49,XXXXY syndrome: A study of neurological function in this uncommon X and Y chromosomal disorder
Abstract
49,XXXXY is a rare chromosomal variation characterized by deficits in motor, language, and cognitive domains. This study reports on the neurological function and dysmorphic features in the largest cohort to date. Seventy-two boys with 49,XXXXY were evaluated on a variety of domains including a neurological examination and neuromotor assessments including the Beery Buktenica Developmental Test of Visual-Motor Integration, Sixth Edition, the Bayley Scales of Infant and Toddler Development, Third Edition (BSID-III), and the Bruininks–Oseretsky Test of Motor Proficiency, Second Edition. Results supported previous literature by describing high occurrences of truncal and extremity hypotonia, which significantly impacts on motor milestones and ambulation in this population. The boys presented with dysmorphic features including epicanthal folds, frontal bossing, and synophrys. Visual perception skills were mildly impaired and cranial nerves were typically intact, however capabilities in motor coordination and fine motor precision were greatly delayed, supporting deficits in refined and controlled hand movements versus widespread visual deficits. Preschool boys treated with testosterone replacement had significantly increased scores when compared to the untreated group on the BSID-III Psychomotor Development Index, further supporting previous research indicating that testosterone replacement may have a positive impact on neurodevelopmental outcomes in males with additional X chromosomes. Boys with 49,XXXXY may benefit from hormonal treatment in conjunction with early intervention services to address their significant motor deficits.
1 INTRODUCTION
49,XXXXY, which occurs in 1:85,000–100,000 live male births (Kleczkowska, Fryns, & van den Berghe, 1988; Linden, Bender, & Robinson, 1995), is a rare sex chromosome aneuploidy that is characterized by deficits in motor, language, and cognitive domains. 49,XXXXY is typically diagnosed within the first year of life, often due to congenital malformations (Burgemeister, Gronwald, Maurer, & Zirn, 2019; Sprouse et al., 2013). Case studies have noted epicanthic folds, upslanting palpebral fissures, broad nasal bridge and nose, low-set ears, arched eyebrows, synophrys, mild hypoplasia of the corpus callosum on brain neuroimaging studies and hypertelorism. (Argun et al., 2015; Burgemeister et al., 2019; Etemadi, Basir, & Ghahremani, 2015; Özcan & Şahin, 2017; Schluth et al., 2002; Sprouse et al., 2013; Stover, Cowan, Cross, Hoffman, & Craigo, 2017). Less common features include cleft lip and palate and cardiac disorders (Gropman et al., 2010). Many dental anomalies appear throughout the lifetime of these boys, including delayed dentition and eruption, hypodontia, taurodontism, and malocclusion (Burgemeister et al., 2019).
While many studies on 49,XXXXY have cited delayed motor milestones, there is great variability in the severity of the delays, with sitting occurring between 8 to 24 months, standing beginning between 10 to 30 months of age, and ambulation ranging from 16 to 54 months of age (Borghgraef, Fryns, Smeets, Marien, & Berghe, 2008; Burgemeister, 2019; Curfs, Schreppers-Tijdink, Wiegers, Borghgraef, & Fryns, 1990; Galasso, Arpino, Fabbri, & Curatolo, 2003; Gropman et al., 2010; Hoffman, Vossough, Ficicioglu, & Visootsak, 2008; Peet, Weaver, & Vance, 1998; Sijmons et al., 1995). Given the rare incidence of this disorder, few studies have conducted formalized neuromotor testing in boys with 49,XXXXY. Peet et al. reported on one case who, at 12 months of age, demonstrated gross motor skills at the 4-month-old level and fine motor skills at the 9-month-old level. At 36 months, the subject's fine motor skills were at the 15-month-old level (Peet, 1998). More recently, Gropman et al. reported on 13 boys with 49,XXXXY who were evaluated using the Bayley Scales of Infant Development. Composite scores on the Motor Development Index (MDI) ranged from less than 50 to 100, with an average standard score of 79.5. The Beery–Buktenica Developmental Test of Visual Motor Integration was also given to 9 boys with 49,XXXXY, with standard scores ranging from 45 to 88 in visual motor integration, 45 to 82 in motor coordination, and 45 to 104 in visual perception. Additional research in these skills will allow researchers to build a characteristic neuromotor profile of 49,XXXXY, providing information that will create more targeted treatment in this population.
This study describes a detailed profile of the dysmorphology, neurological function, and neuromotor capabilities of a large, international population of boys with 49,XXXXY. It also reports on the potential impact of testosterone treatment on the neuromotor development from preschool-aged boys to adolescents with 49,XXXXY.
2 METHODS
2.1 Study participants
Seventy-two boys with 49,XXXXY were participants in an annual meeting for children with 49,XXXXY and their families (Table 1). All patients had the diagnosis of 49,XXXXY confirmed by karyotype, chromosomal microarray or prenatal diagnosis, however only 17 % had additional testing to determine mosaicism or copy number variations (CNV). Any child with identified mosaicism or CNV has been eliminated from this study. Children were evaluated annually at meetings, which were hosted by The Focus Foundation in collaboration with the Neurodevelopmental Diagnostic Center for Children. Not every child was in attendance each year and not every child completed every assessment due to compliance, availability, and neurocognitive capabilities of the subjects. The boys were seen by a multidisciplinary team including a pediatric physical therapist, a neurodevelopmentalist, an occupational therapist, and a neurologist/geneticist. Informed consents were completed and obtained from each parent of all participants under the IRB-approved study protocol (#20081226).
| Patient characteristics and demographics of the study population (n = 61) | ||||
|---|---|---|---|---|
| N | Mean | Median | Range | |
| Patient characteristics | ||||
| Birth weight (kg) | 56 | 2.47 | 2.47 | 1.50–3.46 |
| Birth length (in) | 38 | 18.39 | 18.5 | 12.99–20.5 |
| Birth head circumference (cm) | 24 | 32.47 | 32.5 | 30–34.5 |
| Patient demographics | ||||
| Maternal age at birth | 53 | 31.04 | 31 | 20–46 |
| Paternal age at birth | 52 | 33.5 | 33 | 21–63 |
| Ethnicity | 45 | Percent of total population | ||
| Caucasian | 35 | 77.78% | ||
| African American | 2 | 4.44% | ||
| Hispanic | 0 | 0% | ||
| Other | 8 | 17.78% | ||
| Delivery method | 38 | |||
| Cesarean | 20 | 52.63% | ||
| Vaginal | 18 | 47.37% | ||
The participants had received varying levels of testosterone treatment by the time of evaluation. Of the 28 boys who completed the motor development domain of the BSID-III, 32.14% were untreated and 67.86% had received early hormonal treatment (EHT). EHT is defined as three 25 mg intramuscular injections of testosterone enanthate within the first year of life. The administration of EHT was based upon the physical examination and recommendation of the pediatric endocrinologist seeing the individual boy with 49,XXXXY.
2.2 Neurological examination
After 16 years of following the children with 49,XXXXY, we have recently begun to collect formalized and detailed assessments of neurological function in order to further investigate the neurodevelopmental progression. Therefore, 16 boys with 49,XXXXY underwent a complete neurological evaluation tailored to their age, which was administered by a pediatric neurologist/clinical geneticist. Cognitive function, muscle tone and strength, cranial nerves, gait, deep tendon reflexes, and sensory systems function were assessed and recorded.
2.3 Neuromotor testing
The BSID-III (Bayley, 2006) assesses developmental functioning of infants and toddlers from birth to 42 months. This paper is reporting specifically on the motor domain of the assessment.
The Beery–Buktenica Developmental Test of Visual-Motor Integration, sixth Edition (BEERY-6) (Beery, Buktenica, & Beery, 2010) ranges from 2 to 100 years of age and helps to assess visual motor capabilities. The assessment tests three domains including visual motor integration (VMI), visual perception (VP), and motor coordination (MC). The average standard score is 100 for each domain.
The Bruininks–Oseretsky Test of Motor Proficiency, Second Edition (BOT-2) (Bruininks & Bruininks, 2005) is an evaluation of gross and fine motor skills for children between the ages of 4 and 21 years of age. The test is comprised of 53 items which are separated into 8 subtests and 4 motor area composites. Subtest scaled scores of 5 or below are considered well-below average, 6–10 are below average, 11–19 are average, 20–24 are above average, and 25 and above are well-above average. Standard scores on the motor area composites range from 20 to 80, with 30 or less defined as well-below average, 31–40 are below average, 41–59 are average, 60–69 are above average, and 70 or greater are well-above average.
2.4 Statistical analysis
Group comparison between treated and untreated children on the motor development domain on the BSID-III was analyzed using a two-tailed t-test at the 5% significance level. Group comparisons were not able to be completed on the other neuromotor and neurological assessments due to small sample sizes when the treated and untreated groups were delineated.
3 RESULTS
3.1 Neurological examination and dysmorphology
Of the subset of boys who were randomly selected for the complete neurological examination, cranial nerves 2–12 were found to be intact in all of the boys and none of them presented with clonus or dysmetria (Table 2). They presented with truncal hypotonia, with hypotonia also evident in their extremities. Eighty-seven percent of the boys presented with decreased or slightly decreased muscle bulk and strength. Deep tendon reflexes (DTRs) were within normal limits at 2+ in 68.85% of boys with 49,XXXXY. Of the subset of 14 boys assessed, response to light touch was intact. Other notable findings were comprised of cardiac murmurs and defect, estropia, increased webbing in the fingers, inverted nipples, head titubations, and ocular motor apraxia (OMA).
| Neurological evaluations in 49,XXXXY | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Patient # | CA yr. Mos | Intact cranial nerves | Fundi not visualized | DTRs | Light touch | Low Oral tone | Truncal Hypotonia | Extremities Hypotonia | Decreased muscle bulk | Decreased muscle strength |
| 1 | 19.9 | + | + | Trace | + | + | + | - | Slight | Slight |
| 2 | 16.0 | + | + | 2+ | + | − | + | − | Slight | Slight |
| 3 | 3.8 | + | + | 2+ | + | − | + | − | Slight | Slight |
| 4 | 1.1 | + | + | 2+ | NE | − | + | + | Slight | Slight |
| 5 | 5.2 | + | + | 2+ | NE | + | + | + | Slight | Slight |
| 6 | 17.11 | + | + | 1–2+ | + | − | + | + | − | − |
| 7 | 1.3 | + | + | 1+ | + | − | + | − | + | + |
| 8 | 4.8 | + | + | 2+ | + | − | + | − | + | + |
| 9 | 4.3 | + | + | 2+ | + | − | + | − | + | + |
| 10 | 25.0 | + | + | 2+ | + | − | + | − | + | + |
| 11 | 14.9 | + | + | 1+ | + | − | + | − | − | − |
| 12 | 2.1 | + | + | 1+ | + | − | + | − | Slight | Slight |
| 13 | 11.6 | + | + | 2+ | + | − | + | − | Slight | Slight |
| 14 | 8.5 | + | + | 2+ | + | − | + | − | + | + |
| 15 | 8.8 | + | + | 2+ | + | − | + | − | + | + |
| 16 | 7.2 | + | + | 2+ | + | − | + | − | + | + |
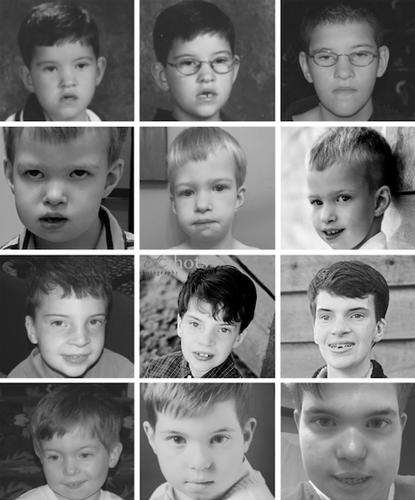
The most common dysmorphic features were epicanthal folds (100%), frontal bossing (87.1%), synophrys (68.18%), upslanting palpebral fissures (57.69%), and hypertelorism (60.61%) (Table 3; Figure 1). Less common features included overfolded helixes, auricular tags, long feet, pectus excavatum, plagiocephaly, thin vermilion, and a broad nasal bridge.
| Dysmorphology features in boys with 49,XXXXY | |||
|---|---|---|---|
| Feature | Number presenting | Total evaluated | Percent present |
| Synophrys | 15 | 22 | 68.18% |
| Arched brows | 18 | 31 | 58.07% |
| Low set ears | 22 | 34 | 64.71% |
| Upslanting palpebral fissures | 15 | 26 | 57.69% |
| Low hanging Columella | 11 | 18 | 61.11% |
| Triangular face | 16 | 25 | 64% |
| Posteriorly rotated ears | 13 | 30 | 43.33% |
| Wide mouth | 24 | 34 | 70.59% |
| Epicanthal folds | 33 | 33 | 100% |
| Smooth philtrum | 7 | 24 | 29.17% |
| Frontal bossing | 27 | 31 | 87.10% |
| Hypertelorism | 20 | 33 | 60.61% |
| Concave nasal ridge | 14 | 27 | 51.85% |
| Dystopia Canthorum | 9 | 20 | 45% |
3.2 Neuromotor capabilities
3.2.1 Preschool
Twenty-eight boys completed the motor development domain of the BSID-III (Table 4). Nine (32.14%) were untreated and 19 (67.86%) received early hormonal treatment (EHT) (Table 5). The mean standard score of the untreated group (CA: 22.89 mos) was 60.22 (SD:13.39) with a range from 46 to 85. The EHT group (CA:22.74) performed significantly better (p = .036), with an average standard score of 72.26 (SD:12.73) and scores ranging from 50 to 100.
| BSID-III psychomotor index scores in treated and untreated boys with 49,XXXXY | ||
|---|---|---|
| Untreated | EHT | |
| N | 9 | 19 |
| Chronological age (months) | 22.89 | 22.74 |
| Mean | 60.22 | 72.26* |
| Median | 58 | 67 |
| Standard deviation | 13.39 | 12.73 |
| Range | 46–85 | 50–100 |
- * Significant at p = 0.036.
| Characteristics of the study population for psychomotor index (n = 28) | |||
|---|---|---|---|
| Participant demographics | Testosterone treatment | No testosterone treatment | |
| Chronological age (Mos) | N | 19 | 9 |
| Mean | 22.74 | 22.89 | |
| Gravida | N | 15 | 7 |
| Mean | 2.2 | 2.43 | |
| Para | N | 11 | 8 |
| Mean | 2.09 | 2.25 | |
| Length of pregnancy | N | 18 | 8 |
| Mean | 38.25 | 38.31 | |
| Maternal age (years) | N | 18 | 8 |
| Mean | 31.59 | 31.13 | |
| Paternal age (years) | N | 18 | 8 |
| Mean | 34.06 | 31.63 | |
| Birthweight (kg) | N | 19 | 8 |
| Mean | 2.39 | 2.52 | |
| Birth length (in) | N | 13 | 5 |
| Mean | 46.56 | 47.75 | |
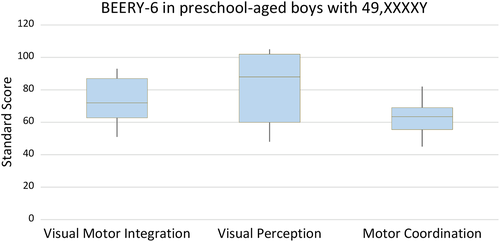
Twelve preschool-aged boys (CA:53.92) completed the BEERY-6 visual motor integration (VMI) subtest (Table 6). Standard scores ranged from 93, which is within normal limits, to 51, which is well below average, and the mean was 72.67. Nine boys completed the visual perception subtest (VP) with an average standard score of 79.67 and a median score of 88 (Figure 2). In motor coordination (MC), the mean standard score of eight boys was 62 and none of the children scored within the normal range.
| BEERY-6 in preschool-aged boys with 49,XXXXY | |||
|---|---|---|---|
| Visual motor integration (VMI) | Visual perception (VP) | Motor coordination (MC) | |
| N | 12 | 9 | 8 |
| Chronological age | 53.92 | 53.89 | 53.13 |
| Mean | 72.67 | 79.67 | 62 |
| Median | 72 | 88 | 63.5 |
| Standard deviation | 14.52 | 21.16 | 11.80 |
| Range | 51–93 | 48–105 | 45–69 |
3.2.2 School-aged
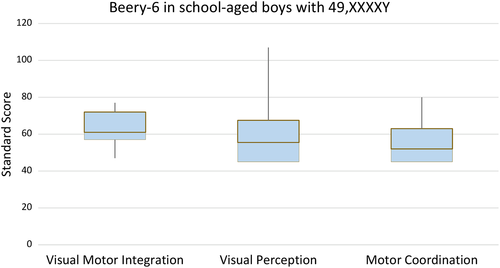
Nineteen school-aged boys completed the BEERY-6 VMI with a mean standard score of 62.9 (SD:9.23) (Table 7). Only 18 of the boys completed the VP and MC domains due to significant dysgraphia and compliance issues. The largest variability in scores was seen in VP, with scores ranging from 107, which is within normal limits, to 45, which is severely compromised (M:55.5). MC was the most depressed with an average standard score of 56.17 (Figure 3).
| BEERY-6 in school-aged boys with 49,XXXXY | |||
|---|---|---|---|
| Visual motor integration (VMI) | Visual perception (VP) | Motor coordination (MC) | |
| N | 19 | 18 | 18 |
| CA | 95 | 96.28 | 97.22 |
| Mean | 62.95 | 58.94 | 56.17 |
| Median | 61 | 55.5 | 52 |
| Std. dev | 9.23 | 16.44 | 11.99 |
| Range | 47–77 | 45–107 | 45–80 |
The BOT-2 was attempted in all school-aged boys. However, due to fatigue, musculoskeletal weakness, and compliance, only nine boys (CA:89 mos) could complete any aspect of the BOT-2 and only four were able to complete the assessment in its entirety (Table 8). All nine boys completed the fine motor control domain and subtests. The mean score was 24 and scores ranged from 20 to 29, which are well-below average. Boys performed better in fine motor integration (M:4) and fine motor precision (M:2). Of the nine children, only four were able to complete the entirety of the BOT-2 (Table 9). The largest range of capabilities was seen in upper limb coordination, with a scaled score of 1 to as high as a scaled score of 12.
| BOT-2 fine motor control scores in boys with 49,XXXXY | ||||||
|---|---|---|---|---|---|---|
| Domain | N | CA | Mean | Median | Standard deviation | Range |
| Fine motor precision | 9 | 89 | 2 | 2 | 1.10 | 1–4 |
| Fine motor integration | 9 | 89 | 4 | 4 | 1.10 | 2–6 |
| Fine motor control | 9 | 89 | 24 | 23 | 3.13 | 20–29 |
| Complete BOT-2 scores in four boys with 49,XXXXY | ||||
|---|---|---|---|---|
| Scores | Patient 1 | Patient 2 | Patient 3 | Patient 4 |
| Manual dexterity | 5 | 5 | 3 | 5 |
| Upper limb coordination | 12 | 7 | 5 | 1 |
| Manual coordination | 34 | 32 | 23 | 25 |
| Bilateral coordination | 4 | 4 | 8 | 1 |
| Balance | 3 | 3 | 3 | 1 |
| Body coordination | 25 | 27 | 30 | 20 |
| Running speed and agility | 3 | 3 | 6 | 1 |
| Strength | 5 | 1 | 7 | 2 |
| Strength and agility | 25 | 20 | 30 | 22 |
| Total motor composite | 23 | 23 | 23 | 20 |
Grip strength was evaluated on a subset of boys (n = 18) between the ages of 72 and 143 months (Table 10). Grip strength at every age was depressed compared to neurotypical boys in both the right and left hands (McQuiddy, Scheerer, Lavalley, McGrath, & Lin, 2015).
| 49,XXXXY | Neurotypical malesa | |||||
|---|---|---|---|---|---|---|
| Age (yrs) | Hand | N | Mean (kg) | SD (kg) | Mean (kg) | SD (kg) |
| 6 | R | 5 | 3.27 | 1.78 | 9.6 | 2.7 |
| L | 1.99 | 1.87 | 8.8 | 2.2 | ||
| 7 | R | 2 | 4.77 | 0.23 | 11.7 | 3.0 |
| L | 2.95 | 0.23 | 10.8 | 3.0 | ||
| 8 | R | 3 | 4.39 | 0.22 | 13.9 | 2.8 |
| L | 5.44 | 2.67 | 12.9 | 2.4 | ||
| 9 | R | 2 | 5.89 | 2.27 | 15.2 | 3.7 |
| L | 3.18 | 0 | 14.0 | 3.1 | ||
| 10 | R | 3 | 6.95 | 2.99 | 17.4 | 4.1 |
| L | 5.59 | 4.29 | 15.8 | 3.3 | ||
| 11 | R | 3 | 10.59 | 3.36 | 20.9 | 4.4 |
| L | 8.77 | 5.19 | 19.3 | 4.3 | ||
| 12 | R | 5 | 6.26 | 3.07 | 23.5 | 4.4 |
| L | 6.17 | 3.37 | 21.2 | 4.0 | ||
| 13 | R | 3 | 13.91 | 6.63 | 27.1 | 7.0 |
| L | 13.61 | 6.32 | 24.4 | 6.5 | ||
| 15 | R | 1 | 22.22 | — | 33.5 | 9.3 |
| L | 18.14 | — | 30.9 | 8.2 | ||
| 16 | R | 3 | 11.94 | 3.36 | 39.8 | 8.6 |
| L | 9.83 | 5.95 | 37.5 | 8.1 | ||
| 17 | R | 1 | 20.4 | — | 42.9 | 8.3 |
| L | 17.69 | — | 42.9 | 8.5 | ||
| 19 | R | 1 | 19.05 | — | 45.5 | 8.8 |
| L | 17.69 | — | 41.9 | 9.3 | ||
- a McQuiddy et al. (2015).
3.2.3 Adolescence
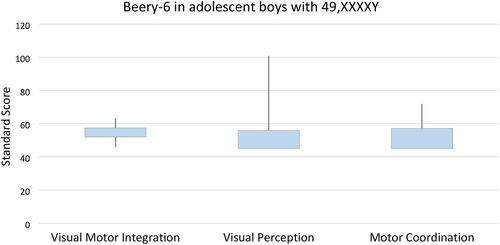
Eight adolescent boys with 49,XXXXY (CA:156.38 mos) were evaluated with the BEERY-6 (Table 11). In the VMI, the mean standard score was 52.38, which is moderately impaired. In VP, standard scores varied significantly, ranging from 101 to 45, with a mean of 56.5 (Figure 4). In MC the average standard score was 51.5, with none of the standard scores within the average range, which is consistent with preschool and school age performance on this subtest. These results support the presence of dysgraphia in these boys.
| Beery-6 in adolescent boys with 49,XXXXY | |||
|---|---|---|---|
| Visual motor integration (VMI) | Visual perception (VP) | Motor coordination (MC) | |
| N | 8 | 8 | 8 |
| CA | 156.38 | 156.38 | 156.38 |
| Mean | 52.38 | 56.5 | 51.5 |
| Median | 52 | 45 | 45 |
| Std. dev | 6.42 | 19.74 | 9.38 |
| Range | 45–63 | 45–101 | 45–72 |
Grip strength was assessed in 14 adolescent boys with 49,XXXXY between the ages of 144 months (12 years) and 230 months (19.17 years) (Table 10). All boys were well-below average on grip strength in both hands when compared to the neurotypical normative values for the corresponding ages.
4 DISCUSSION
This study describes an in depth investigation of the neurologic function, neuromotor skills, and the dysmorphology of the largest population of boys with 49,XXXXY to date. Dysmorphic features in this cohort were consistent with previous reports, however several novel features were noted. Epicanthal folds (100%) and frontal bossing (87.1%) were extremely common with high incidences of upslanting palpebral fissures, low set and posteriorally rotated ears, synophrys, and hypertelorism. Novel dysmorphic features included smooth philtrum (29.17%), low hanging columella (61.11%), and dystopia canthorum (45%). Many parents reported that the chromosomal testing was initiated in the newborn period to rule out Trisomy 21 (Down syndrome), which would be consistent with some of the more common dysmorphic features that were noted.
Neurological assessment demonstrated intact cranial nerves and sensory modalities to light touch and pinprick in 100% of those assessed. Cranial nerves were evaluated due to their vital role in determining neurological integrity. Our results indicate that the etiology of the neurodevelopmental delays seen in this disorder are derived from a generalized central nervous dysfunction rather than specific deficits in cranial nerves. All boys with 49,XXXXY presented with truncal hypotonia and the majority presented with at least slightly decreased muscle bulk and strength regardless of their age which ranged from infancy through adolescence. These findings are consistent with previous case reports on the disorder demonstrating that neuromotor dysfunction is a characteristic feature of the phenotypic presentation in 49,XXXXY.
The abnormal muscle tonus is associated with increased incidences of gross and fine motor delays evident as early as 4 months of age and throughout life. Hypotonia and decreased strength are impactful on every domain of development. Hypotonia with the subsequent fatigue also impacted on whether boys with 49,XXXXY could complete the gross motor evaluation, thus explaining why more boys completed the less strenuous fine motor tasks than the gross motor items. The moderate hypotonia is a significant factor in the consistently below average scores on balance, running speed and agility, and strength. Based on these comprehensive findings, boys with 49,XXXXY would benefit from long-term, consistent physical therapy services, ideally with pediatric providers who are experienced with children who have neurogenetic disabilities.
This study has also described the variable neuromotor development in the boy with 49,XXXXY. The widest range of capabilities were observed on the BOT-2 in manual coordination and upper limb coordination (ULC) from well below average to average scores. The ULC subtest requires a child to dribble, catch, and throw a tennis ball in multiple tasks. Some of the variation of scores seen in this subtest may be due to the presence of radioulnar synostosis (RUS), which is a documented part of the 49,XXXXY phenotype (Burgemeister et al., 2019; Curfs et al., 1990; Martini et al., 1993; Rehder, Fraccaro, Cuoco, Gimelli, & Porro, 1986; Sprouse et al., 2013; Tosi et al., 2020). RUS and the associated restrictions in supination and pronation of the elbow may impact activities of daily living (ADL) and tasks that require refined and controlled movements for throwing and catching a ball. Of the four boys with 49,XXXXY who completed the ULC subtest, three presented with documented RUS. However, there may be other reasons for the variability observed in these motor capabilities. While patient one had the highest score and limited RUS, patient two had the most severe RUS and yet had the second highest score in ULC. Further study is necessary to delineate the relationship between RUS, acquisition of neurodevelopmental skills and ADL skills in order to optimize the outcome in the child with 49,XXXXY and minimize the possible impact of RUS.
The variability of scores was also apparent on the BEERY-6, with VP revealing a consistent pattern of mildly impaired but more preserved in comparison with MC, which was the lowest area of function. This profile is similar but more severely affected than boys with 47,XXY. Typically, the boys with 47,XXY demonstrate average to above average capabilities in visual perception and low to below average scores in motor coordination (Lasutschinkow, Gropman, Sadeghin, & Samango-Sprouse, 2019). This pattern of performance is consistent with the presence of dysgraphia in both disorders.
Findings of decreased hand strength were noted in the neurological assessment and standardized testing on grip strength. The grip strength in 16-year-old boys with 49,XXXXY matched the average strength in neurotypical boys at 7 years of age. These deficits are extremely impactful on the development of ADLs such as dressing, eating and toileting and later in life for work employment for these boys whether independent or supervised. Depressed grip strength is also indicative of decreased muscle and forearm strength. Further research is needed to identify whether this decreased grip strength is the primary result of the hypotonia, a possible interaction of RUS and hypotonia, or if there are additional factors impacting the development of hand strength. Boys with 49,XXXXY would benefit from occupational therapy services starting in preschool and continuing throughout school age for these deficiencies.
Previous studies for more than 20 years have been associated with improvements in neurodevelopment upon implementation of testosterone treatment in boys with extra X chromosomes at various ages (Lanfranco, Kamischke, Zitzmann, & Nieschlag, 2004; Patwardhan, Eliez, Bender, Linden, & Reiss, 2000; Samango-Sprouse et al., 2011; Samango-Sprouse et al., 2013; Tran, Samango-Sprouse, Sadeghin, Powell, & Gropman, 2019). The relationship between biological treatment and neurodevelopment improvement is not well understood, but the importance of androgen to the health and well-being of all males is well recognized (Arnold & Breedlove, 1985; Chura et al., 2010; Harman, Metter, Tobin, Pearson, & Blackman, 2001; Perrin et al., 2008). Therefore, this study explored the potential impact of early hormonal treatment on neuromotor capabilities in boys with 49,XXXXY. While both the untreated and treated groups of young boys demonstrated expected well-below average motor development, the testosterone treated group had significantly increased scores when compared to the untreated group (p = .036) on the BSID-III Psychomotor Development Index. This investigation, coupled with previous research publications, has supported the positive impact on neurodevelopment associated with hormonal replacement in boys with 49,XXXXY. Therefore, hormonal replacement should be considered as one aspect of their individualized care that may optimize their neurodevelopmental outcome when given in infancy and in tandem with early intervention services.
There was significant variance in standard scores on multiple tests throughout this study. The variability in performance is a very characteristic feature of all boys with additive X chromosomes. Many causes for this variance have been hypothesized from the origin of the additive X, dosage effect and familial history of learning dysfunction and/or mental health issues. Additionally, the existence of mosaicism may explain some of the variance within this disorder and a limitation of this study is that the presence or absence of mosaicism was only confirmed via chromosome analysis in 17% of the research population. Further research is underway to confirm the incidence of mosaicism in boys with 49,XXXXY and its subsequent relationship to neurodevelopmental outcome.
This comprehensive study has further expanded the dysmorphic and neurological profile of this disorder in a large, well-described cohort of males with 49,XXXXY. This investigation has further identified preserved visual perception function in comparison to motor coordination skills and demonstrated a positive association between EHT and improvement in neuromotor skills on the BSID-III. 49,XXXXY is a complex disorder and more investigations are warranted to identify salient factors that may be impacting the variance in neurodevelopment in all children with X and Y chromosomal variations.
ACKNOWLEDGMENTS
We would like to express our deep gratitude to all of our participants and their families, as well as The Focus Foundation for their continued support of our research. The authors declare no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.