Calvarial mass as a presenting feature of neurofibromatosis type 2 in a pediatric patient
To the Editor:
A 10-year-old boy was evaluated for a large, painless mass on the left parietal aspect of his skull. A CT scan revealed a complex mass that appeared to arise from the bone (Figure 1a), which was concerning for a primary sarcoma given extensive periosteal reaction. A subsequent MRI showed a large 10.8 × 6.2 × 9.3 cm mass centered in the left parietal bone with both extra-axial intracranial and extracalvarial components (Figure 1b). The intracranial component of the tumor caused mass effect on the subjacent brain parenchyma, which was associated with marked edema (Figure 1c). In addition to the large calvarial mass, MR imaging also revealed a second dural-based lesion at the level of the foramen magnum anteriorly and enhancing lesions within the internal auditory canals (Figures 1d and 1e) and right prepontine cistern. A spine MRI showed additional enhancing lesions in the conus medullaris and sacral region (Figure 1f). The differential diagnosis consisted of a primary sarcoma with metastatic disease versus an intraosseous meningioma with disparate neoplasms as seen in the setting of neurofibromatosis type 2 (NF2).
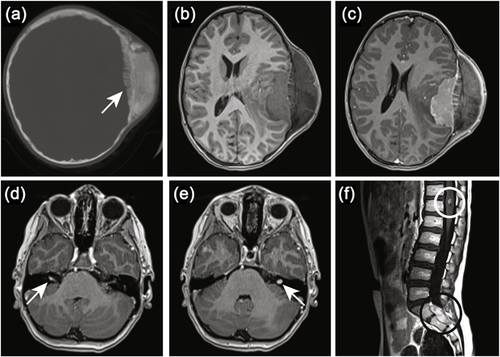
The favored diagnosis was an intraosseous meningioma in the setting of NF2 given the patient's indolent course, the presence of bilateral vestibular schwannomas and multiple other lesions, and an additional history of a cataract in early childhood. Although the patient met clinical criteria for NF2, there was residual concern for the possibility of a metastatic sarcoma based on the initial concern raised by CT imaging. The surgical approach for a sarcoma would have been to do an upfront biopsy followed by neoadjuvant chemotherapy. The surgical approach for an intraosseous meningioma would have been to avoid an upfront biopsy due to bleeding risk and proceed with embolization and subsequent resection. As the patient's presentation was quite unusual, it was decided to prove that the sacral mass did not represent metastatic sarcoma before proceeding to definitive management of the primary mass. Pathology of the sacral mass was consistent with a schwannoma, which virtually ensured an underlying NF2 diagnosis. The patient therefore underwent embolization of the suspected intraosseous meningioma followed by resection. Pathology confirmed a diagnosis of intraosseous meningioma, WHO grade I. The patient is now 18 months post-surgery with no evidence of disease recurrence. Genetic testing returned following surgery and verified a heterozygous truncating mutation in the NF2 gene (NF2 NM_016418.5:c.1021C>T p.Arg341Ter).
This case illustrates an unusual presentation of NF2. NF2 is a cancer predisposition syndrome characterized by bilateral vestibular schwannomas and other neoplasms impacting the brain and spine including meningiomas, schwannomas, and ependymomas. It is an autosomal dominant disorder resulting from inactivating mutations of the NF2 tumor suppressor gene. The disease normally presents in the early 20s with hearing loss or other neurologic deficits including problems with balance, visual deficits, or numbness/weakness of extremities. Meningiomas occur in about 70% of NF2 patients and are usually asymptomatic (Evers, Verbaan, Sanchez, & Peerdeman, 2015; Nowak, Dziedzic, Czernicki, Kunert, & Marchel, 2015; Smith et al., 2011). Truncating mutations in the NF2 gene are associated with early-onset of disease and an increased number of meningiomas and spinal tumors (Ruggieri, Pratico, & Evans, 2015). Intraosseus meningiomas are quite rare, and they are virtually never present in newly diagnosed NF2. This case highlights a dramatic presentation of NF2 and reveals how careful analysis of radiology images can lead to the diagnosis of an underlying cancer predisposition syndrome.