest in infancy, the foramen magnum remains small throughout an individual's lifetime (Hecht, Horton, Reid, Pyeritz, & Chakraborty, 1989), leaving a residual risk for acute or chronic cervical myelopathy. However, there is only limited literature on the manifestations of craniocervical junction constriction and the need for decompression after infancy (e.g., Aryanpur et al., 1990; Boor, Fricke, Brühl, & Spranger, 1999; King, Vachhrajani, Drake, & Rutka, 2009; Morgan & Young, 1980; Ryken & Menezes, 1994). Therefore, we retrospectively assessed a cohort of 477 individuals with achondroplasia to characterize the frequency, presentations, interventions, and outcomes of individuals with craniocervical junction issues after 1 year of age.
2 METHODS
This study was reviewed and approved by the Institutional Review Board of the University of Wisconsin-Madison School of Medicine and Public Health, Madison, WI.
All individuals with confirmed diagnoses of achondroplasia via molecular, radiographic, and/or clinical findings seen at the Midwest Regional Bone Dysplasia between 1980 and 2017 were included in this study. These individuals were followed by an experienced physician, capable of differentiating achondroplasia from other bone dysplasias. Patients were excluded only if confirmed diagnoses of homozygous achondroplasia, compound heterozygosity (i.e., achondroplasia + hypochondroplasia) or double heterozygosity were present (Flynn & Pauli, 2003; Pauli et al., 1983).
All data including the presence and type of craniocervical concerns, surgical history, imaging history, and patient outcomes were extracted from medical records and entered into a supplemental REDCap database (Harris et al., 2009) and engrafted onto a multicenter achondroplasia natural history study (CLARITY) (Hoover-Fong et al., 2020).
In retrospective chart review, the following clinical descriptors were considered to be sentinels of possible craniocervical junction concerns, if they were present beyond 1 year of age, and were flagged: ongoing follow up of previous concerns of cervicomedullary stenosis; severe hypotonia persisting past infancy; persisting motor delays; neurologic examination of concern; acute life-threatening event; and development of hydrocephalus. Additionally, the following abnormalities of the upper cervical spine detected by magnetic resonance imaging (MRI) were also considered to be similarly concerning: worsening compression; development of a T2 signal abnormality; development of a syrinx. Although clinical features were used as sentinel indicators, individuals whose only abnormality included a neurologic sign of concern were excluded from this study, since non-progressive and isolated abnormalities of neurologic examination (Apparently Benign Craniocervical Signs) are a common and apparently often benign finding in achondroplasia (Smid, Legare, Modaff, & Pauli, 2020).
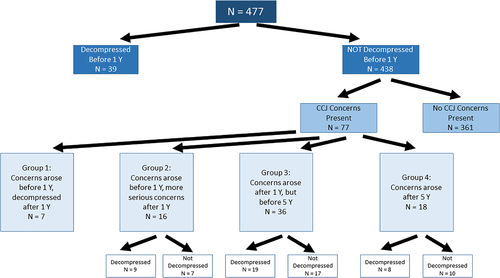
The purposes of this study were to quantify the prevalence of craniocervical junction concerns after age 1 year, to document how frequently suboccipital and upper cervical decompressive surgery is needed beyond infancy and to investigate the indications, interventions, and outcomes of those who had craniocervical junction concerns beyond 1 year of age. Thus, all of those who never demonstrated craniocervical junction concerns, as well as the 39 individuals who underwent decompression surgery prior to 1 year of age were excluded (Figure 1). Note that we chose not to use polysomnographic features to identify those with late craniocervical junction concerns since central apnea and/or sloppiness of central respiratory control appear to be far more often important indicators of craniocervical concerns in the first year of life (Pauli et al., 1995).
3 RESULTS
3.1 Demographics
Overall, 116 of 477 (24.3%) patients had some craniocervical junction concerns at some point in their life. Of these 116 individuals, 39 (33.6% of those with concern, 8.2% of total population) were decompressed before 1 year of age and removed from further analysis here. The remaining 77 individuals (66.4% of those with concern, 16.1% of total population) were not decompressed before 1 year of age, yet had abnormal manifestations of the craniocervical junction beyond 1 year of age (Figure 1).
There was no predilection by sex. Of these 77 individuals, 38 (49.4%) were female and 39 (50.7%) male.
Initial presentation was at a median age of 1.3 years (males: 1.2 years, females: 2.0 years), and mean age of was 4.9 years +/− 9.5 years (males only: 2.7 years +/−3.4 years, females only: 7.2 years +/− 12.8 years). There were several adult female outliers, with initial presentation of craniocervical junction concerns at 70, 29, 28, and 18 years of age.
3.2 Classification of groups
Individuals were grouped based on their age of initial presentation and need for decompression (Figure 1). As shown in Figure 1, Group 1 includes seven individuals whose initial concerns arose prior to 1 year of age but in whom decompressive surgery did not occur until after 1 year of age. A total of 16 individuals are included in Group 2, where concern initially arose prior to 1 year of age, but which concerns became more serious after 1 year of age. Within Group 2, nine patients were decompressed. Group 3 is composed of 36 individuals in whom the initial concerns related to the craniocervical junction arose between one and 5 years of age. Of those in Group 3, 19 were decompressed. Lastly, 18 individuals were placed in Group 4—their initial concerns did not arise until after 5 years of age. Of the 18 individuals in Group 4, eight were decompressed.
3.3 Suboccipital decompression
Within our entire cohort of 477 individuals, our analysis includes 82 individuals (17.1%) who required suboccipital decompression surgery.1 More than half of all such surgeries were completed after age 1 year (n = 43; 9.0% of entire population, 52.4% of subpopulation) (Figure 1). The most common listed indications for suboccipital decompression after 1 year of age were neuroimaging findings (demonstrated in 41/43, 95.3%) (e.g., foramen magnum stenosis, n = 24; presence of T2 signal abnormality, n = 14; cord indentation, n = 12; obliteration of subarachnoid fluid layer, n = 10; and syrinx, n = 6). Subjects may have presented with multiple types of MRI findings and therefore the number of events exceeds the number of subjects. Other common listed indications for suboccipital decompression included failure of progress in gross motor development (n = 20, 46.6%), and persistent and severe hypotonia (n = 18, 41.9%) (Table 1). Note that of the 43 individuals who had late decompression, 35 had both clinical and imaging indications listed, while in only seven was decompression apparently carried out solely on the basis of imaging features (syrinx development, new T2 signal abnormality). Of the 43 individuals who were decompressed after 1 year of age, four (9.3%) had additional or recurrent symptoms requiring a second decompression surgery.
| Group | Persisting hypotonia | Persisting motor delay | Concerning neurologic examination | Acute life threatening event | Ongoing follow-up of stenosis | Hydrocephalus | Change in MRI: compression | Change in MRI: T2 signal abnormality | Change in MRI: syrinx |
|---|---|---|---|---|---|---|---|---|---|
| Overall, n = 77 | 39 (51%) | 32 (42%) | 38 (49%) | 7 (9%) | 30 (39%) | 4 (5%) | 18 (23%) | 18 (23%) | 10 (13%) |
| Group 1, n = 7 | 6 (86%) | 4 (57%) | 3 (43%) | 3 (43%) | 5 (71%) | 0 | 2 (29%) | 1 (14%) | 0 |
| Group 2, n = 16 | 14 (88%) | 11 (69%) | 8 (50%) | 3 (19%) | 8 (50%) | 0 | 4 (25%) | 2 (13%) | 2 (13%) |
| Group 2, decompressed, n = 9 | 7 | 7 | 6 | 0 | 4 | 0 | 4 | 2 | 2 |
| Group 2 NOT decompressed, n = 7 | 7 | 4 | 2 | 3 | 4 | 0 | 0 | 0 | 0 |
| Group 3, n = 36 | 17 (47%) | 15 (42%) | 18 (50%) | 0 | 11 (31%) | 3 (8%) | 10 (28%) | 8 (22%) | 3 (8%) |
| Group 3, decompressed, n = 19 | 8 | 10 | 11 | 0 | 8 | 2 | 7 | 7 | 3 |
| Group 3 NOT decompressed, n = 17 | 9 | 5 | 7 | 0 | 3 | 1 | 3 | 1 | 0 |
| Group 4, n = 18 | 2 (11%) | 2 (11%) | 9 (50%) | 1 (6%) | 6 (33%) | 1 (6%) | 2 (11%) | 7 (39%) | 5 (28%) |
| Group 4, decompressed, n = 8 | 1 | 1 | 6 | 0 | 4 | 1 | 1 | 4 | 3 |
| Group 4 NOT decompressed, n = 10 | 1 | 1 | 3 | 1 | 2 | 0 | 1 | 3 | 2 |
Of the patients decompressed after 1 year of age, the average duration of time between initial recognition of concern and completion of decompression surgery was 0.65 years ± 0.87 years (median = 0.53 years). Thirty-five of 43 (81.4%) were completed within 1 year of initial identification of craniocervical junction concerns. Group 1 included seven individuals whose initial concerns arose prior to 1 year of age, but who were not decompressed until after 1 year of age. Of these seven individuals, four (57%) had undergone decompression surgery by 13 months, and six (86%) were decompressed by 18 months of age. The average duration between age of initial recognition and completion of decompression surgery within Group 1 was 0.80 years ± 0.42 years.
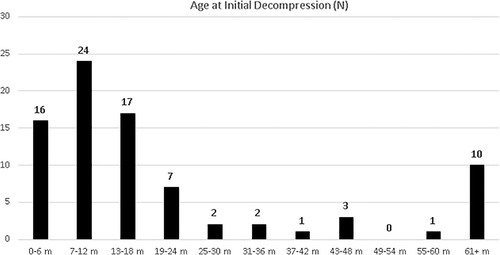
The distribution of ages at which decompressive surgery occurred is shown in Figure 2.
3.4 Outcomes
The outcomes of all subjects with craniocervical junction concerns after infancy are summarized in Table 2. Overall, 57/77 (74.0%) had an apparently normal outcome, without evidence for any neurological sequelae. Of the 20 patients (26.0%) with an abnormal outcome, the most common abnormalities included persisting hypotonia (n = 11, 14%), persisting motor delays (n = 11, 14%), asymmetric strength (n = 7, 9%), and limited walking (n = 6, 8%). (See also Supporting Information, Tables 1 and 2).
| Group | Normal function | Persisting hypotonia | Persisting motor delay | Asymmetric strength | Hemiparesis | Limited walking | No walking | Bladder incontinence, partial | Bladder incontinence, full | Bowel incontinence, partial | Bowel incontinence, full |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall, n = 77 | 57 (74%) | 11 (14%) | 11 (14%) | 7 (9%) | 5 (6%) | 6 (8%) | 2 (3%) | 4 (5%) | 1 (1%) | 3 (4%) | 1 (1%) |
| Group 1, n = 7 | 5 (71%) | 2 (29%) | 1 (14%) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Group 2, n = 16 | 9 (56%) | 5 (31%) | 5 (31%) | 3 (19%) | 1 (6%) | 2 (13%) | 1 (6%) | 2 (13%) | 0 | 1 (6%) | 1 (6%) |
| Group 2, decompressed, n = 9 | 5 | 4 | 3 | 2 | 0 | 1 | 1 | 1 | 0 | 0 | 0 |
| Group 2 NOT decompressed, n = 7 | 4 | 1 | 2 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 |
| Group 3, n = 36 | 28 (78%) | 3 (8%) | 4 (11%) | 2 (6%) | 2 (6%) | 2 (6%) | 0 | 1 (3%) | 0 | 1 (3%) | 0 |
| Group 3, decompressed, n = 19 | 14 | 2 | 3 | 2 | 2 | 2 | 0 | 0 | 0 | 0 | 0 |
| Group 3 NOT decompressed, n = 17 | 14 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 |
| Group 4, n = 18 | 15 (83%) | 1 (6%) | 1 (6%) | 2 (11%) | 2 (11%) | 2 (11%) | 1 (6%) | 1 (6%) | 1 (6%) | 1 (6%) | 0 |
| Group 4, decompressed, n = 8 | 6 | 1 | 1 | 2 | 1 | 1 | 0 | 1 | 1 | 1 | 0 |
| Group 4 NOT decompressed, n = 10 | 9 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 |
Group 2 included 16 individuals whose initial concern arose prior to 1 year of age, but more serious concerns arose at a later time. Of these 16, only nine (56%) were subsequently neurologically normal. Persisting problems were evident both in those decompressed (4/9, 44%) and in those judged not to require decompression (3/7, 43%).
Individuals within Groups 1 and 2 were the least likely to have a completely normal outcome (71 and 56%, respectively). That is, those with earlier onset of concerns were more likely to have persisting sequelae despite intervention.
Groups 3 and 4 represent 54 individuals who had no evidence for craniocervical junction concerns during infancy but who developed such concerns for the first time later in life. Subjects in Groups 3 and 4 appear to be more likely to be neurologically intact in the long term.
Of 43 individuals who underwent “late” decompression, 30 (69.8%) had a completely normal neurologic outcome. The most common residual abnormalities within the 13 decompressed individuals without a normal outcome included persistent hypotonia (n = 9), persistent motor delays (n = 9), asymmetric strength (n = 6), and limited walking (n = 4).
What follows are two examples of late presentations of craniocervical junction concerns in achondroplasia.
3.5 Case studies
3.5.1 Case 1 (Group 3; delayed intervention and poor outcome)
This girl was thought to have completely normal neurologic status and diagnosis-appropriate development until ~2 years of age. At this time, the patient began to show decreased amounts of crawling and pulling to stand. Approximately 3 months later, the child's parents began to notice the child's left foot would drag when she cruised. Within the next 2 months, the patient was no longer able to hold a cup, was using her left side much less than her right, and was no longer cruising. She was seen for the first time through the Midwest Regional Bone Dysplasia Clinic at 2.5 years of age at which time left sided weakness and signs of cervical myelopathy were unequivocal. Computerized tomography (CT) was performed (prior to availability of MRI) and showed an extremely narrow foramen magnum. She underwent decompression within a week of this evaluation. Intraoperatively, the spinal cord at the craniocervical junction was markedly compressed. She showed considerable postoperative improvement, but has permanent neurologic sequelae related to left-sided weakness, which results in marked limitation of independent ambulation and poor left hand fine motor function.
3.5.2 Case 2 (Group 3, accidental trauma)
This patient had reassuring assessments in infancy and no neurologic concerns prior to 3.5 years of age, when she was bumped by the family dog, fell and hit her head. She had questionable loss of consciousness, and was unable to move the left side of her body. MRI of the cervical spine demonstrated stenosis of the foramen magnum with cord compression, edema, and T2 signal abnormality (as well as progressive ventriculomegaly when compared to a previous MRI from infancy). She underwent decompression surgery 2 days after the trauma incident. She improved neurologically, but has residual mild hemiparesis of both the arm and the leg.
4 DISCUSSION
We document here that craniocervical junction issues remain common in achondroplasia after infancy. Although lethal outcomes appear to be mostly limited to issue arising in the first year of life, development of high cervical myelopathy is a concern throughout childhood (and even in a few adults). In those in whom no craniocervical intervention is deemed warranted in the first year of life, almost 1/5 (77/438, 17.6%) are found to have serious concerns later in life and 9.0% (43/477) overall will require suboccipital decompression surgery after 1 year of age. Thus, one-half of such surgeries (43/82, 52.4%) in persons with achondroplasia occur after a year of age (Figure 2).
Of the 77 individuals with craniocervical junction concerns after infancy, most (54/77, 70.1%) had no evidence, by clinical examination or imaging, of significant cervical cord issues prior to 1 year of age. This is not, then, simply an issue of delayed intervention. Rather, most of these patients were asymptomatic during infancy, but developed craniocervical junction issues at a later age.
Few previous studies have attempted to estimate the prevalence of the need for cervicomedullary decompression of individuals with achondroplasia after 1 year of age. Table 3 summarizes those previous investigations. The exceedingly broad range—from 2.7 to 22.4%—is most likely primarily attributable to different criteria used in deciding if decompression surgery was warranted.
4.1 Craniocervical junction issues in achondroplasia
The most worrisome issue related to the craniocervical junction is the risk for sudden unexpected death early in life (Pauli et al., 1984; Pauli et al., 1995; Reid et al., 1987). However, in addition, individuals with achondroplasia have risk to develop high cervical myelopathy (Yang et al., 1979), which can develop at any age (Mukherjee, Pressman, Krakow, Rimoin, & Danielpour, 2014). Both arise because of compression of the upper cervical spine, adjacent vasculature, and/or brainstem secondary to anatomic differences of the foramen magnum and suboccipital region in achondroplasia (Hecht et al., 1987; Yang et al., 1979). Clinical signs of high cervical myelopathy in children may include persisting hypotonia, asymmetric strength, or reflexes in the arms or legs, ankle clonus, and up going response to Babinski stimulation. Evidence for myelopathy after infancy may include features such as decreased endurance, sudden or transient pain in the arms or legs, decreased fine motor function, or changes in bowel or bladder continence. Additionally, individuals may present with acute myelopathy due to trauma (Pauli, 2019). Individuals presenting with unequivocal chronic or acute evidence for high cervical myelopathy need to undergo cervicomedullary decompression surgery.
4.2 Outcomes of individuals with craniocervical junction concerns after 1 year of age
The majority of individuals (55/77, 71.4%) with craniocervical junction concerns after infancy will have a normal outcome. In fact, of the 54 individuals whose initial concerns did not arise until after 1 year of age (Groups 3 and 4), 43 (79.6%) had what was judged to be a completely normal neurologic outcome, whether decompression surgery was necessary or not. Therefore, while craniocervical issues frequently arise after 1 year of age, with appropriate intervention, a good outcome should be anticipated. These findings are similar to those of Bagley et al., (2006), who described no future recurrent signs/symptoms of cervical myelopathy in 38 of 43 (88.4%) individuals with achondroplasia who underwent decompression surgery.
There were 16 individuals in whom early but worsening symptoms suggest that decompression earlier in life was warranted but was delayed (Group 2). Only nine (56%) of these individuals were subsequently neurologically normal. Such delays are associated with a negative outcome and are particularly concerning.
4.3 Etiologies of craniocervical junction concerns after infancy
Craniocervical junction issues after infancy may arise acutely or chronically. As noted, some may be attributed to delayed management (e.g., Case 1). Others are caused by acute trauma, as described in Case 2. Others may, perhaps, arise from unrecognized, recurrent minor injury at the craniocervical junction. Slower growth of the foramen magnum may also be relevant (Matsushita et al., 2009).
4.4 Limitations
The data described here were retrospective and were all derived from chart review and entry into a REDCap database. No additional clinical evaluations specific to this study were carried out. While there is complete ascertainment of the clinic population, of course biases may be present based on individuals having been assessed through a specialty clinic such as the Midwest Regional Bone Dysplasia Clinic.
Certain of our exclusion criteria may have eliminated a few individuals inappropriately. As noted, patients whose only concern was an isolated abnormal neurologic sign were excluded because such “neurologic leftovers” appear to be common and usually benign findings in achondroplasia (Smid et al., 2020). Polysomnographic results were not considered at all, because our experience suggests that abnormalities of central respiratory control secondary to craniocervical compression probably are confined to the first year of life.
4.5 Recommendations
All individuals with achondroplasia should undergo a neurologic assessment including: neurologic history and neurologic examination, imaging of the craniocervical junction (by computerized tomography or MRI), and polysomnography in early infancy (Mukherjee et al., 2014; Pauli, 2019; Pauli & Legare, 1998; Sanders et al., 2019). After infancy, individuals should be routinely monitored to ensure that no new craniocervical junction concerns arise. If an individual develops new clinical signs and symptoms suggestive of high cervical myelopathy, magnetic resonance imaging should be pursued. Additionally, if an individual experiences trauma to the head or neck, emergent assessment to ensure no acute damage at the craniocervical junction has occurred is essential.
ACKNOWLEDGMENTS
We would like to express special thanks to Adekemi Alade and Chengxin Liu for their guidance in REDCap navigation and data requests. Qianqian Zhao generously provided statistical advice. BioMarin Pharmaceutical provided funding for the larger REDCap database upon which this study was grafted. We thank the PI and the other co-PIs of the larger collaborative investigation, Julie Hoover-Fong, Johns Hopkins University; Jacqueline Hecht, University of Texas—Houston McGovern Medical School; and Michael Bober, Nemours/Alfred I. duPont Hospital for Children.
CONFLICT OF INTEREST
All authors declare that they have no conflicts of interest.
Endnote
Open Research
DATA AVAILABILITY STATEMENT
Primary data supporting this investigation is not available because of HIPAA limitations.